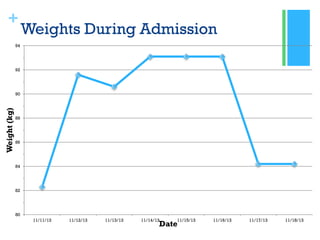
Chronic pancreatitis is a long-term inflammation of the pancreas that results in permanent damage. The patient, AH, underwent a Whipple procedure for chronic pancreatitis caused by hypertriglyceridemia and possible bile duct stones. Over her 7 day hospital stay, AH's diet was advanced from NPO to regular meals. She was educated on GI and diabetes diets and discharged tolerating a regular diet.