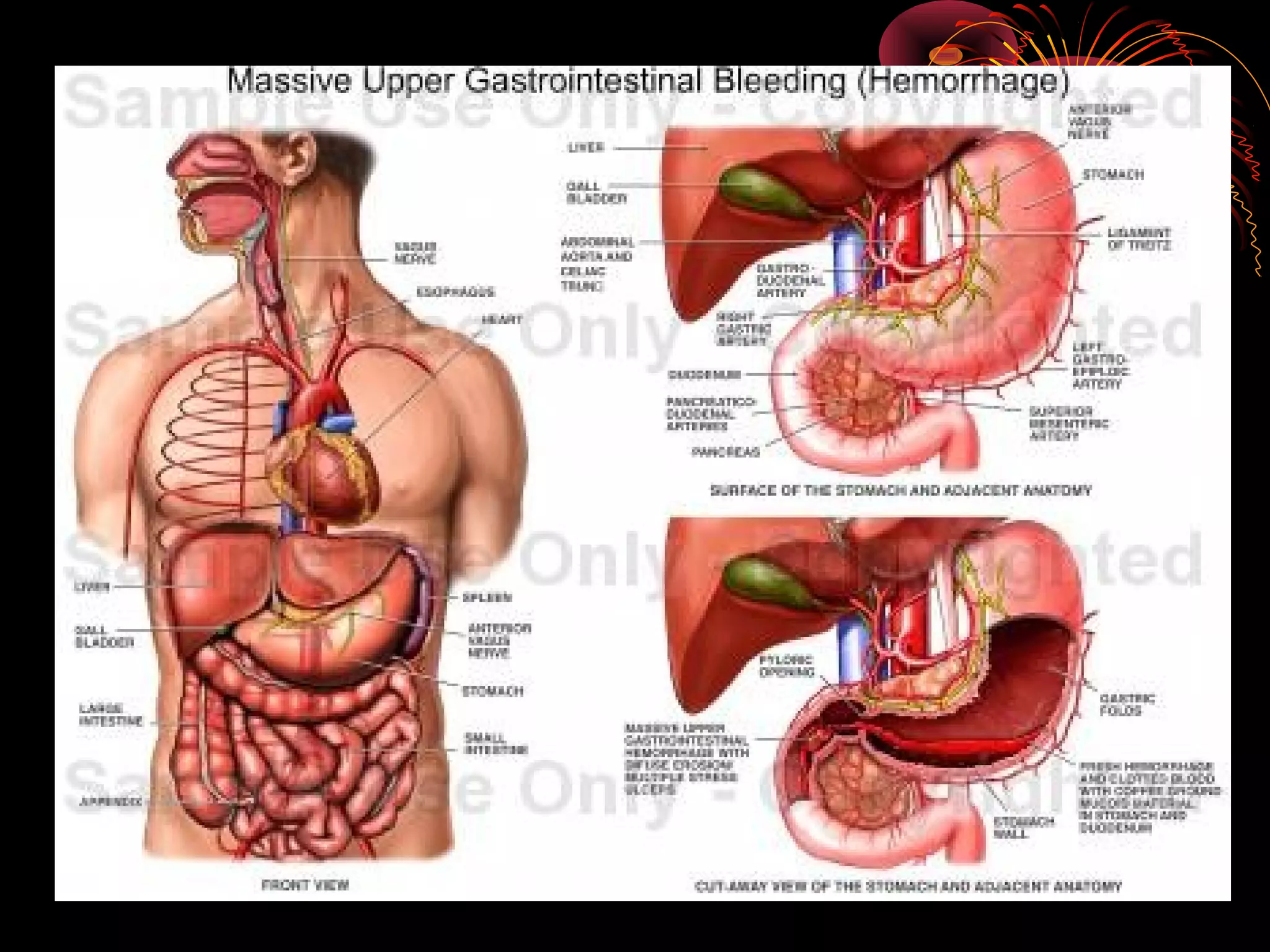
UGIB can be defined as bleeding from the gastrointestinal tract above the ligament of Treitz. The most common causes are peptic ulcers, varices, and Mallory-Weiss tears. Presentation includes hematemesis, melena, hematochezia, or signs of blood loss. Management involves resuscitation, endoscopic diagnosis and treatment such as band ligation or coagulation, and drug therapy like PPIs or vasoconstrictors. Prognosis depends on age, comorbidities, signs of shock, and rebleeding risk.


![Aetiology (contd)
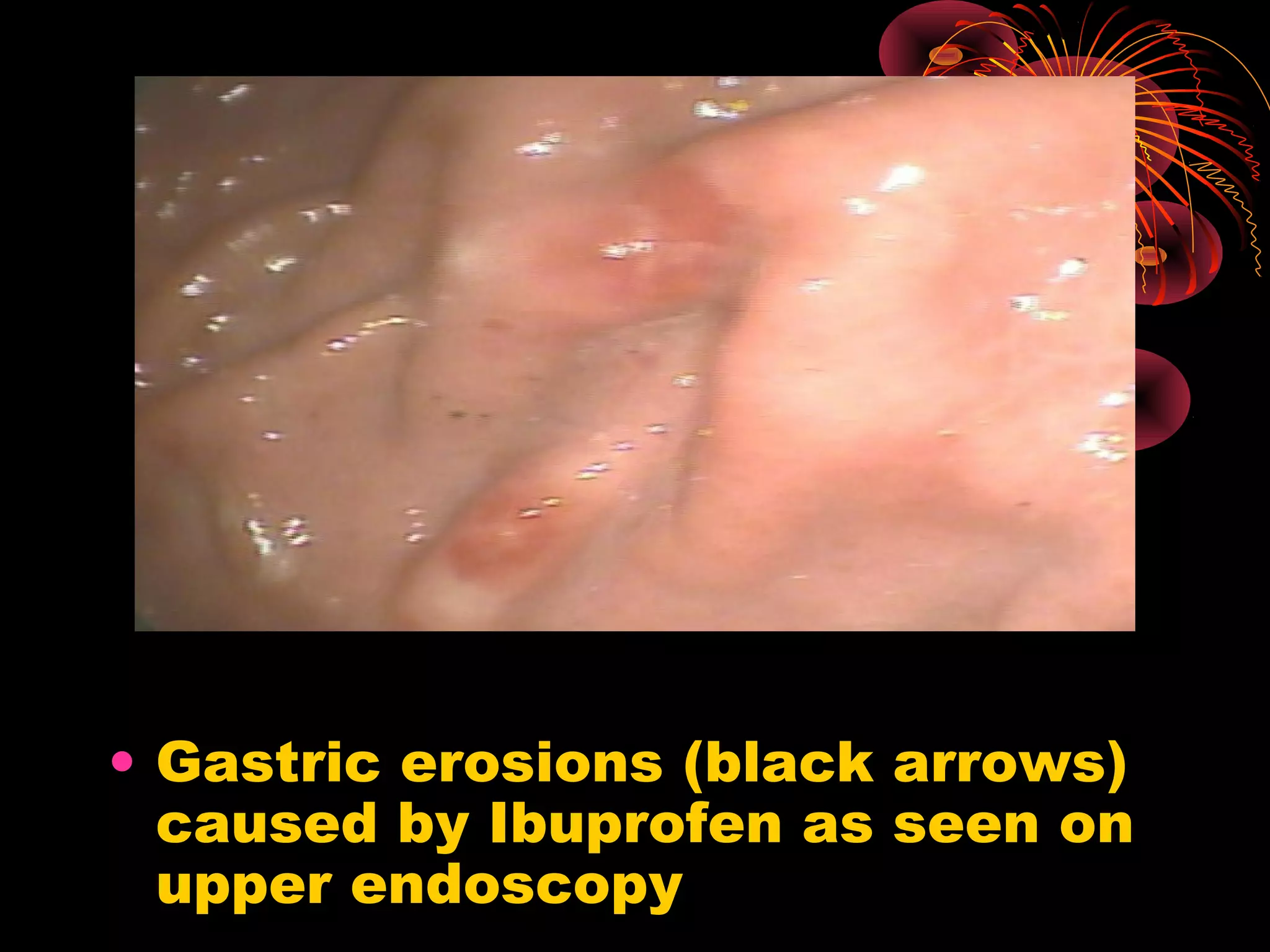
• Uncommon causes; they include Erosive
duodenitis, neoplasms, aortoenteric
fistulas, vascular lesions[ including
hereditary haemorrhagic
telengectasias(Osler- Weber-Rendu) and
gastric antral vascular ectasia (‘Water-
melon stomach’)], Dieulafoy’s lesion (in
which an aberrant vessel in the mucosa
bleeds from a pinpoint mucosal defect),
prolapse gastropathy, haemobilia and
hemosuccus pancreaticus.](https://image.slidesharecdn.com/uppergastrointestinaltractbleedingugib-121216160207-phpapp01/75/Upper-gastrointestinal-tract-bleeding-ugib-7-2048.jpg)