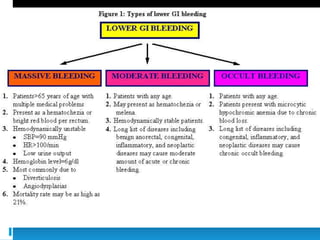
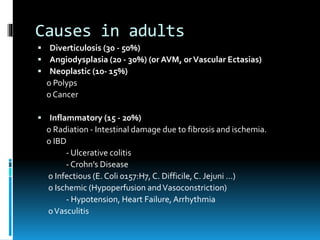
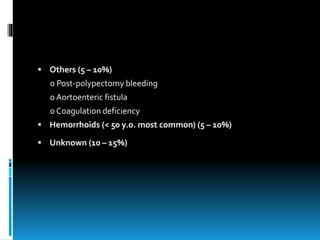
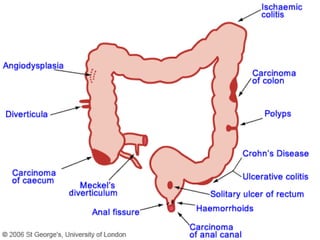
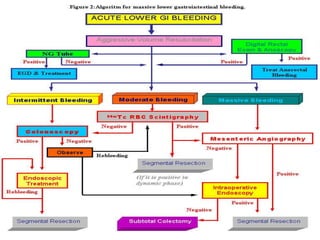
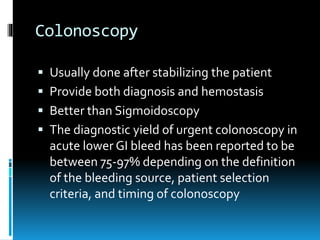
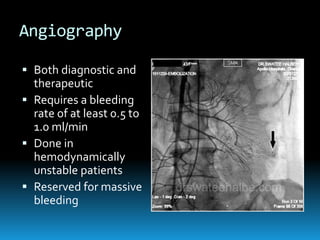
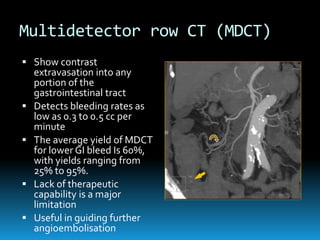
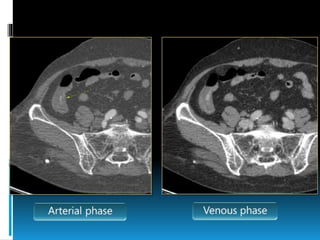
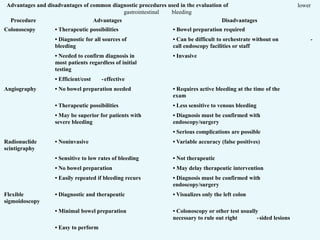
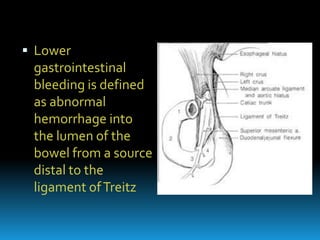
Lower gastrointestinal bleeding can have various causes like diverticulosis, angiodysplasia, inflammation, and cancers. A thorough history, physical exam, and initial tests like colonoscopy are important to determine the source and severity of bleeding. Colonoscopy allows for both diagnosis and potential treatment but often requires bowel prep, while angiography and CT angiography can localize active bleeding but lack therapeutic options. Together, these diagnostic tests aim to safely identify the cause and guide appropriate clinical management of lower GI bleeding.
![Epidemiology
Overall mortality <5%. [Frequency and
severity of UGIB > LGIB]
LGIB is more common in women > men.
Incidence and prevalence related to specific
etiologies.](https://image.slidesharecdn.com/lowergibleed-141104015027-conversion-gate02/85/Lower-gi-bleed-3-320.jpg)