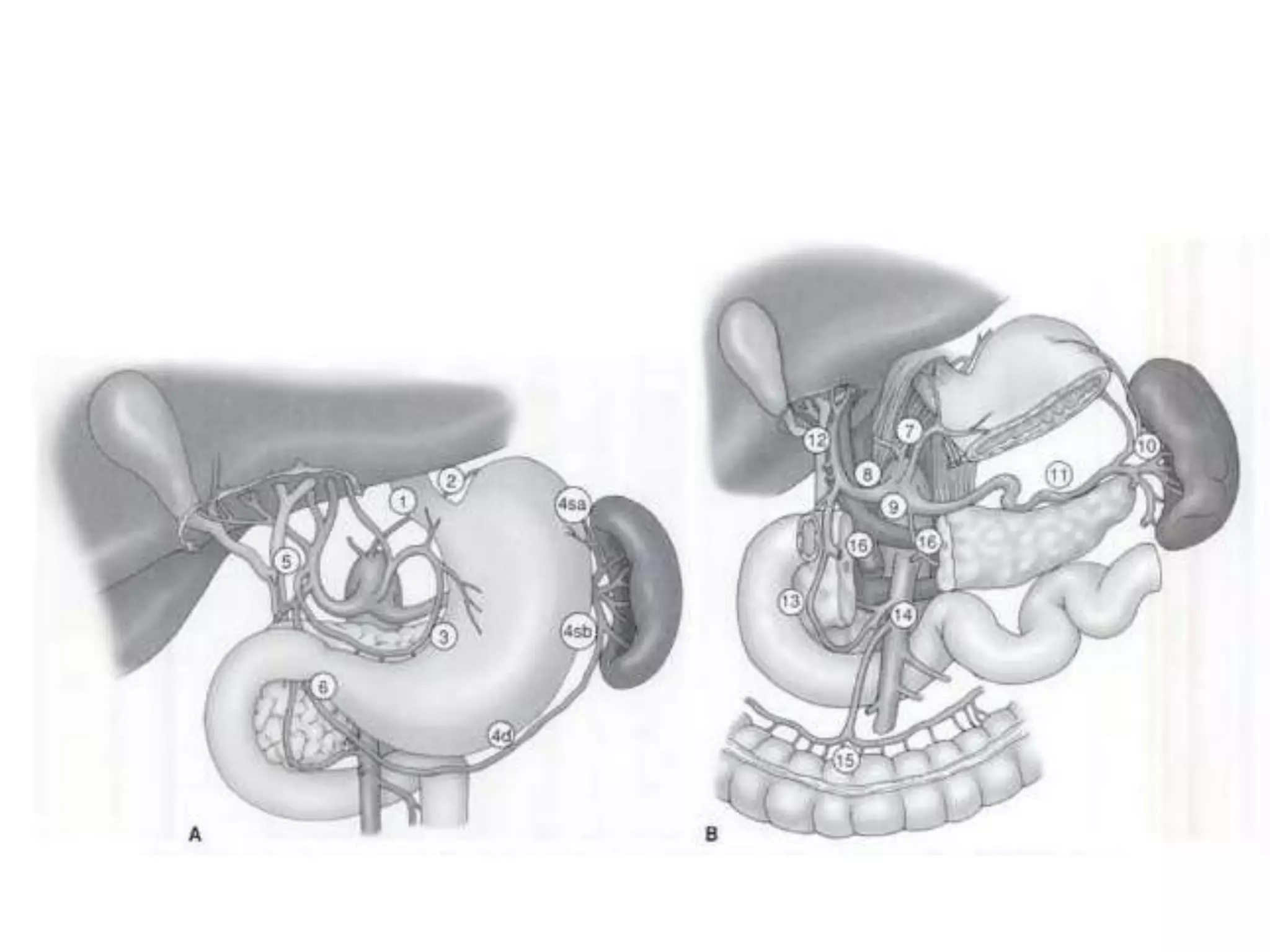
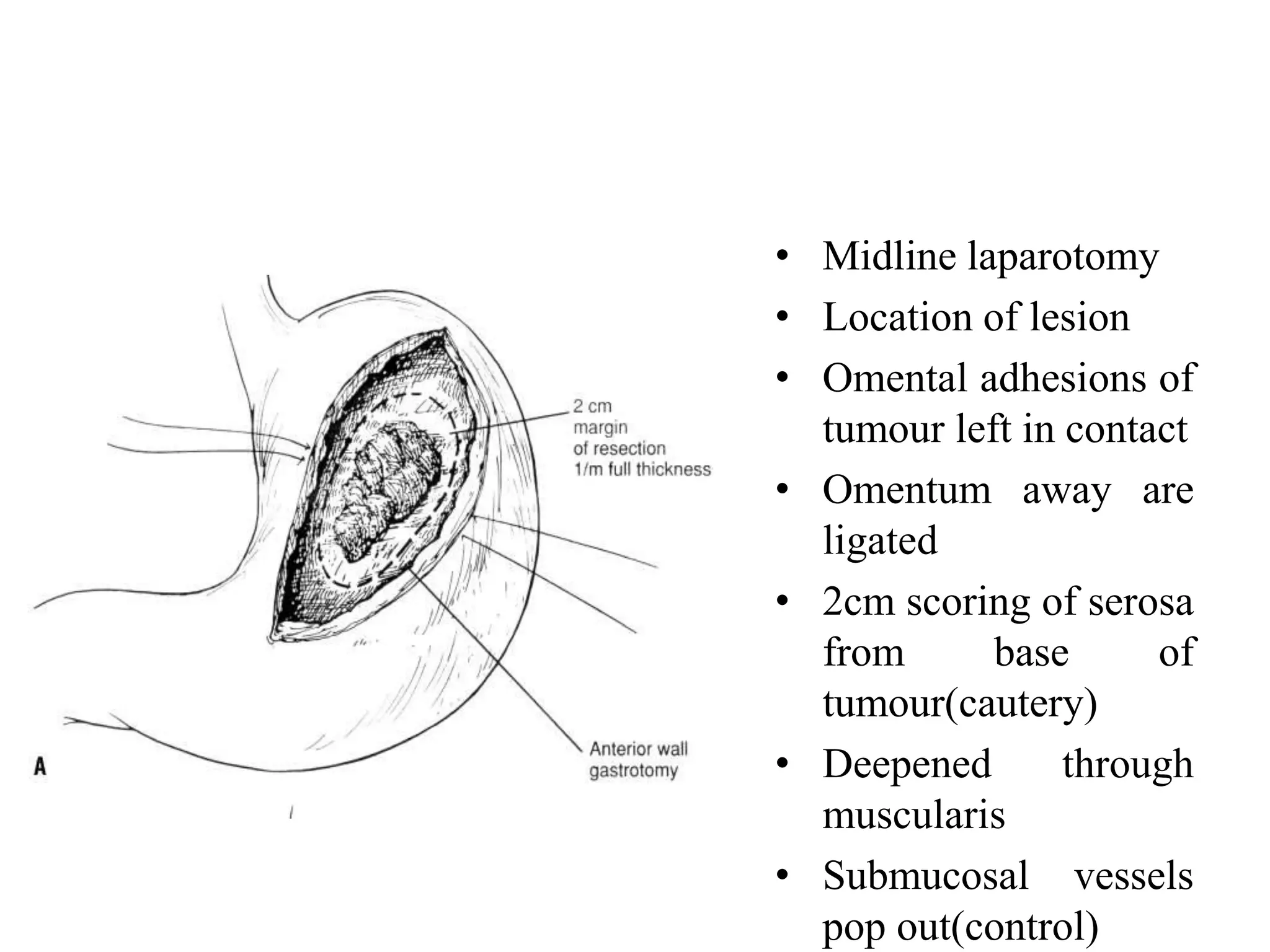
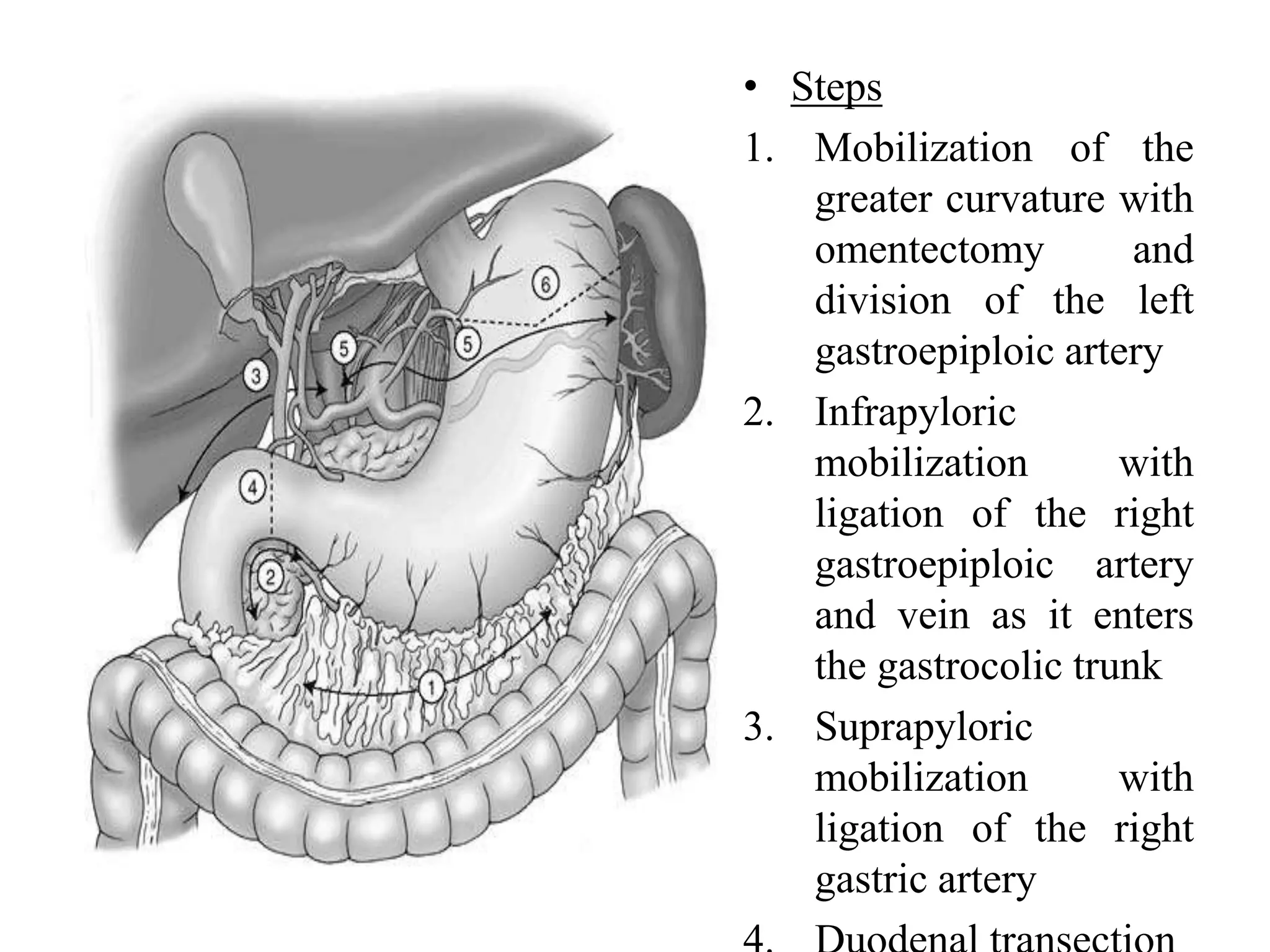
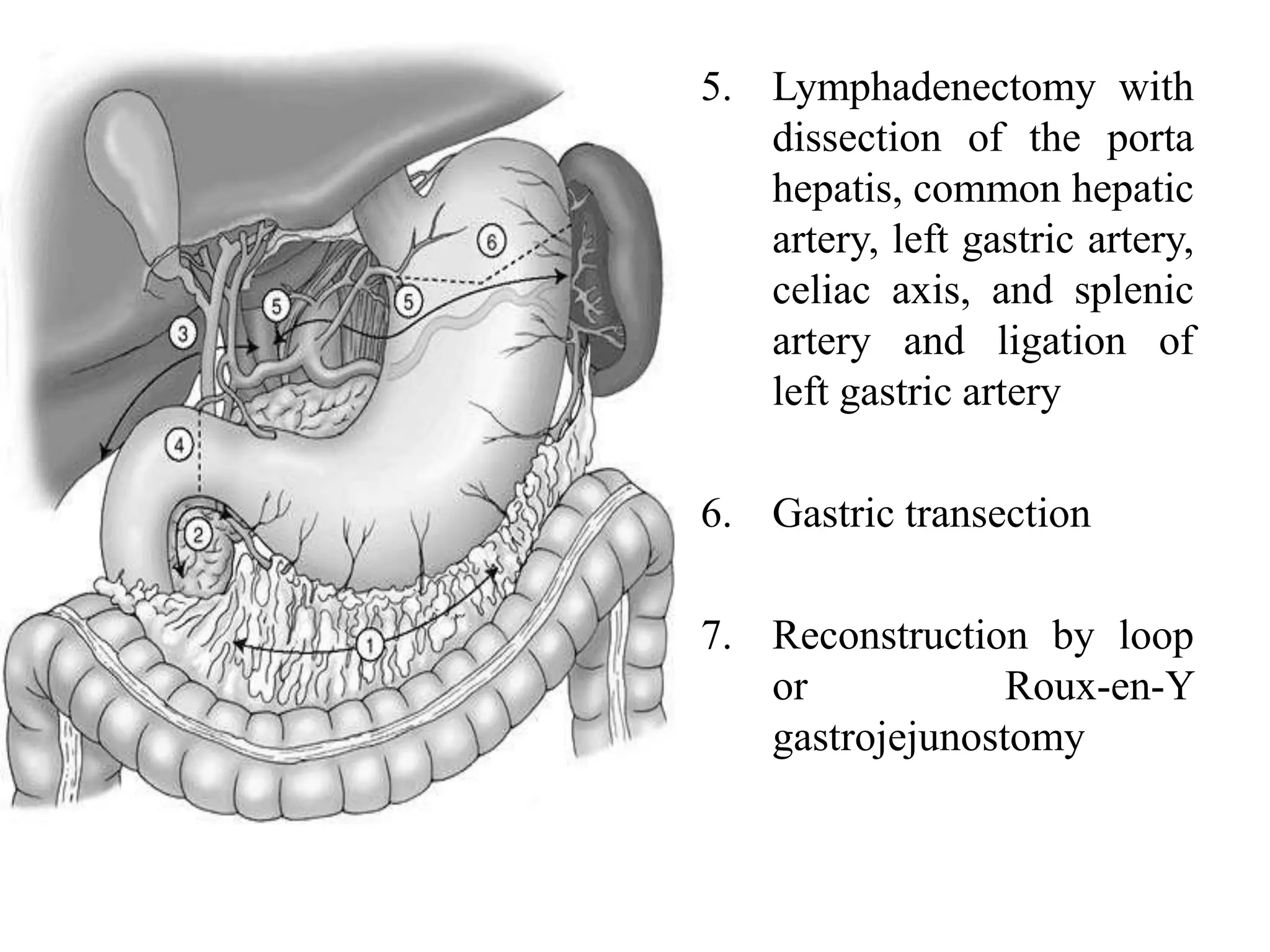
This document provides information on different types of gastric resection surgeries including wedge resection, distal gastrectomy, total gastrectomy, and subtotal gastrectomy. It describes the anatomy of the stomach and surrounding structures. It details the surgical techniques for each type of resection including mobilization, resection, and reconstruction. Common indications for gastric resections are described as peptic ulcer disease and gastric tumors. The history of developments in gastric surgery techniques from the late 19th century onward is also summarized.