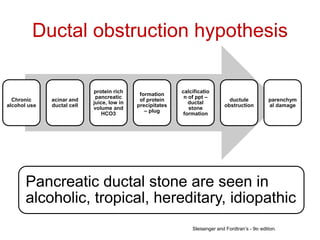
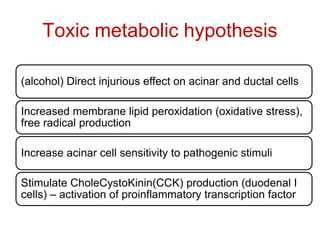
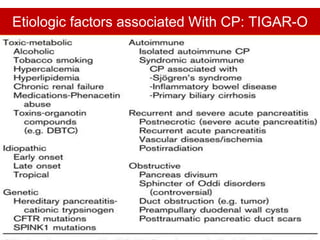
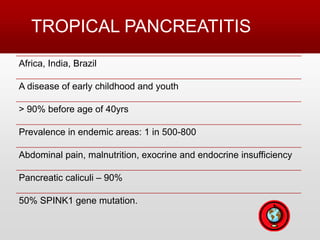
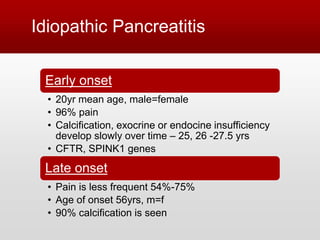
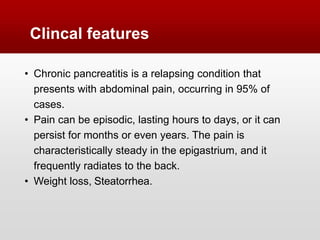
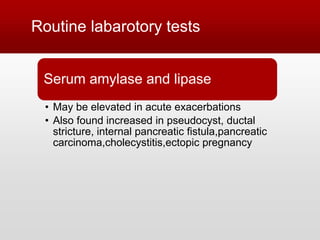
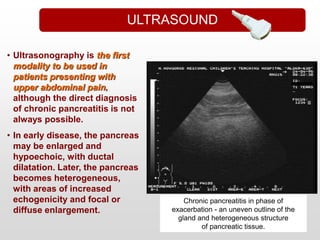
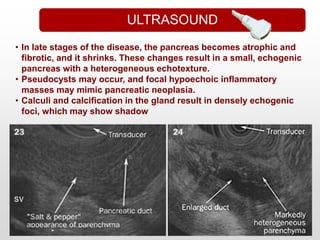
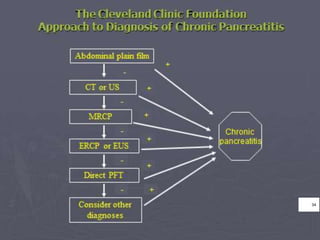
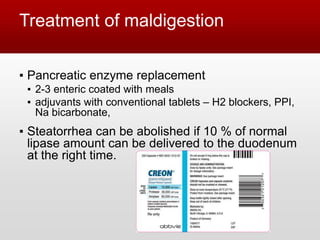
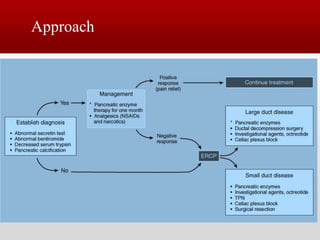
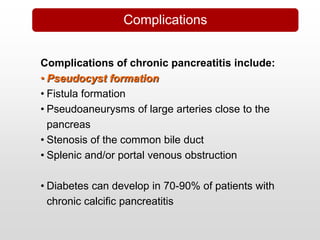
This document provides an overview of chronic pancreatitis, including its pathophysiology, etiology, clinical features, diagnosis, and management. It discusses how chronic pancreatitis represents a continuous inflammatory and fibrosing process of the pancreas resulting in permanent dysfunction. The main causes are alcohol use and genetic factors. Patients present with abdominal pain in 95% of cases and can develop weight loss, steatorrhea, and diabetes. Diagnosis involves tests of pancreatic function and imaging tests looking for features like calcification. Treatment focuses on pain control, managing maldigestion with pancreatic enzyme replacement, and addressing complications like pseudocysts and stenosis.