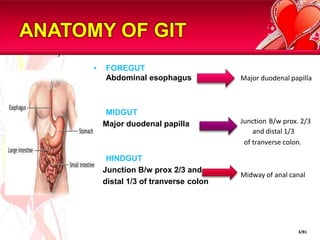
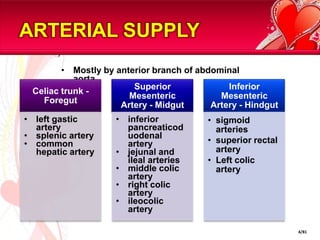
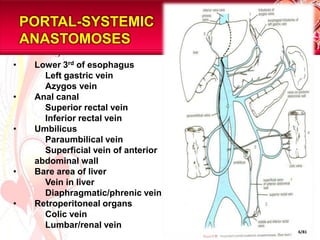
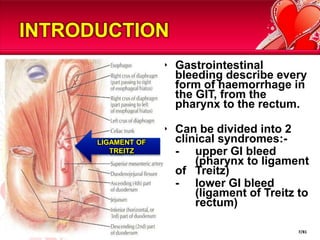
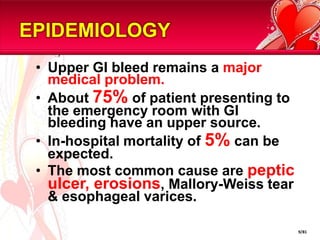
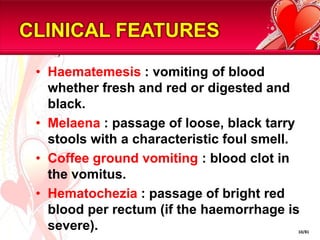
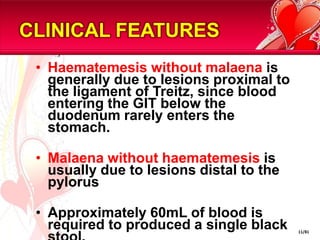
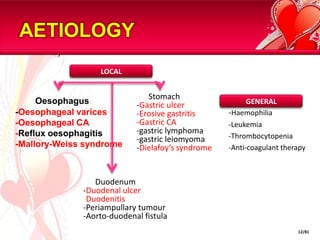
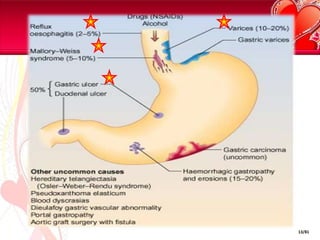
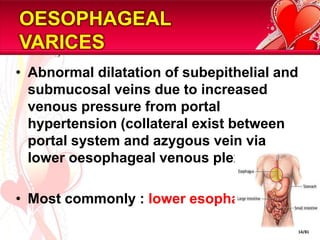
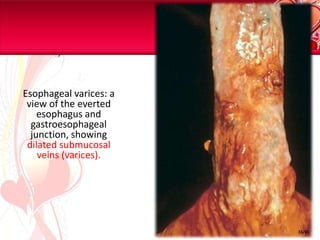
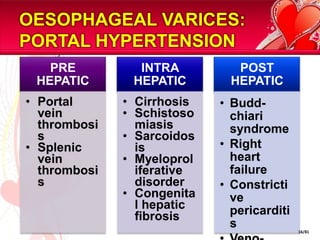
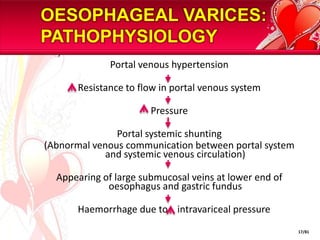
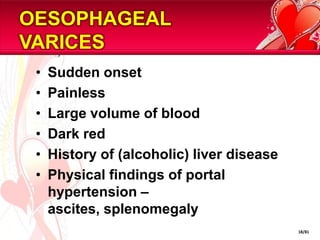
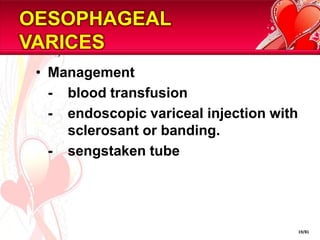
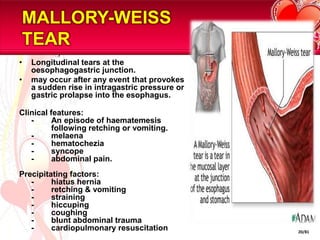
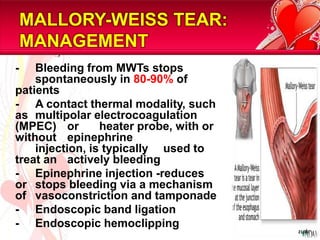
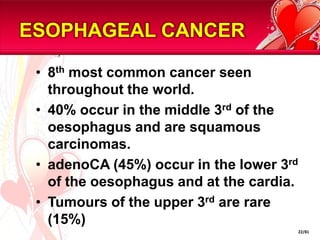
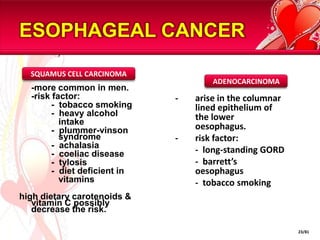
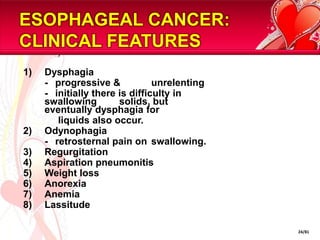
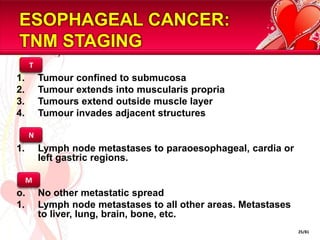
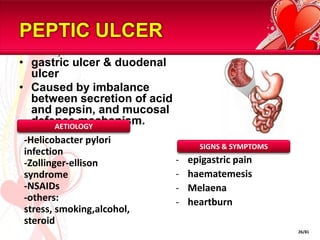
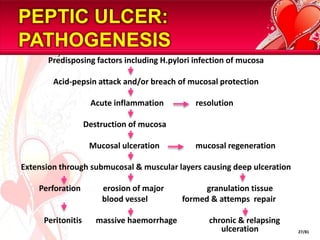
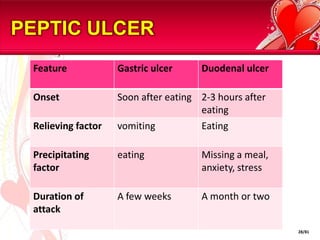
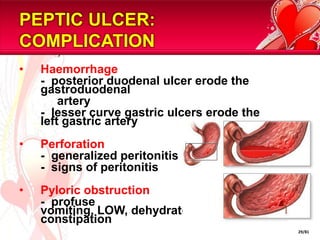
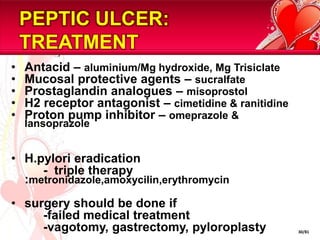
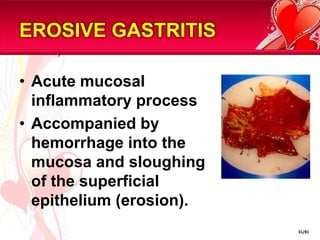
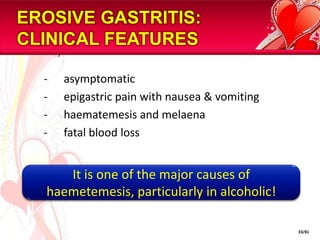
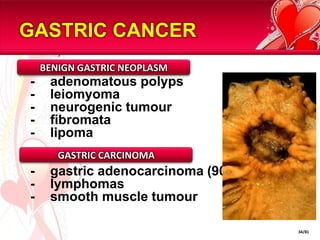
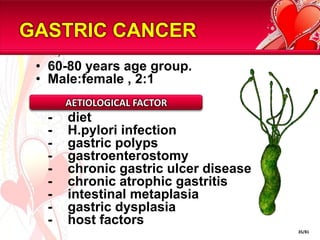
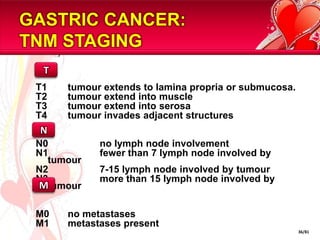
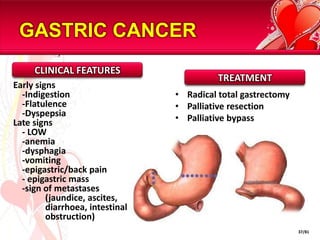
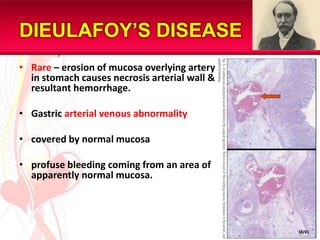
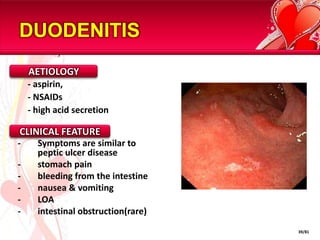
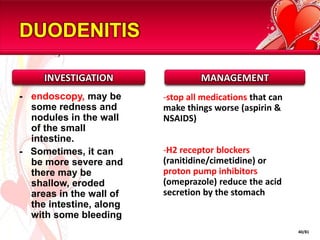
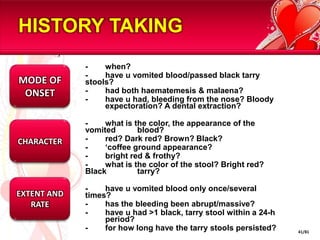
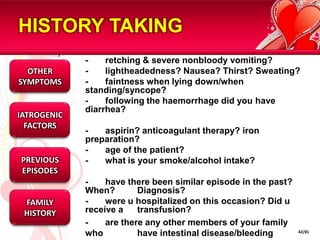
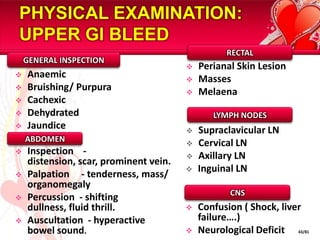
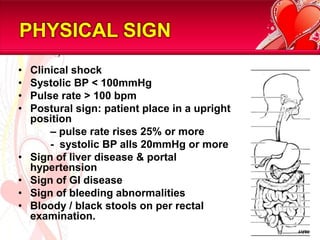
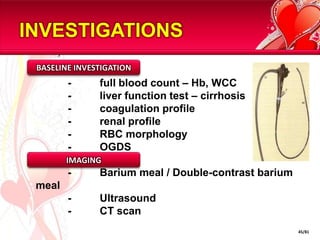
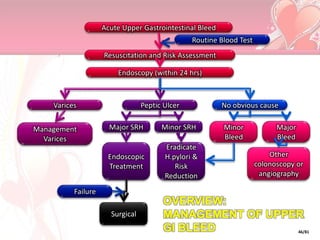
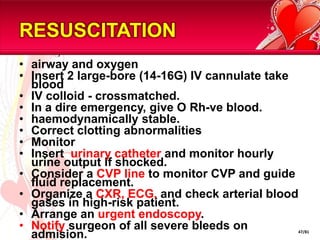
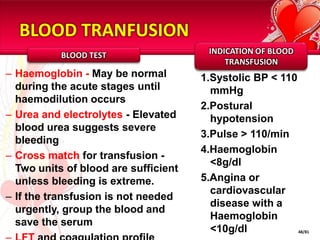
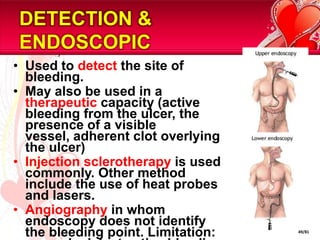
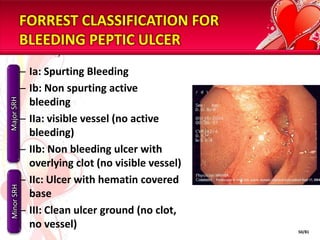
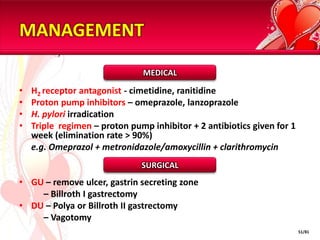
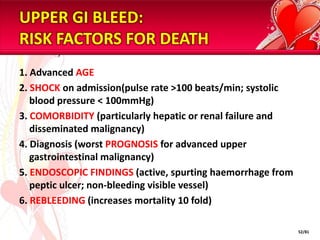
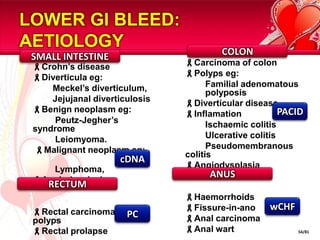
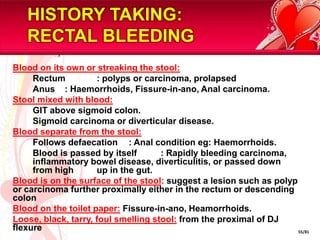
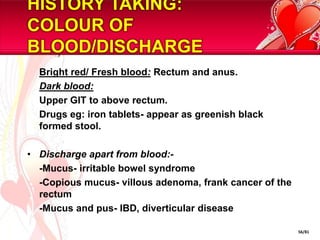
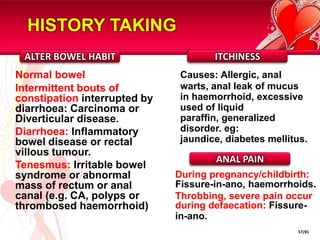
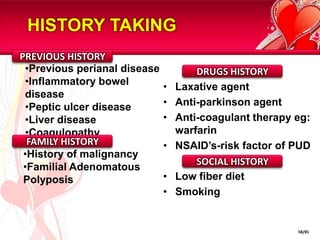
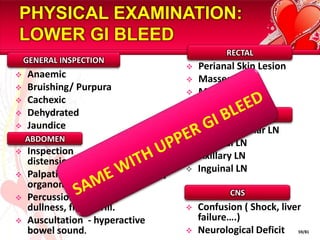
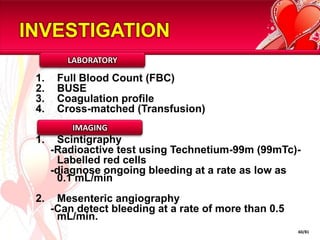
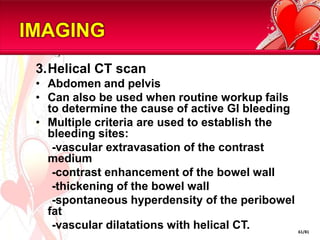
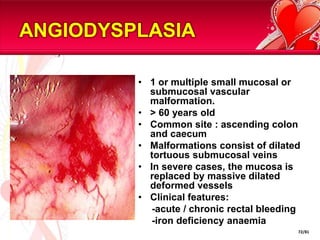
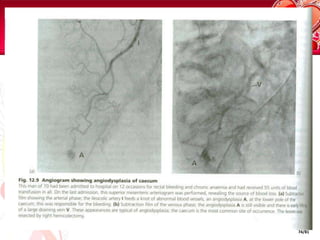
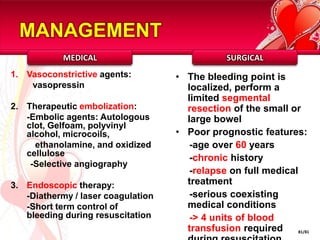
This document provides information on gastrointestinal bleeding, including its anatomy, definition, epidemiology, clinical features, etiology, history and examination, investigation, and management. It discusses the major sites of upper and lower GI bleeding. For upper GI bleeding it covers topics such as esophageal varices, Mallory-Weiss tears, esophageal cancer, peptic ulcer disease, erosive gastritis, gastric cancer, and Dieulafoy's disease. For lower GI bleeding it briefly mentions duodenitis. It provides details on the pathogenesis, clinical presentation, investigations and treatment of many of these conditions.