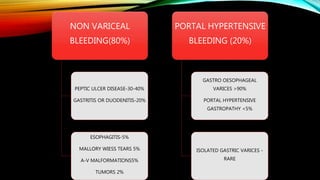
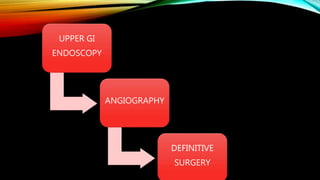
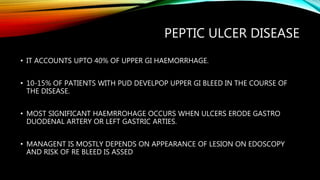
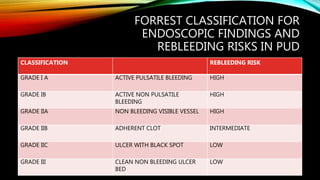
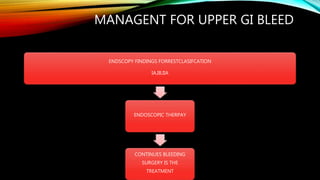
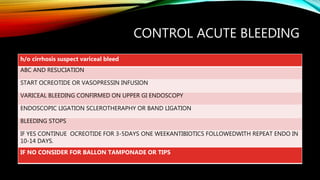
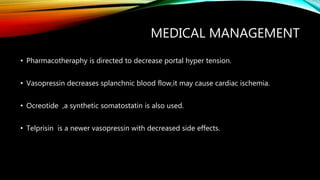
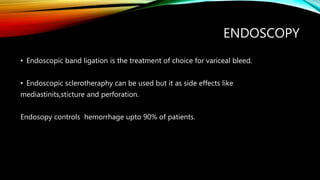
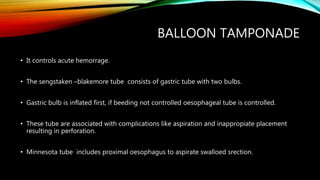
Upper GI bleeding refers to bleeding from the GI tract proximal to the ligament of Trietz. Non-variceal bleeding accounts for 80% of cases, with peptic ulcer disease being the most common cause at 30-40%. Portal hypertensive bleeding from gastroesophageal varices accounts for the remaining 20% of cases. Early endoscopy within 24 hours of bleeding results in reduced transfusions, decreased need for surgery, and shorter hospital stays. Endoscopic therapies like epinephrine injection and thermal coagulation are effective first-line treatments for actively bleeding ulcers. Surgery is indicated if bleeding cannot be controlled or for recurrent bleeding. Variceal bleeding requires resuscitation, vasoactive drugs, and endoscopic