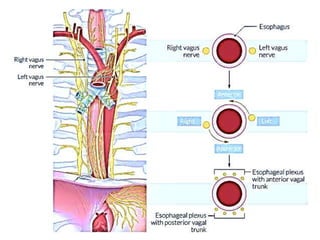
This document provides an overview of gastric perforation. It begins with an introduction defining gastric perforation and noting the decrease in incidence due to treatment of H. pylori and acid hypersecretion. It then covers the anatomy of the stomach, etiologies of perforation including peptic ulcer disease, signs and symptoms, investigations like abdominal x-rays, and surgical management including repair techniques like omentoplasty and reconstructions like Billroth procedures. Post-operative complications are also discussed such as leakage, strictures, and syndromes. The role of vagotomy and drainage procedures is reviewed.