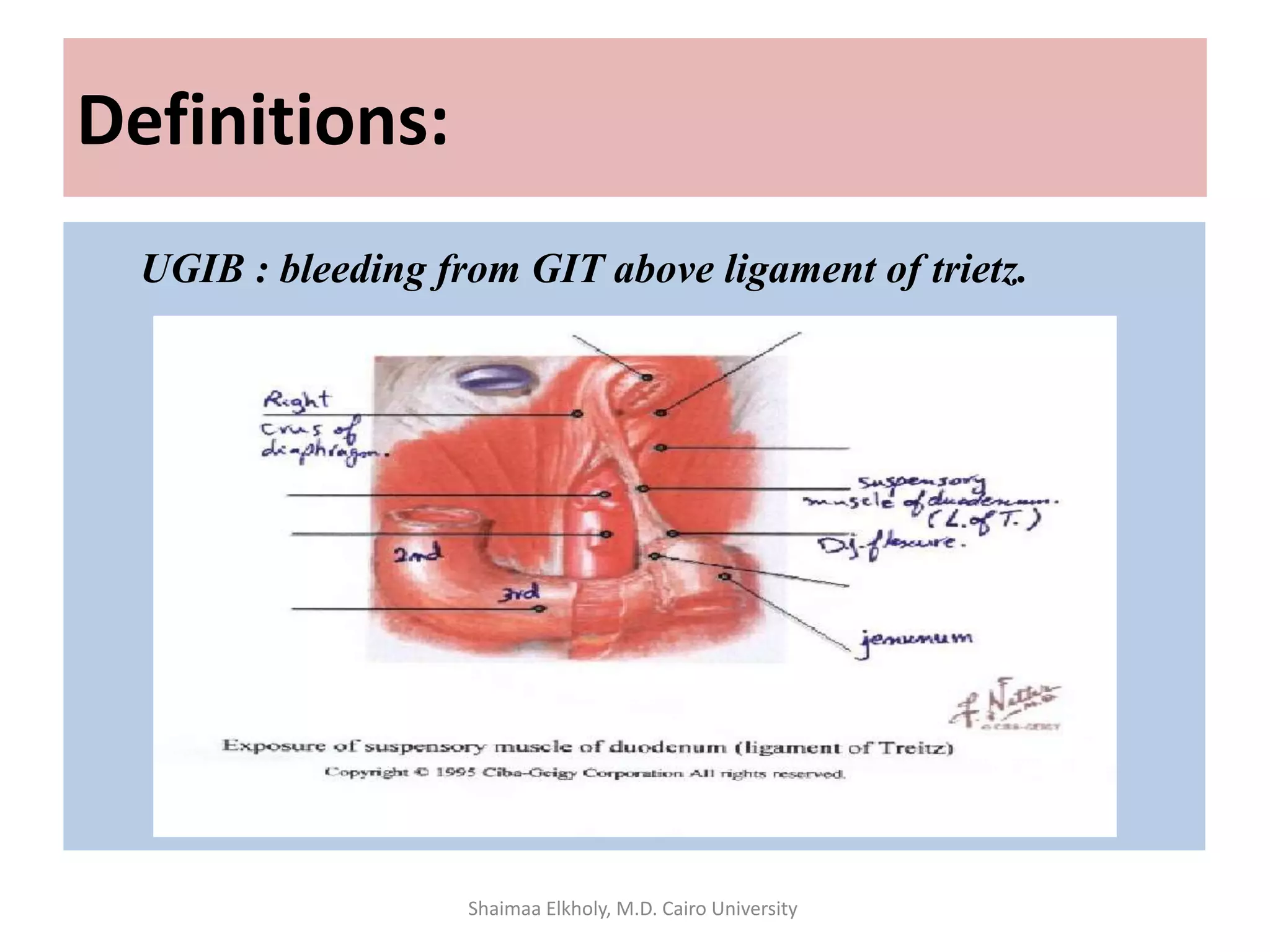
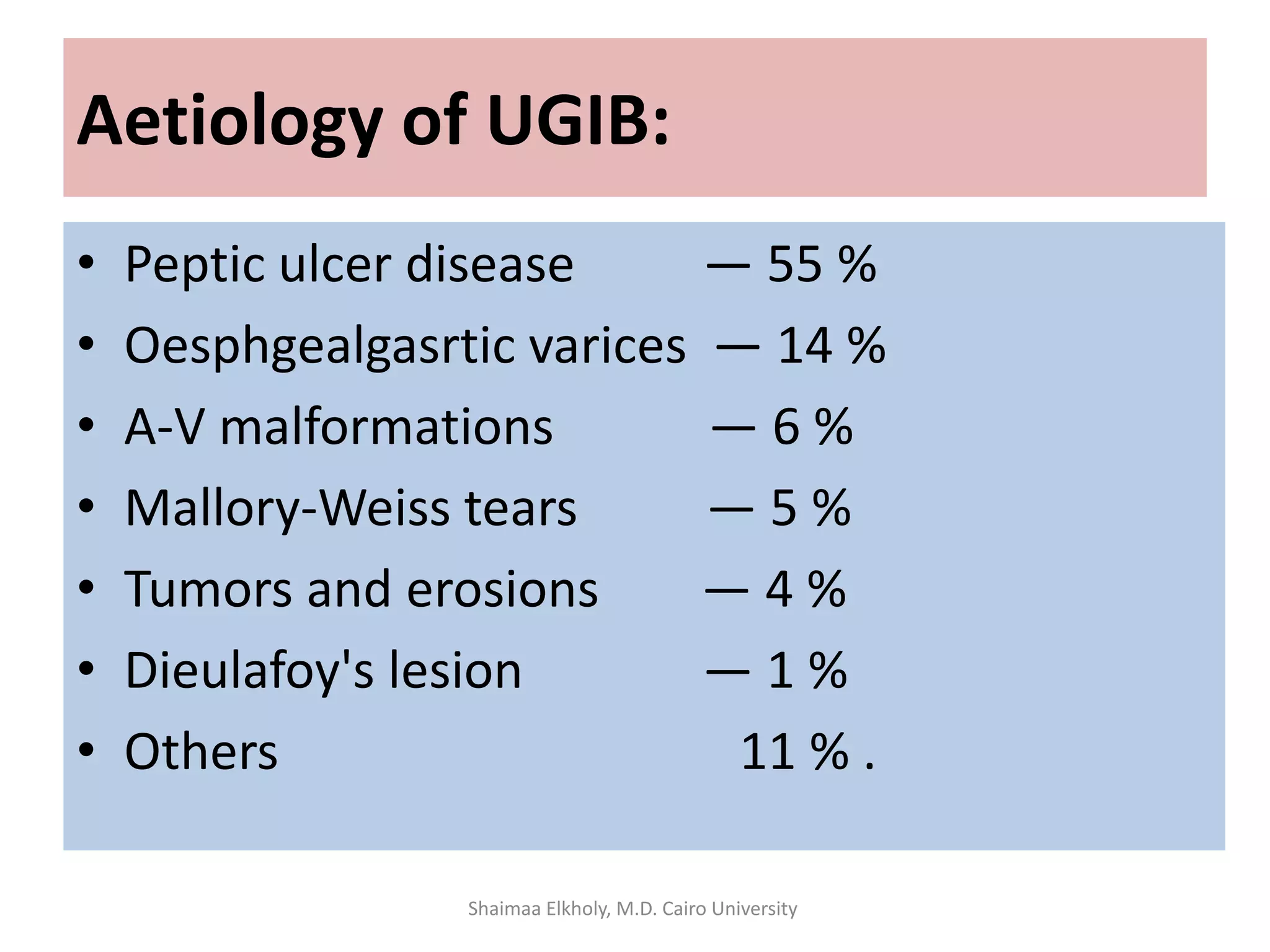
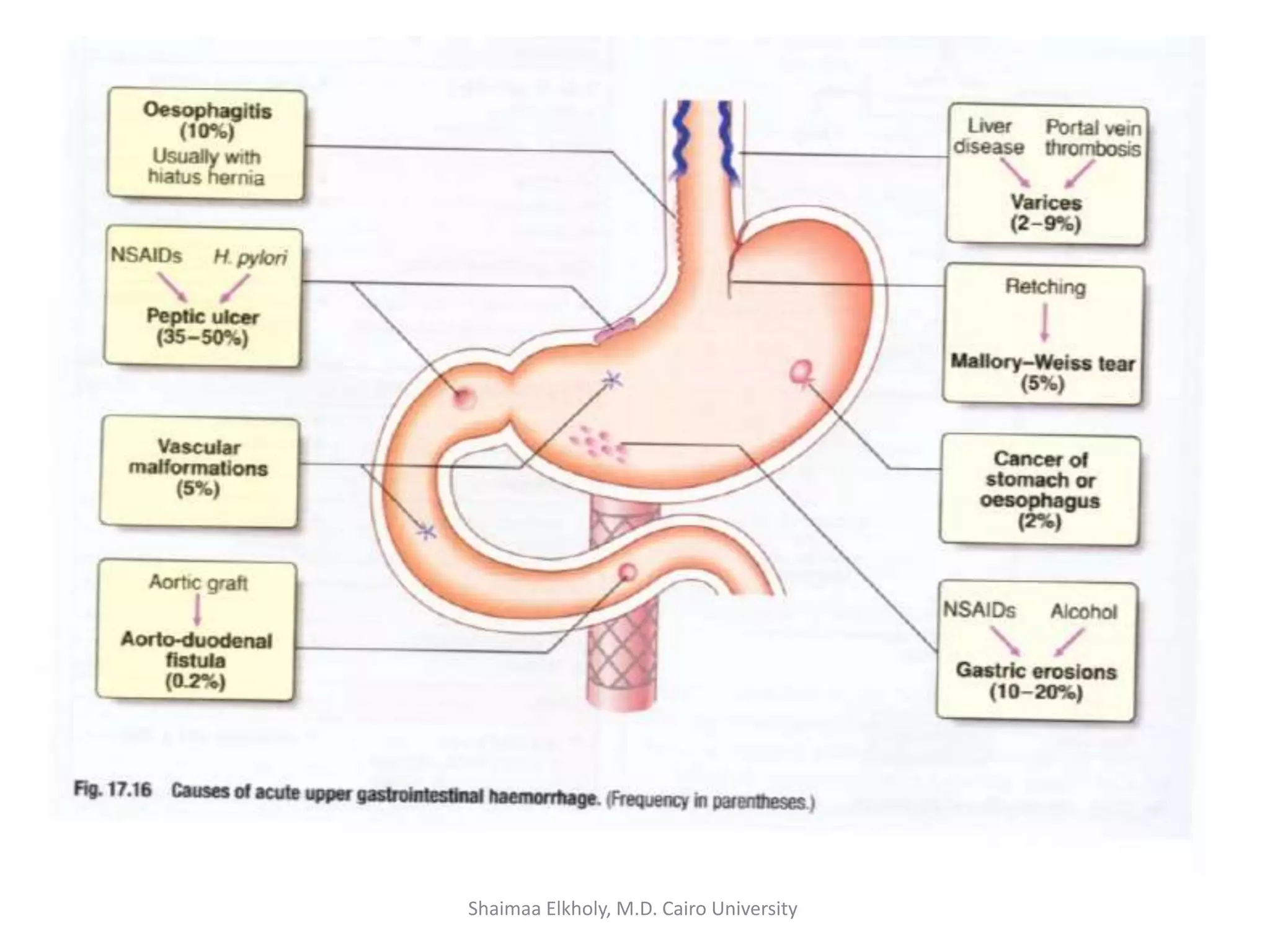
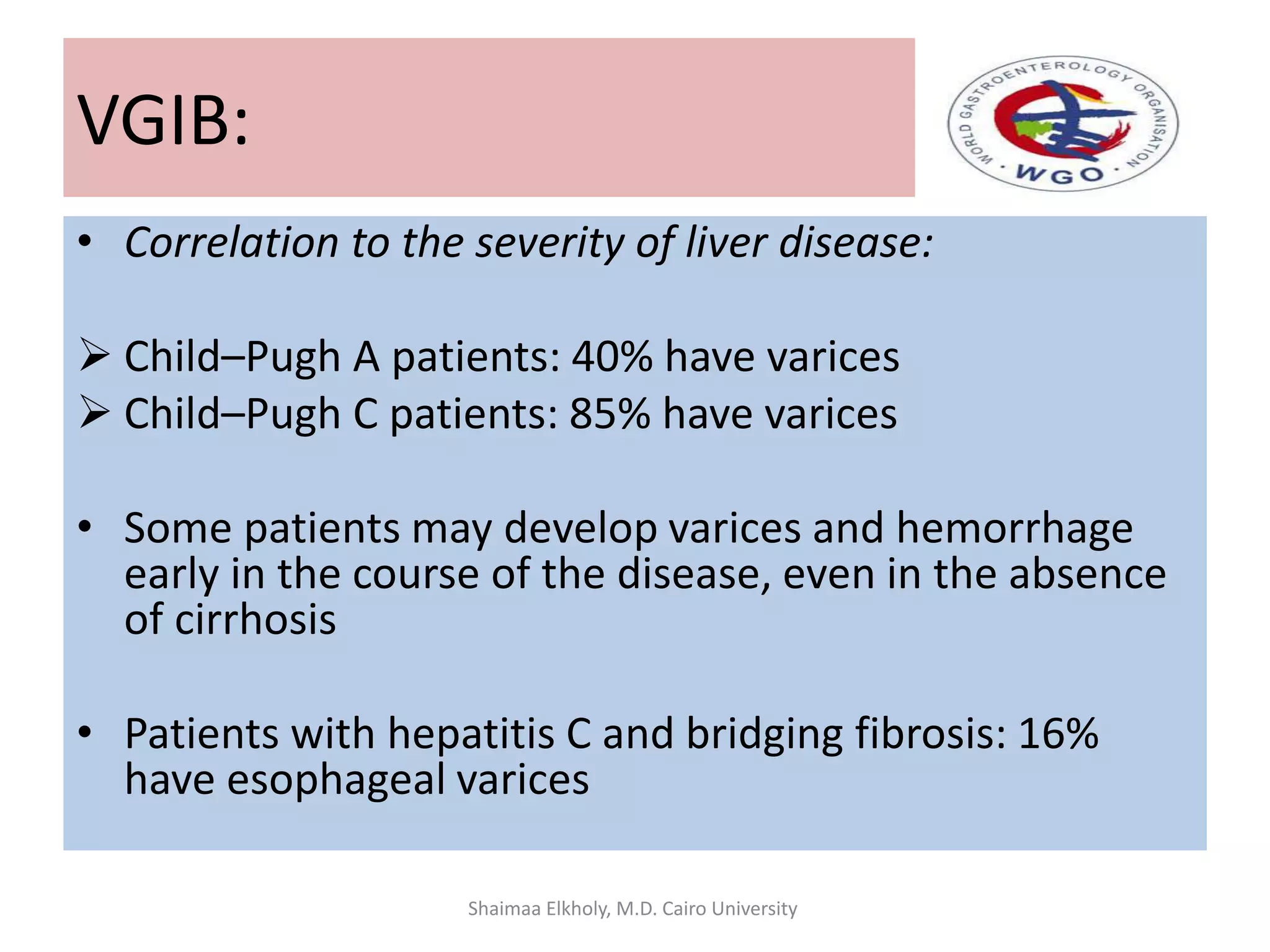
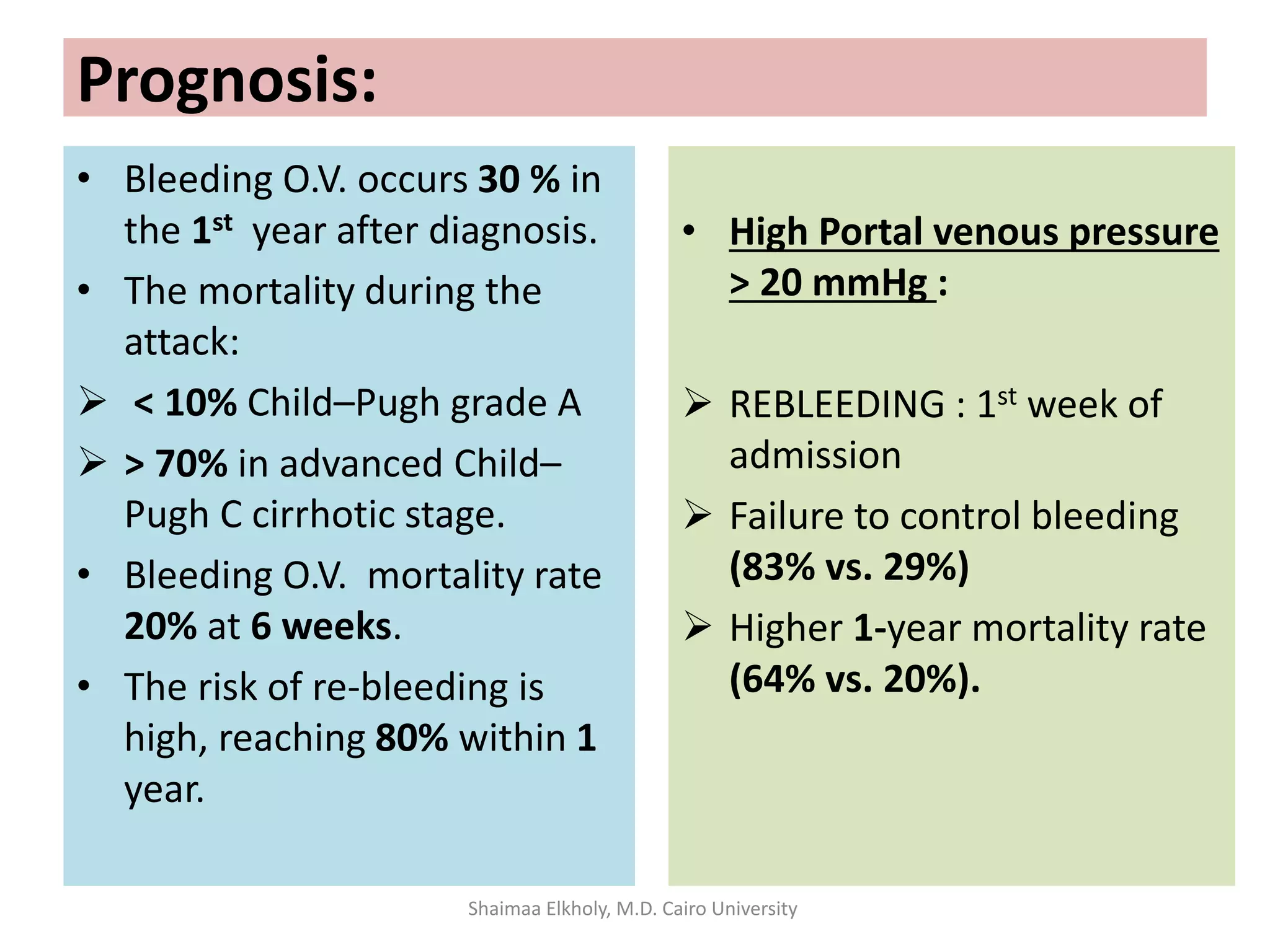
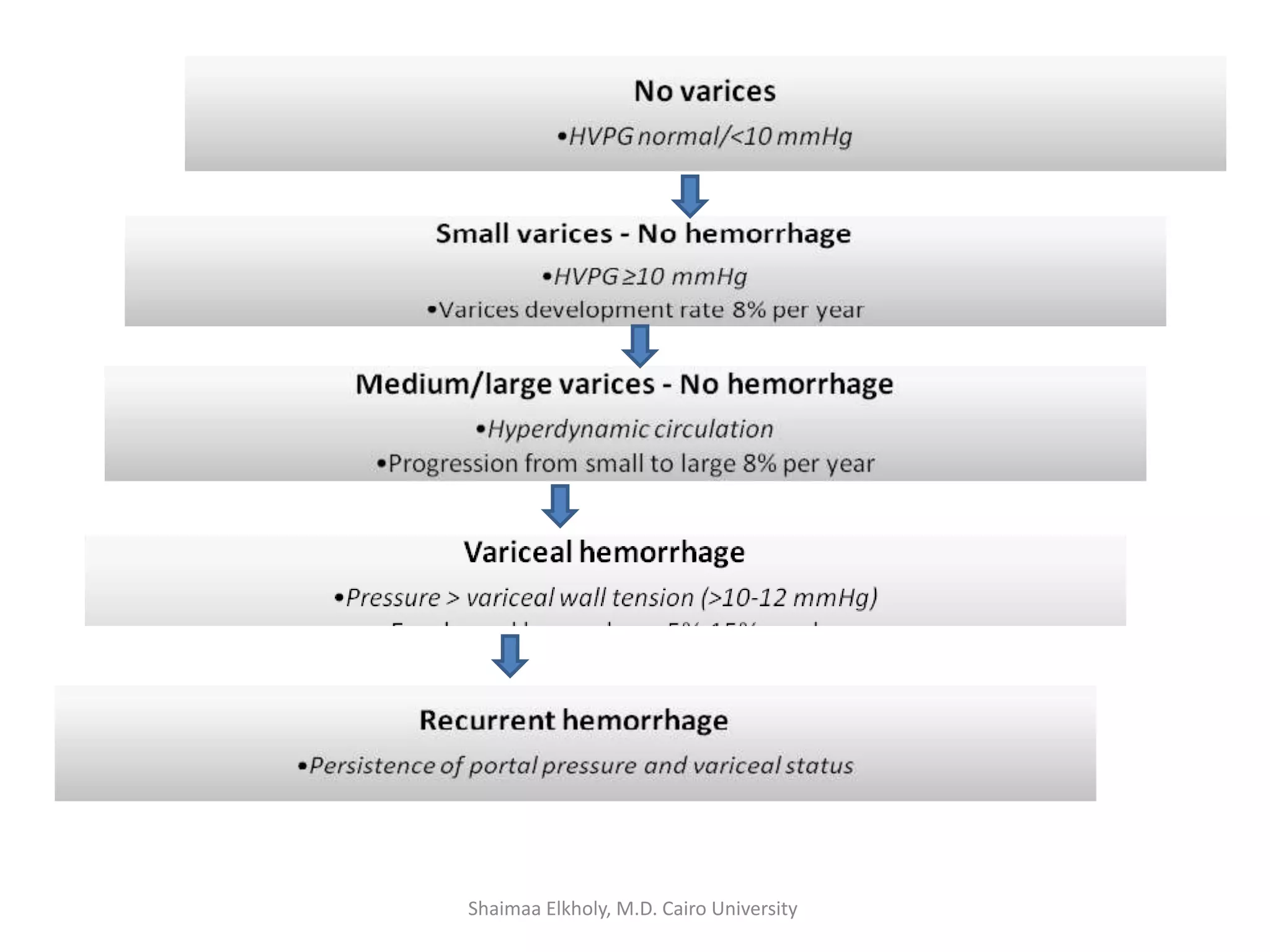
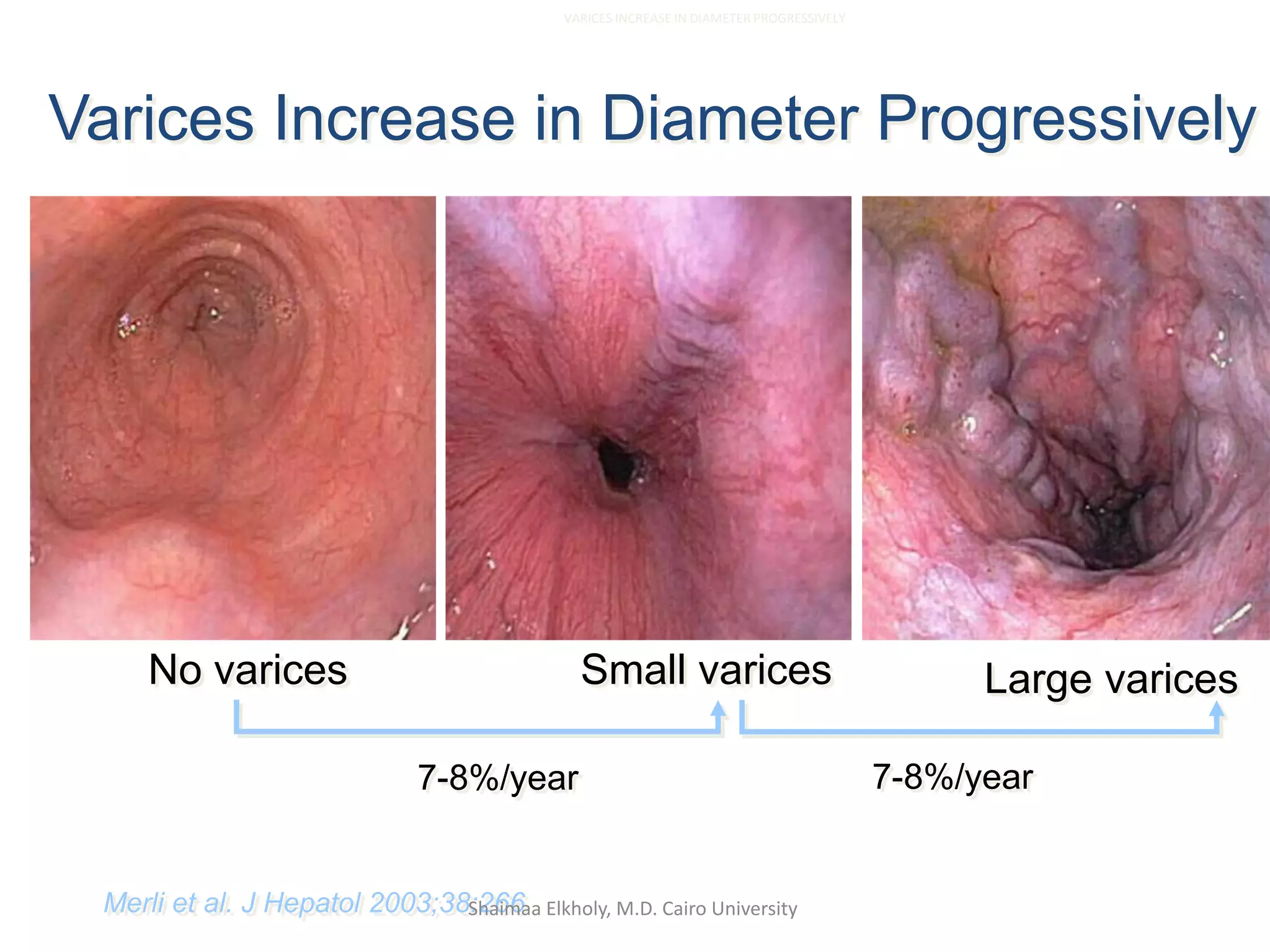
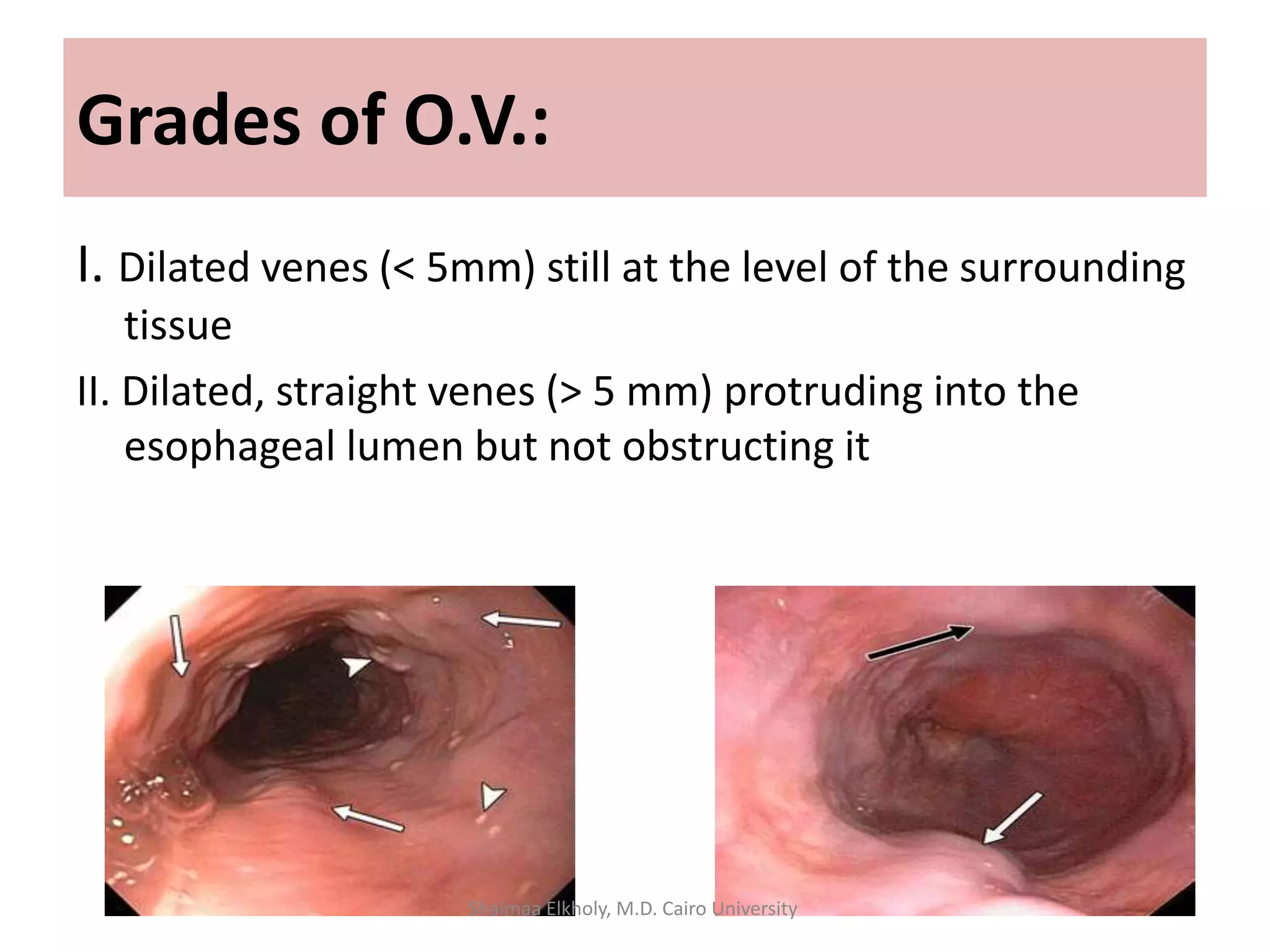
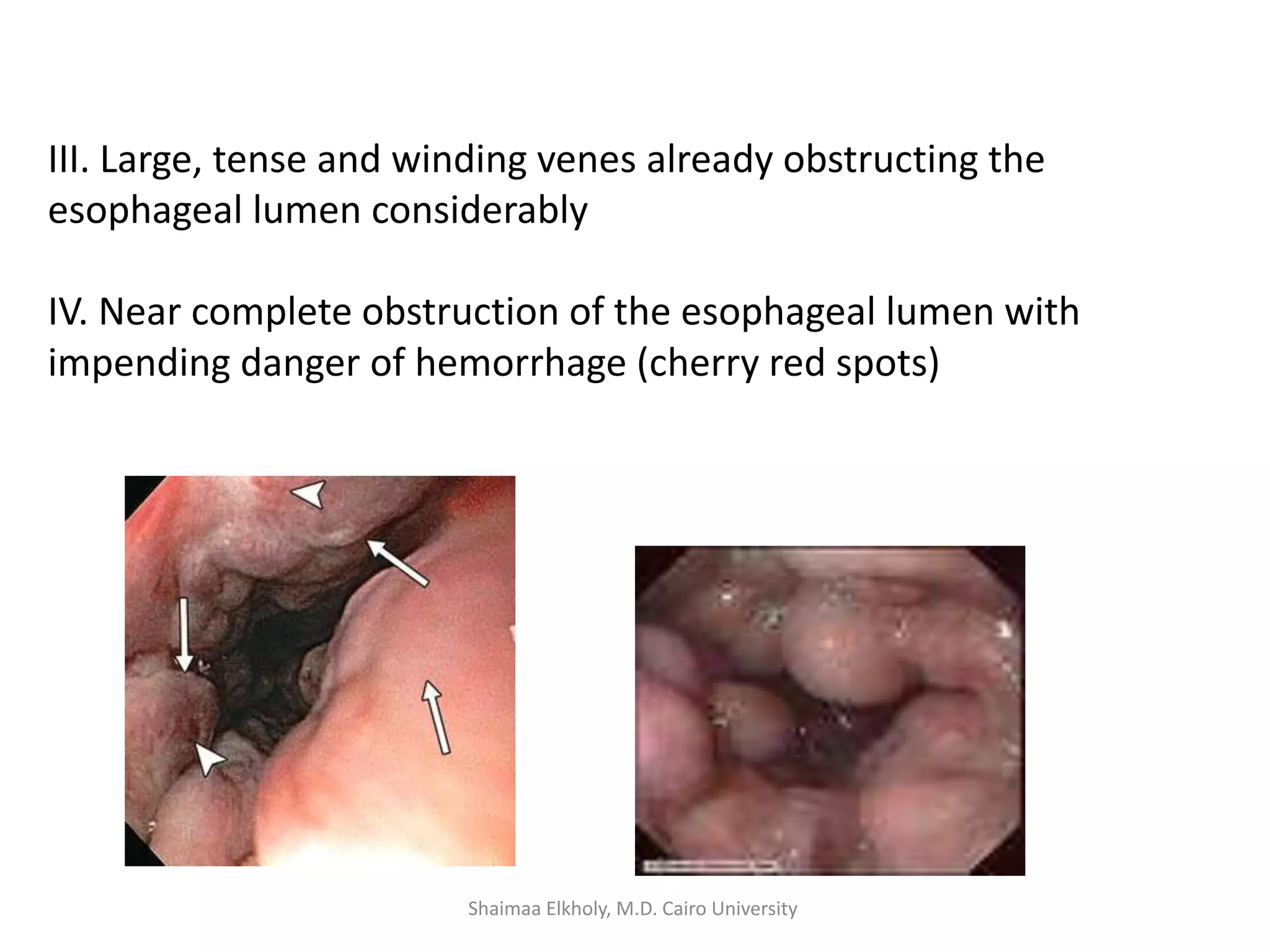
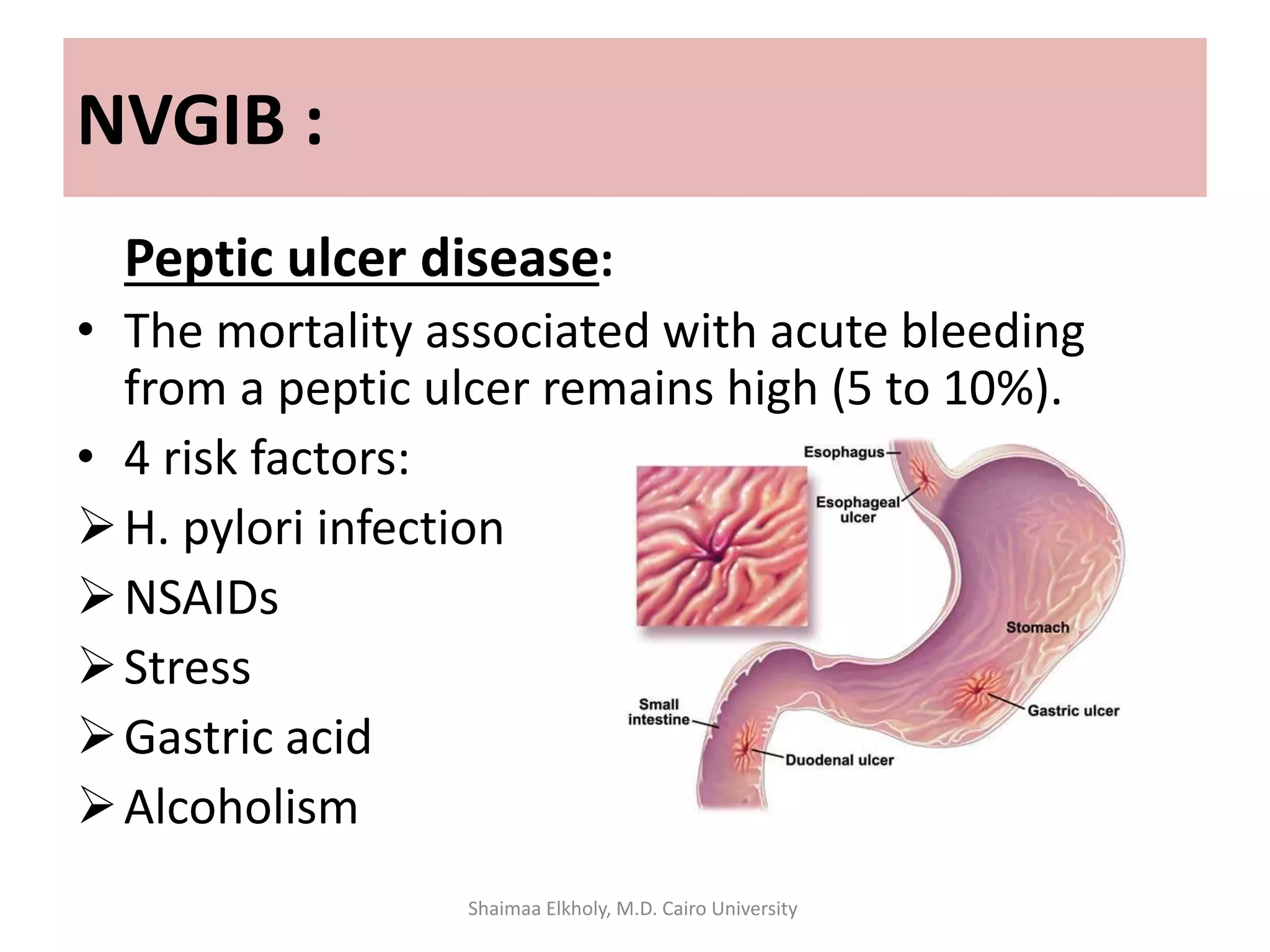
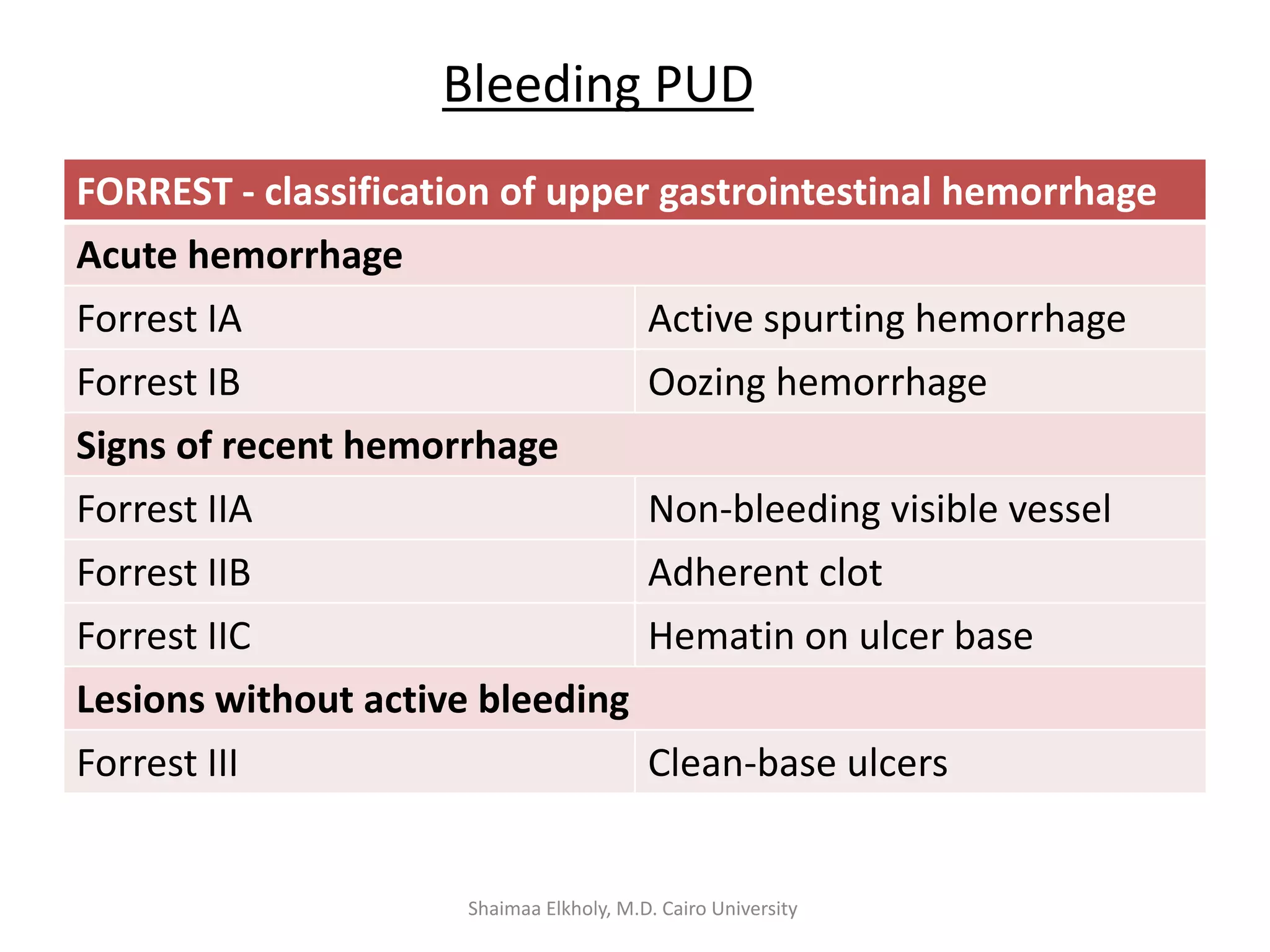
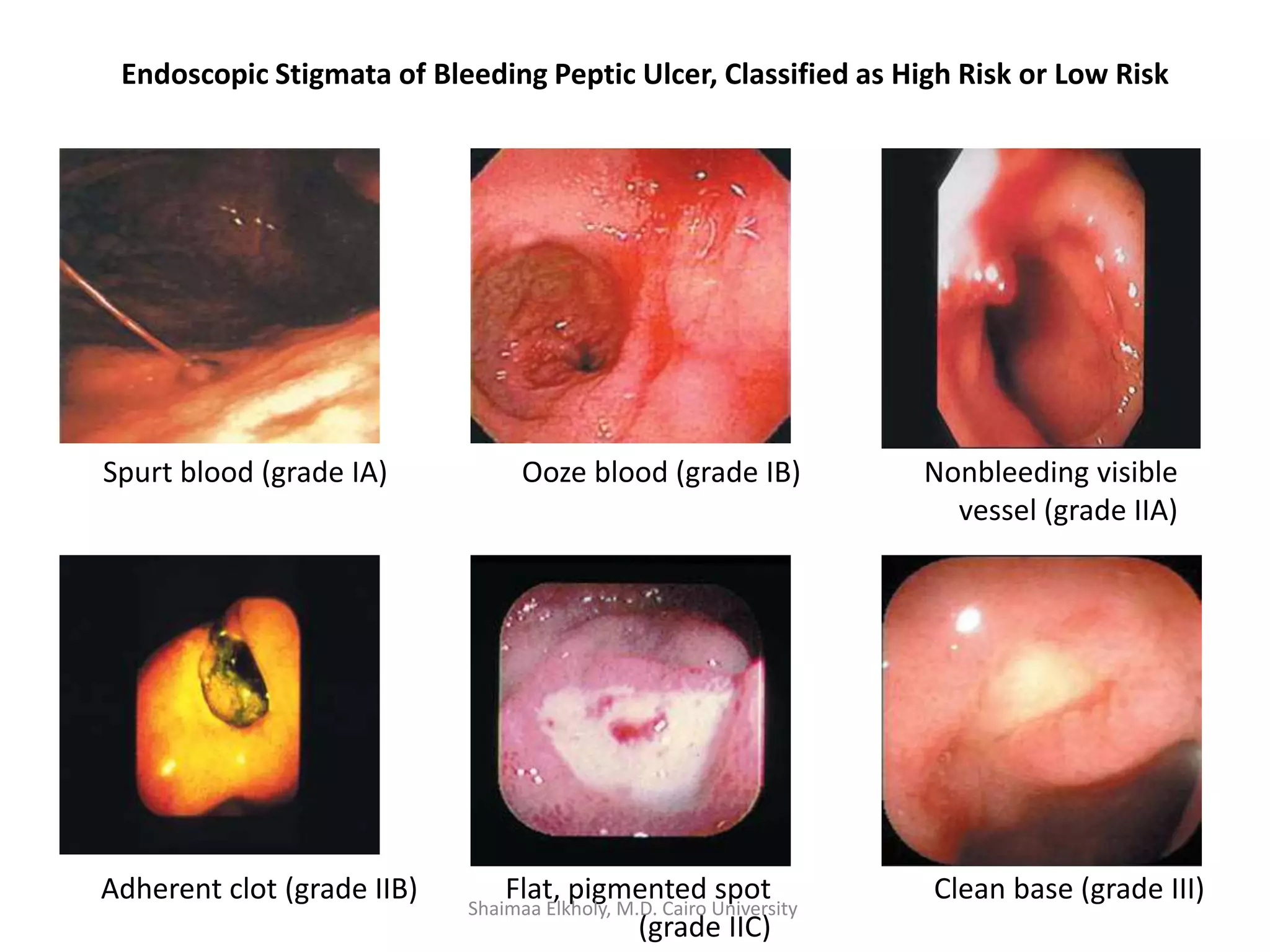
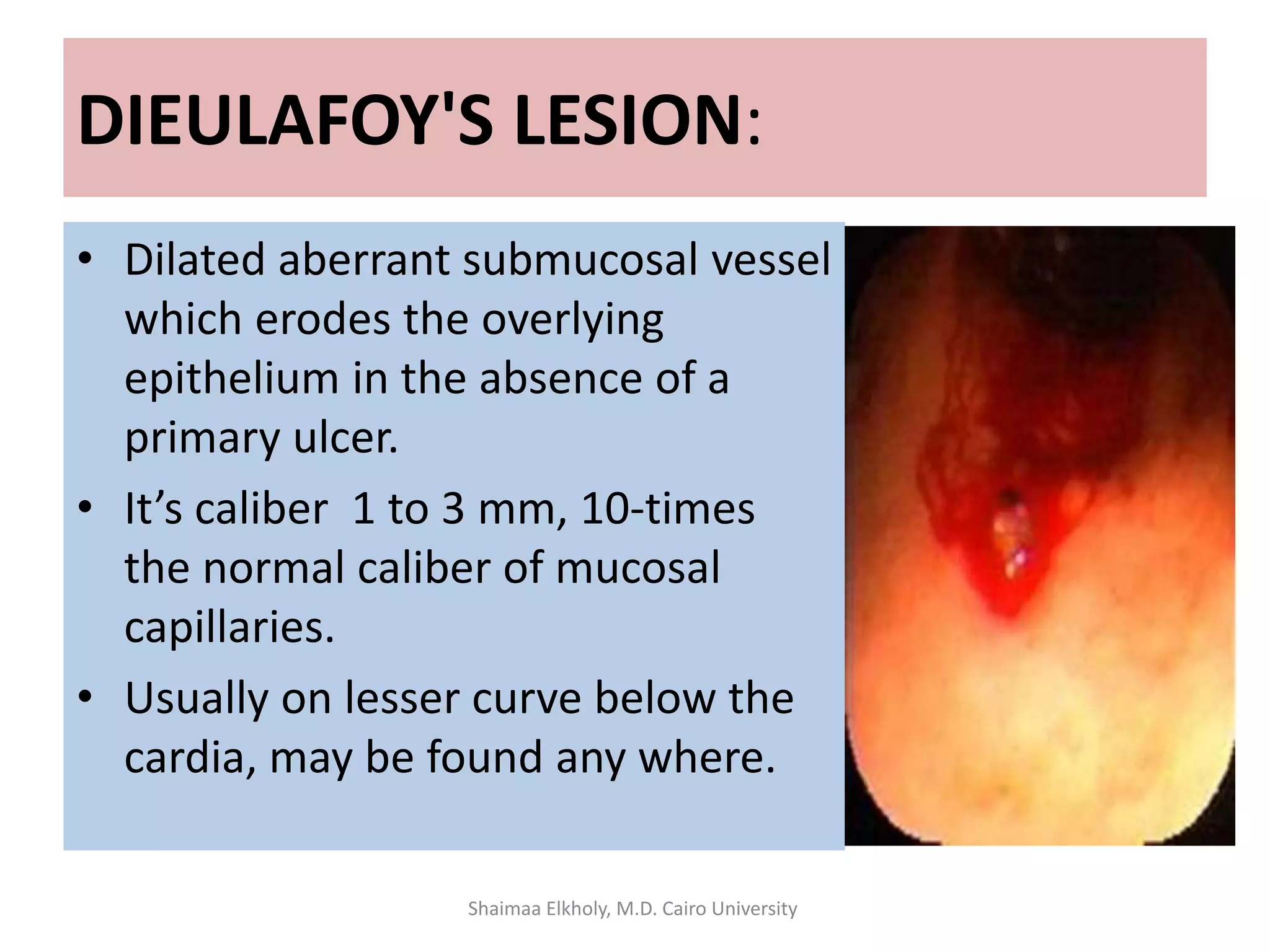
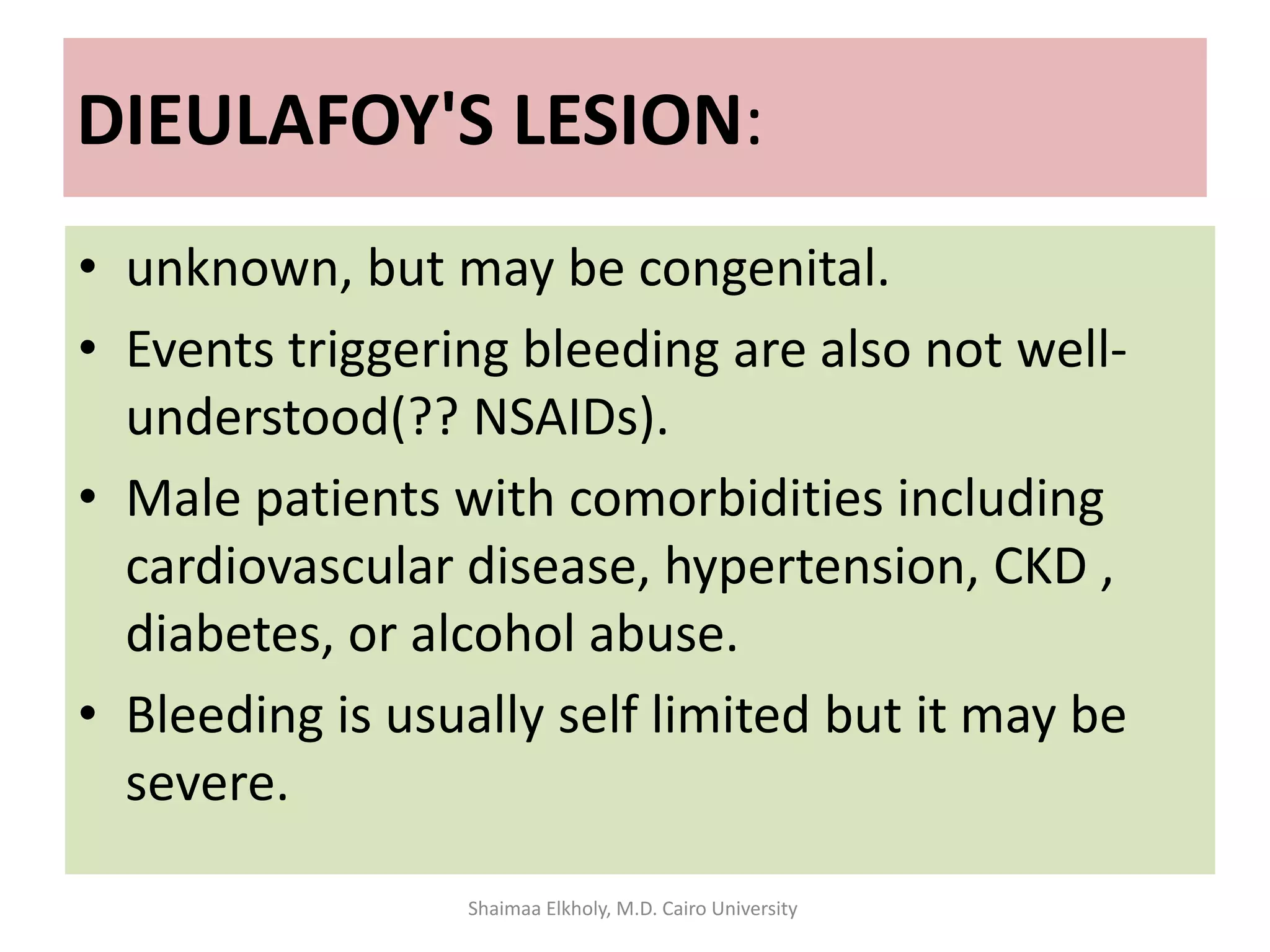
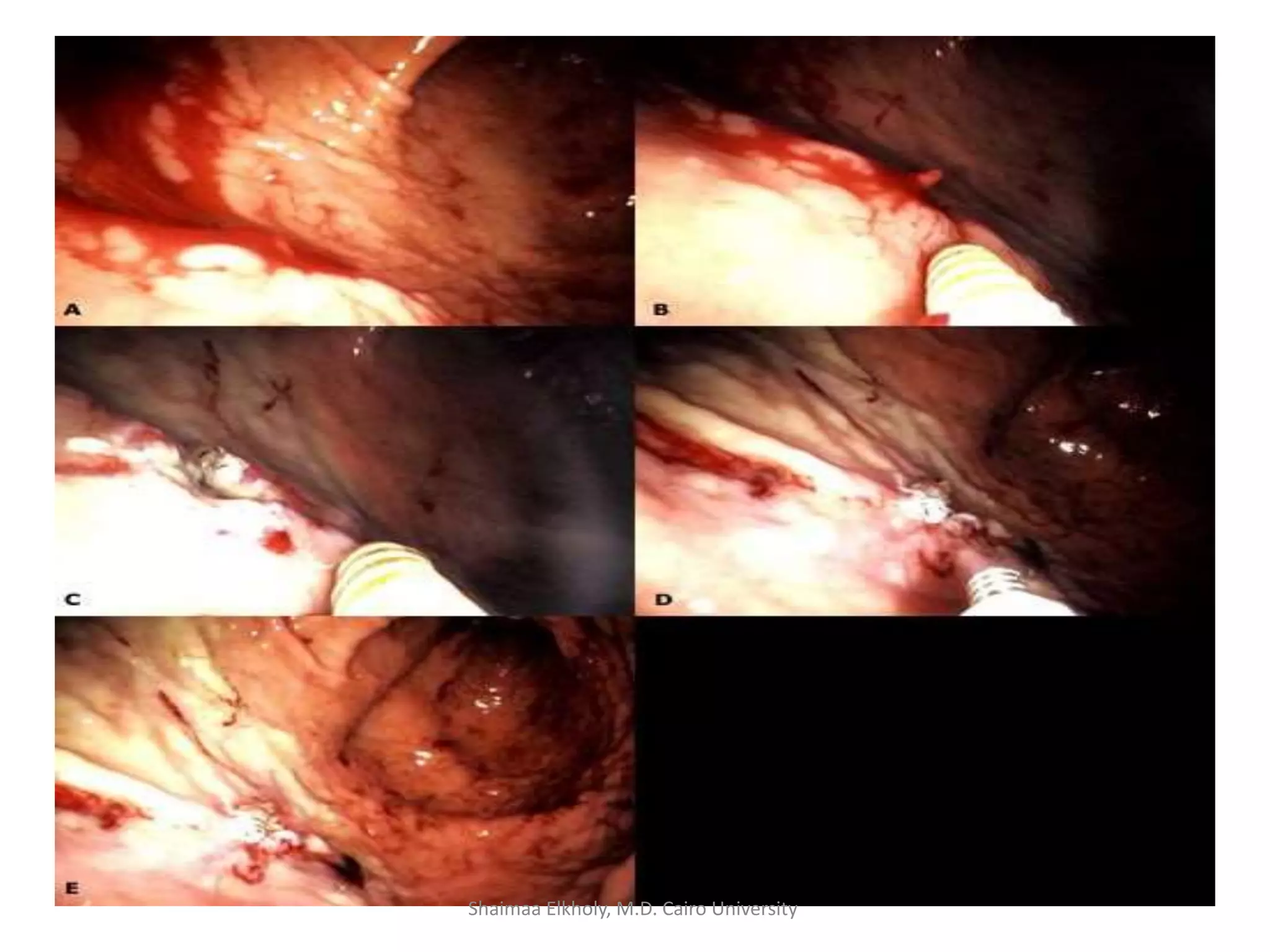
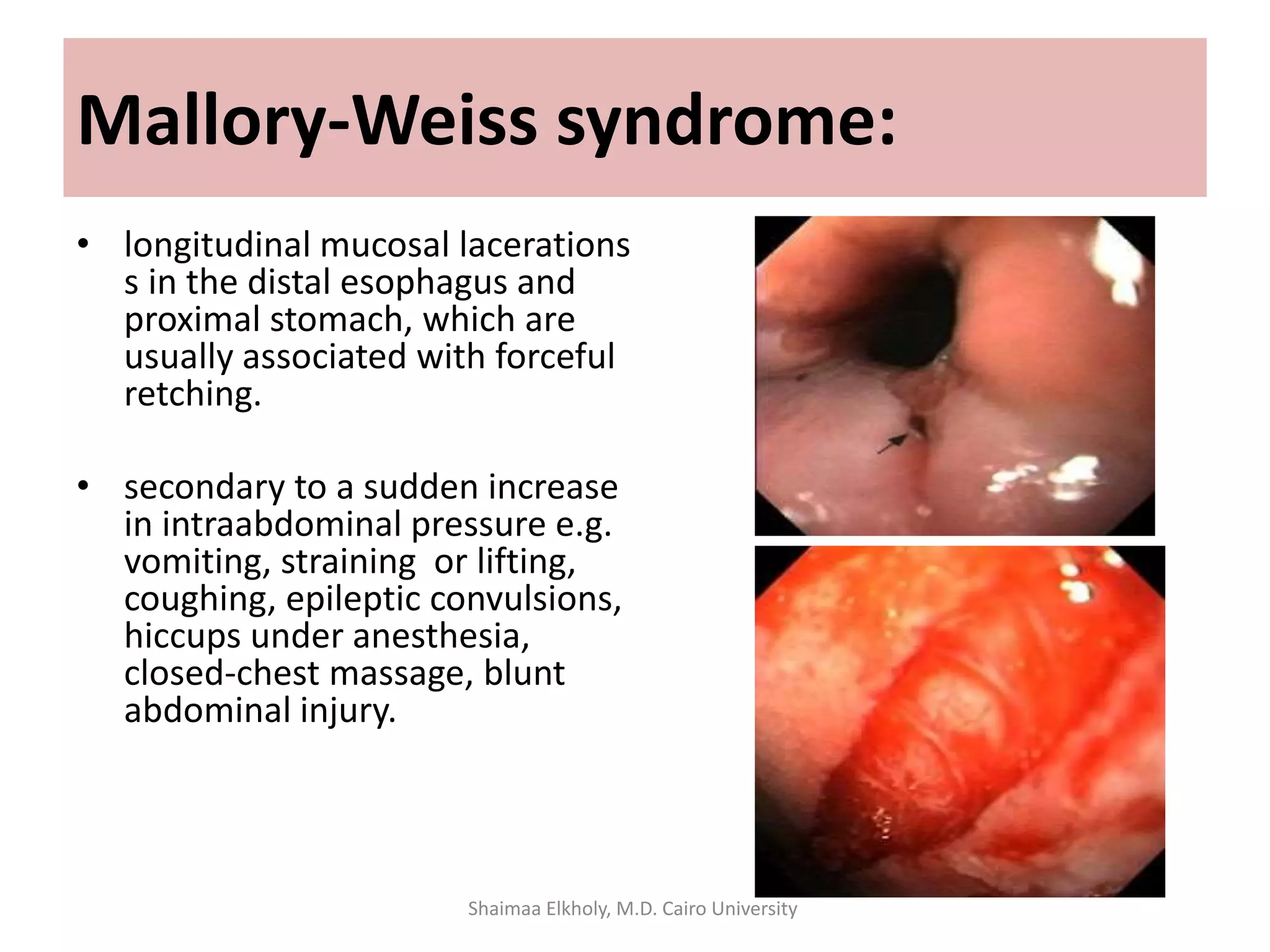
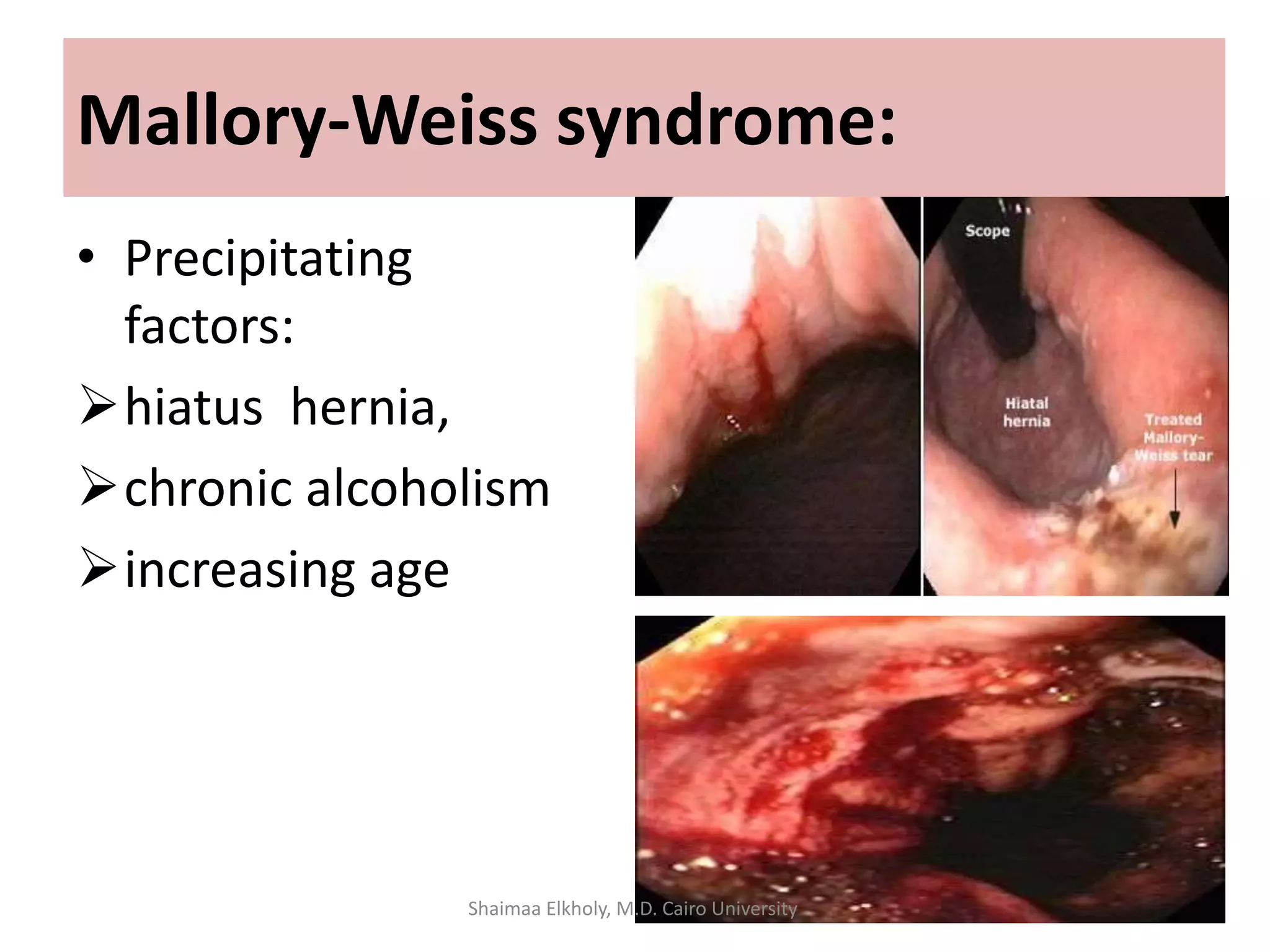
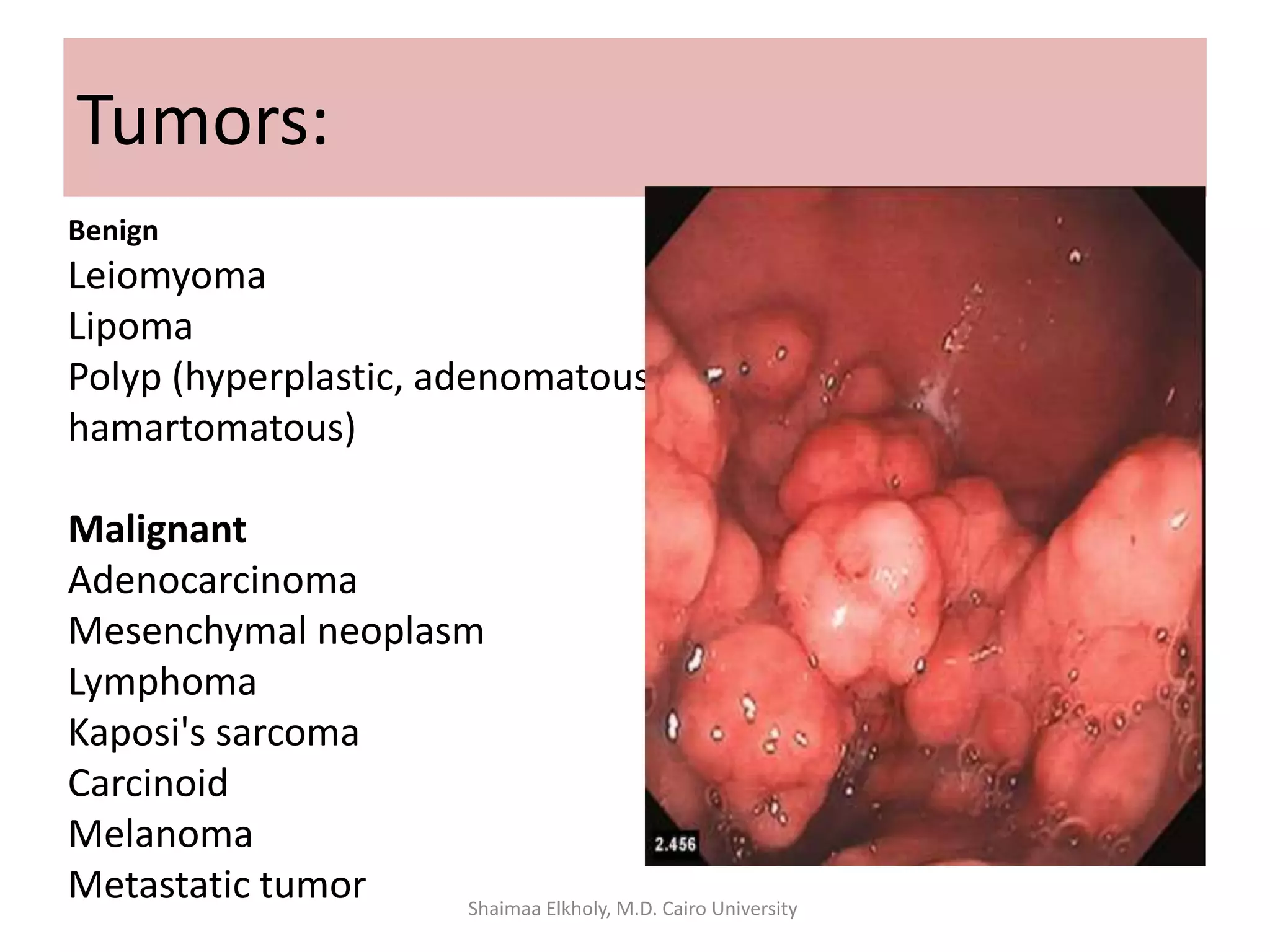
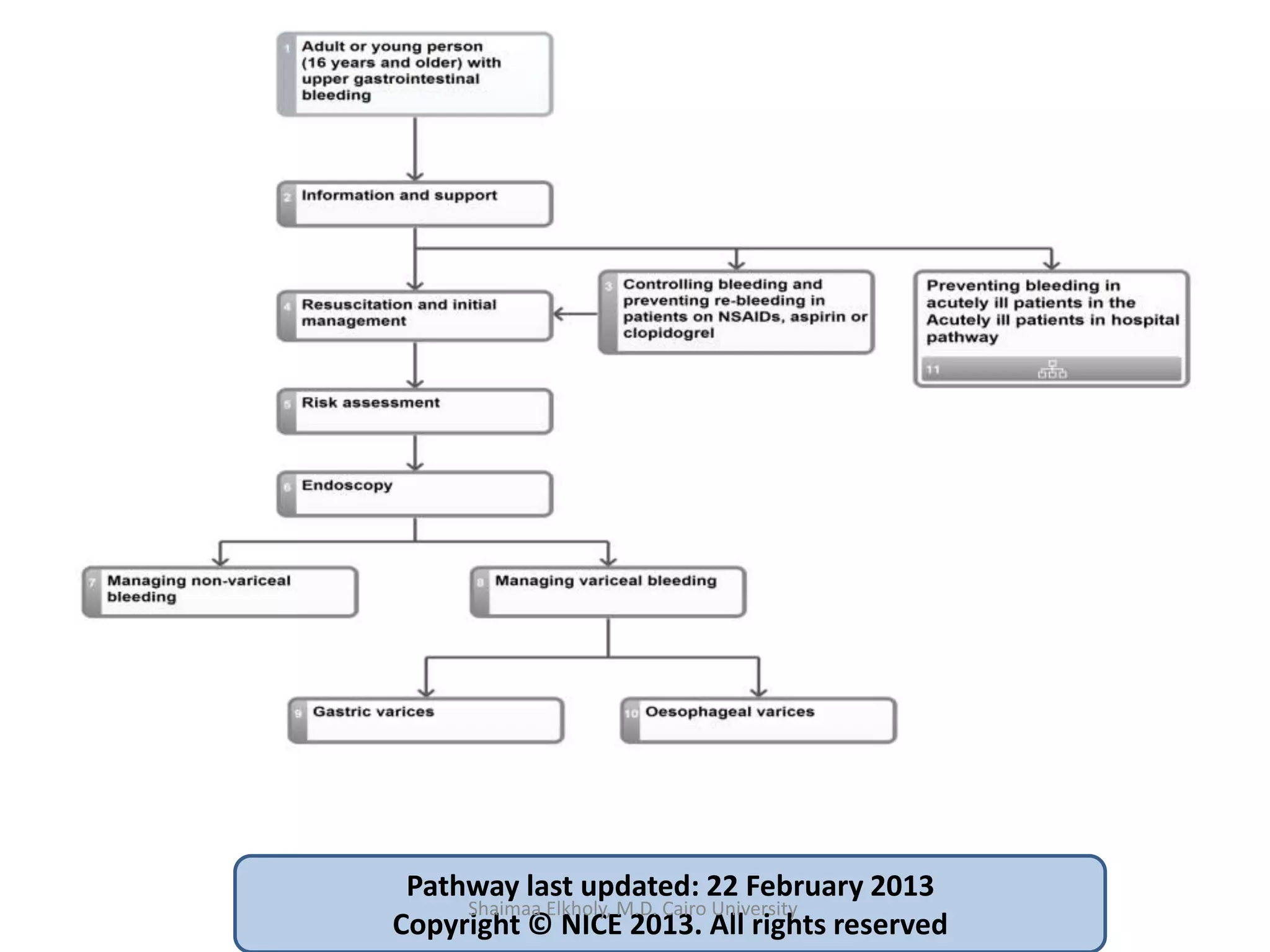
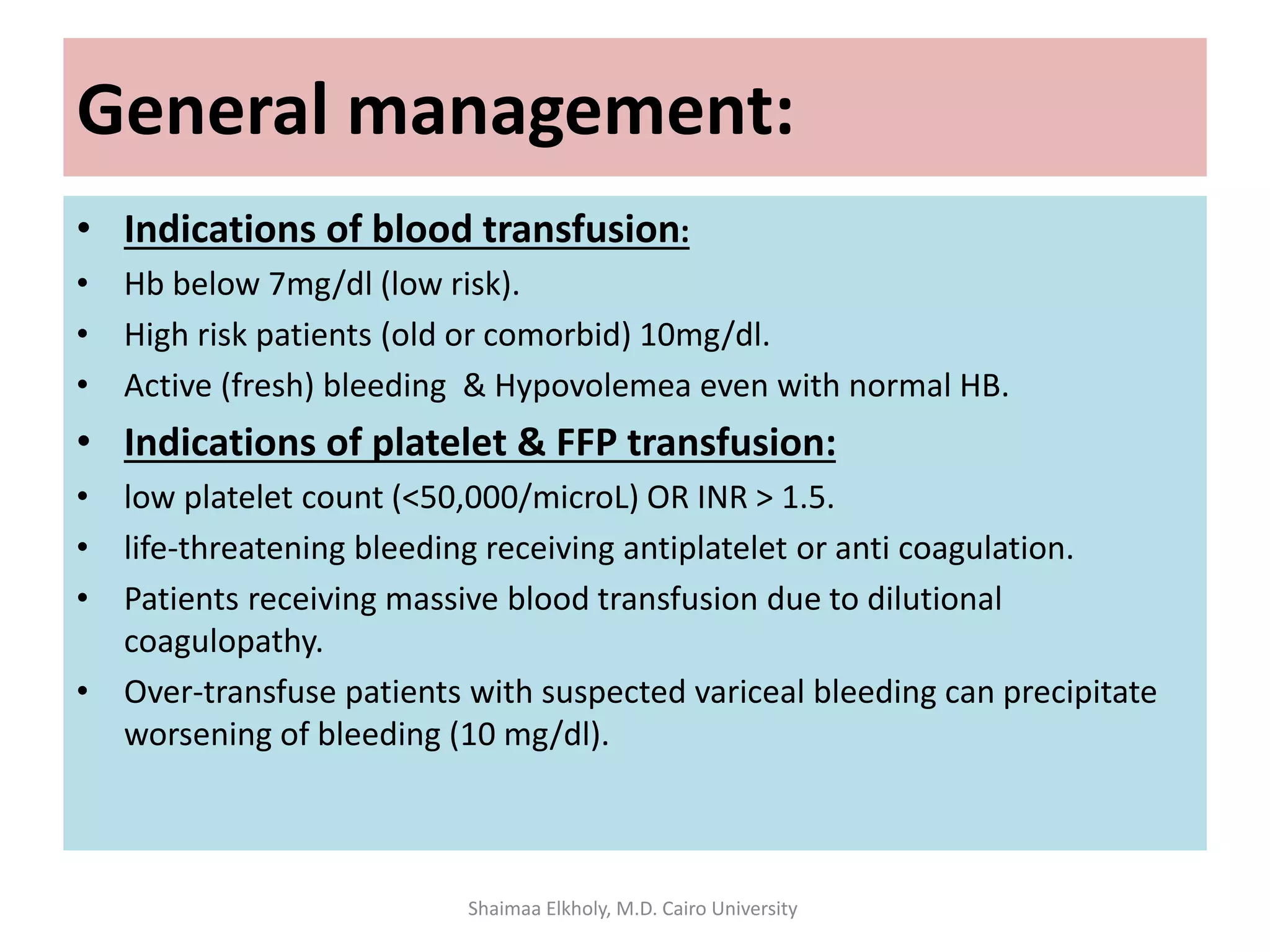
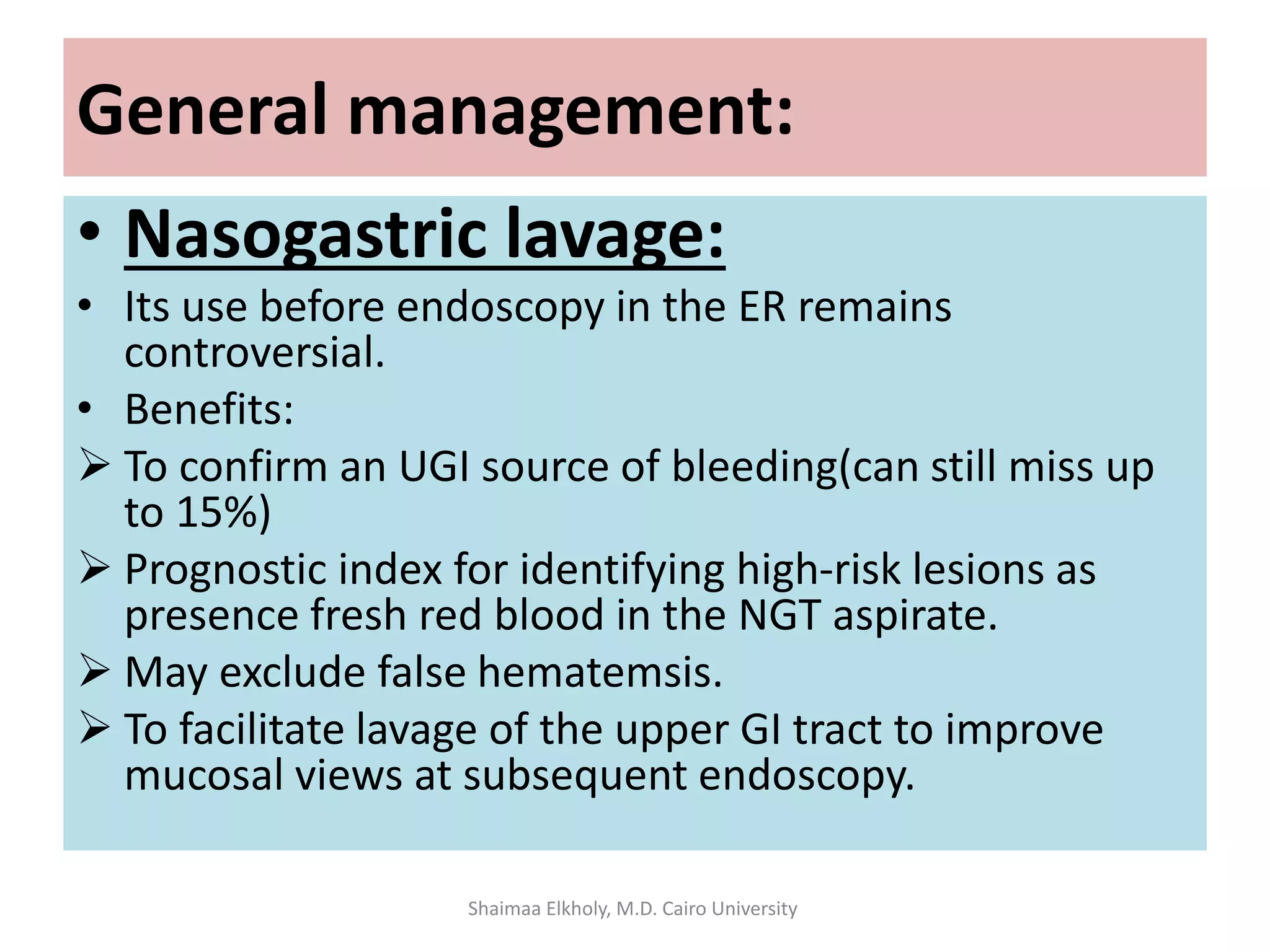
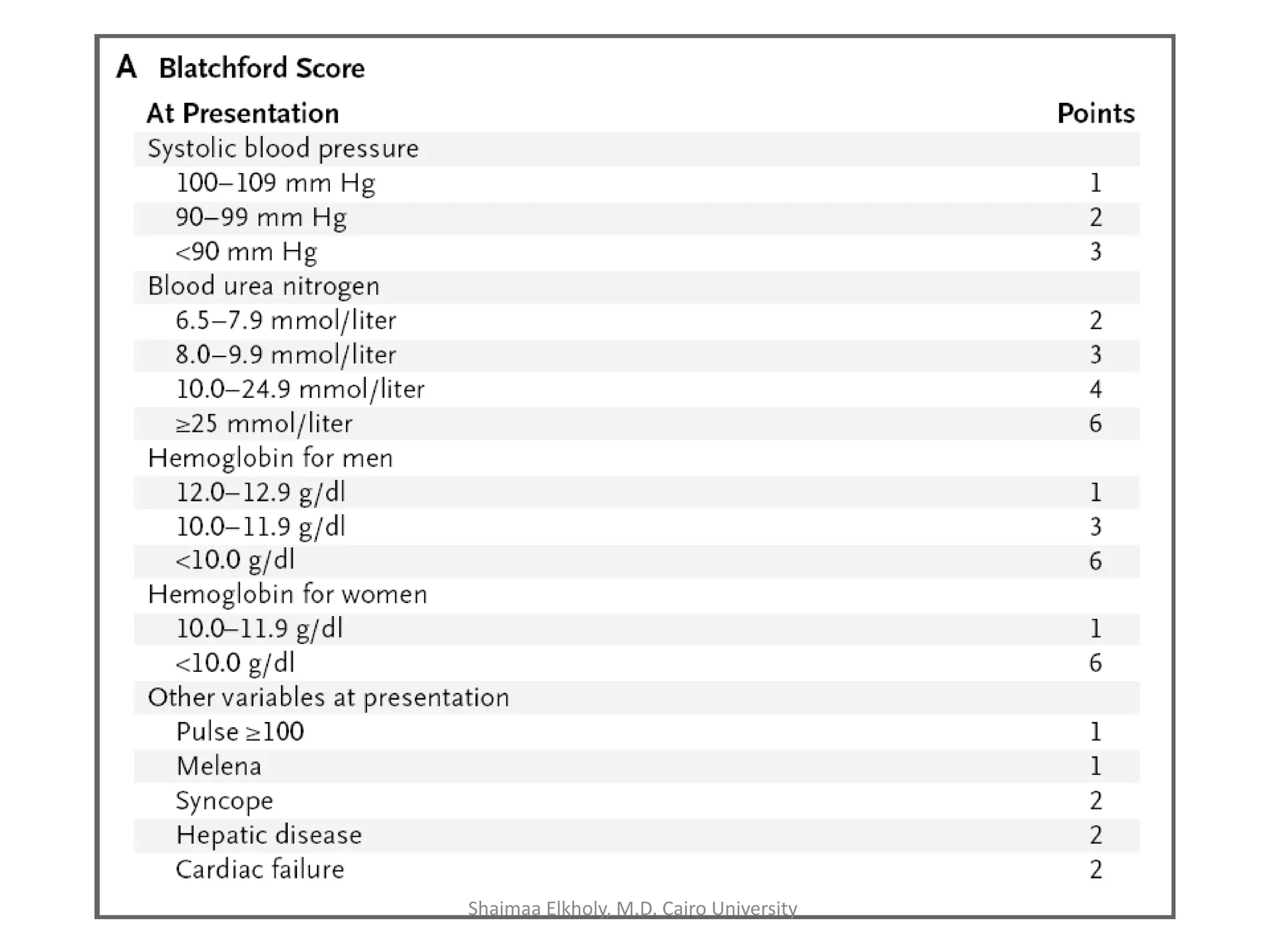
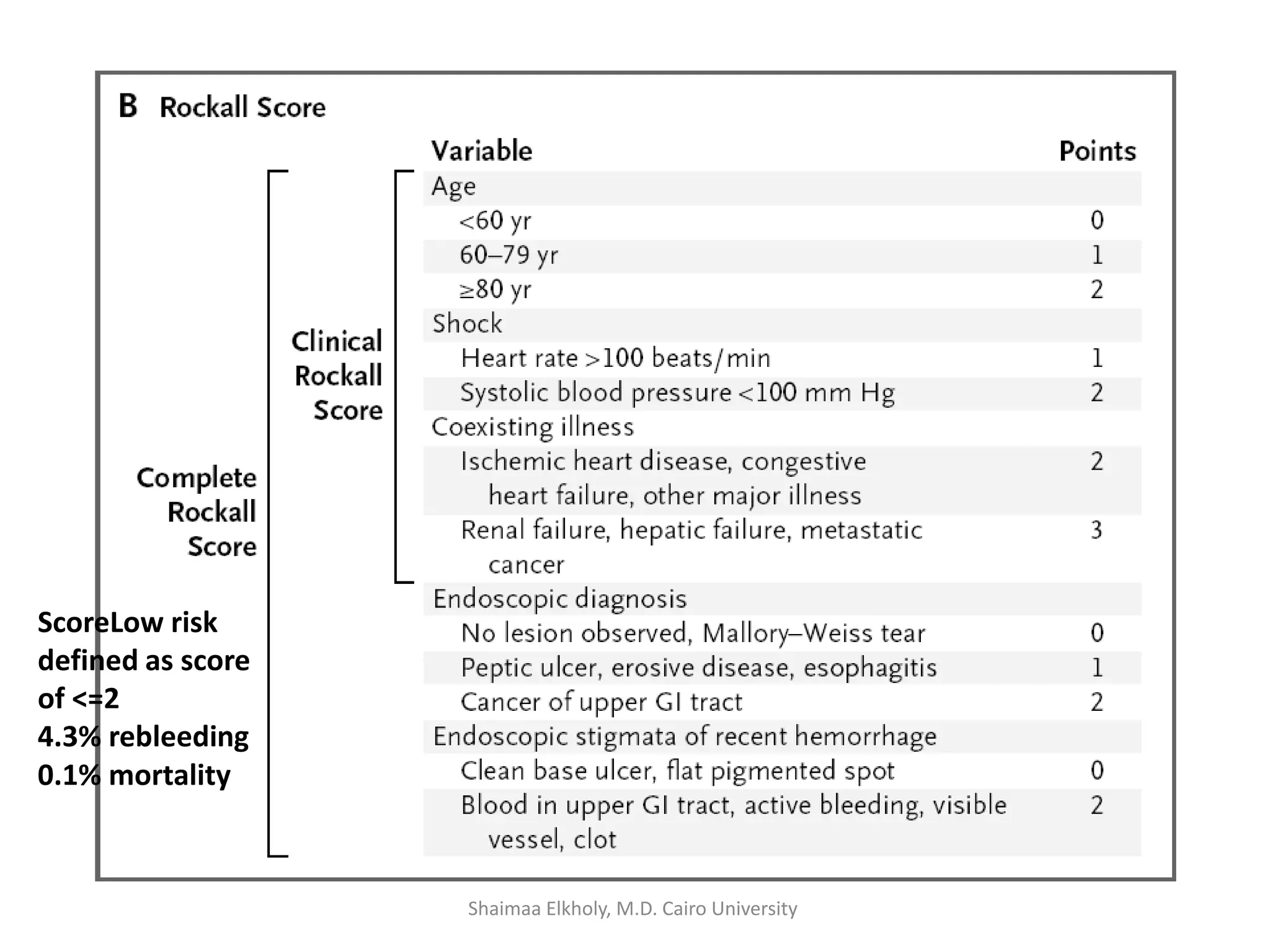
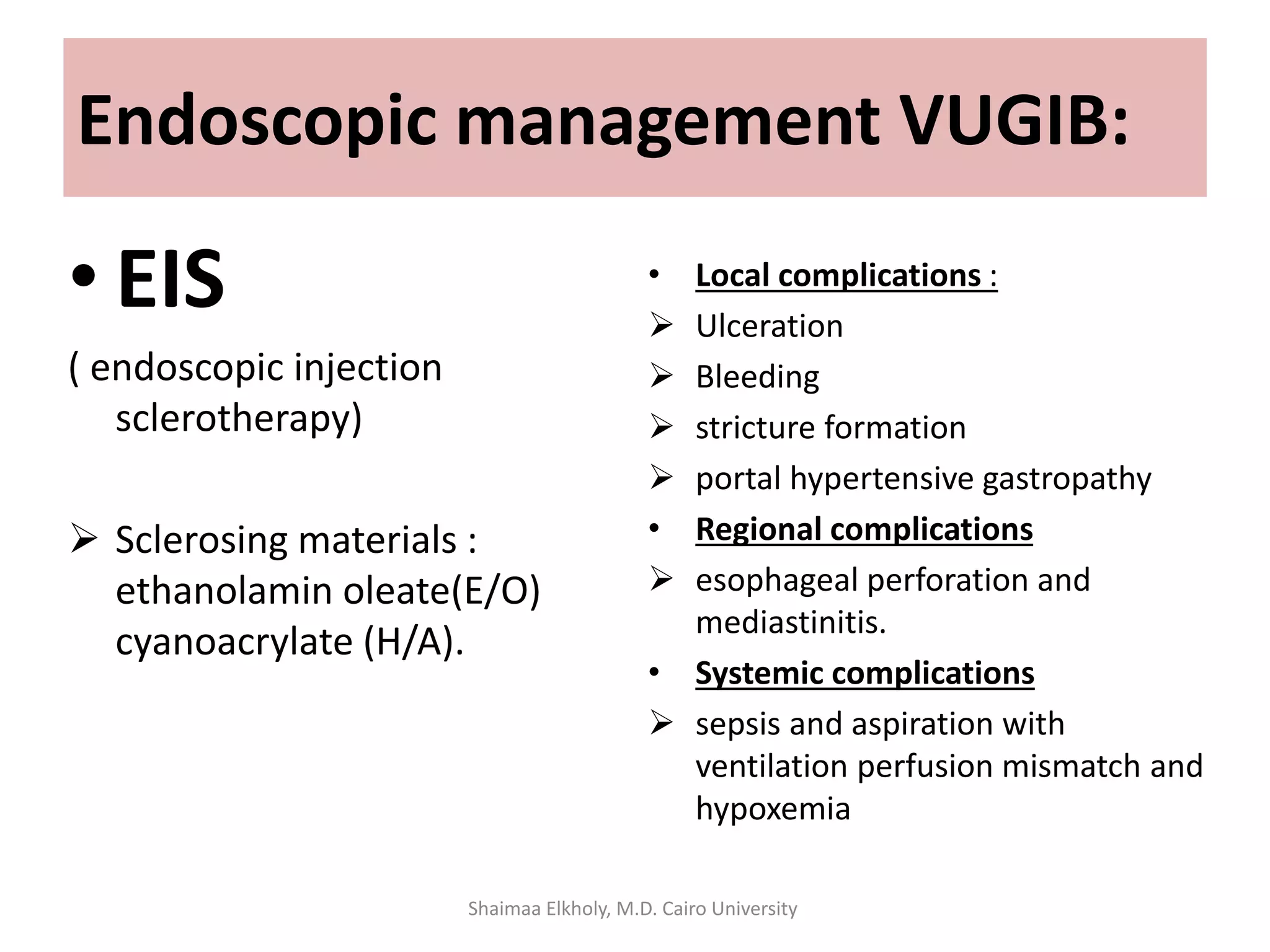
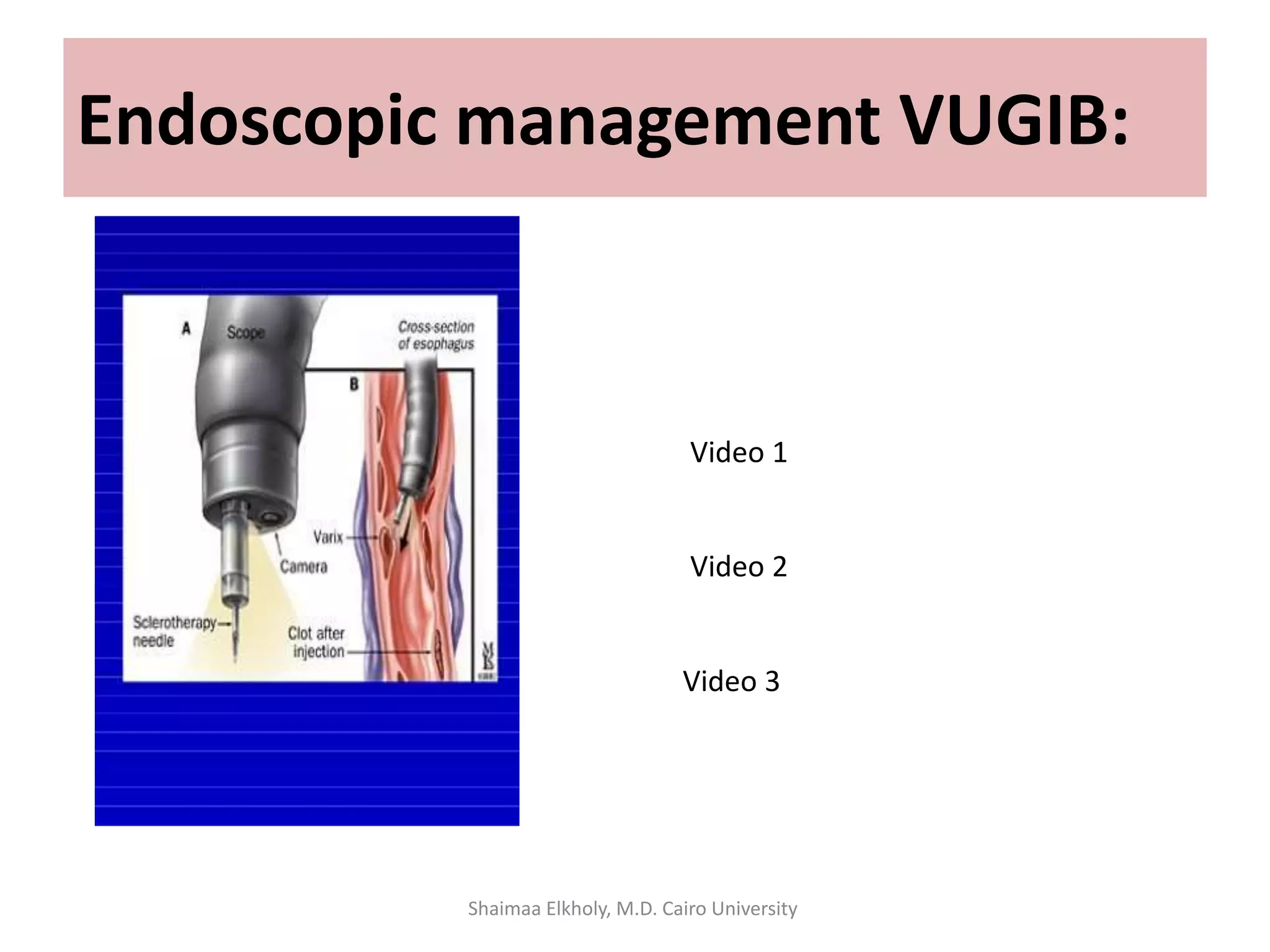
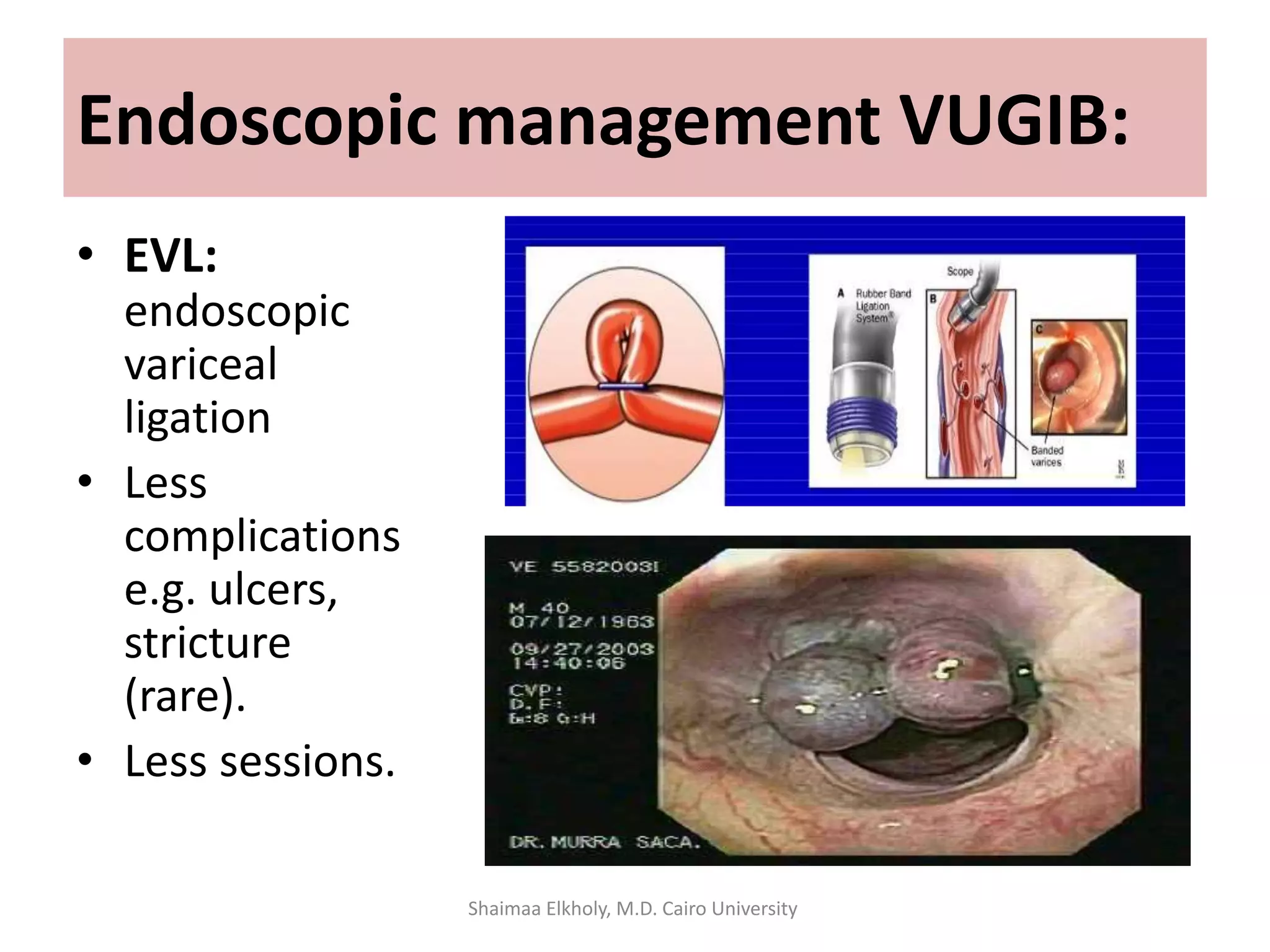
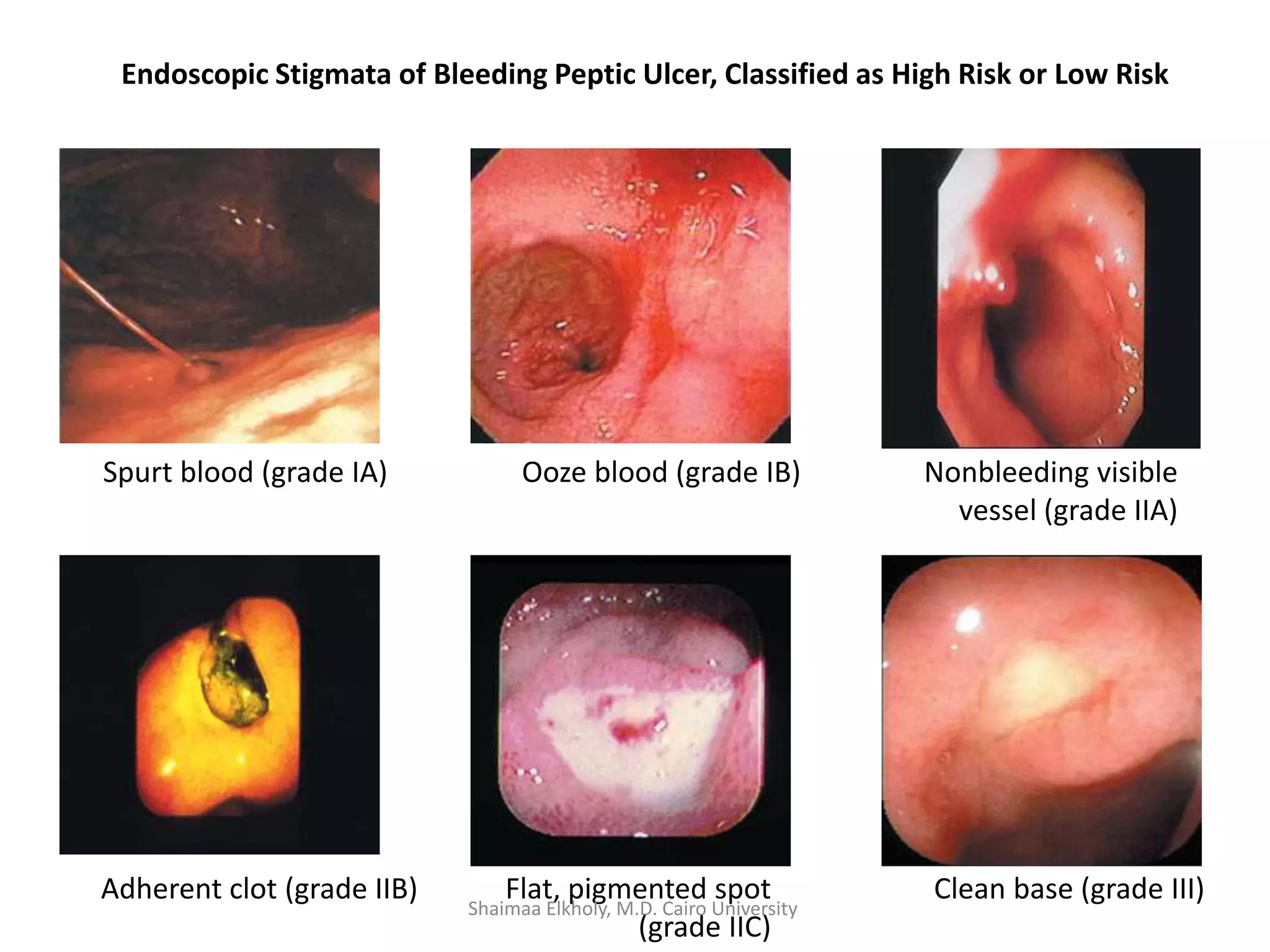
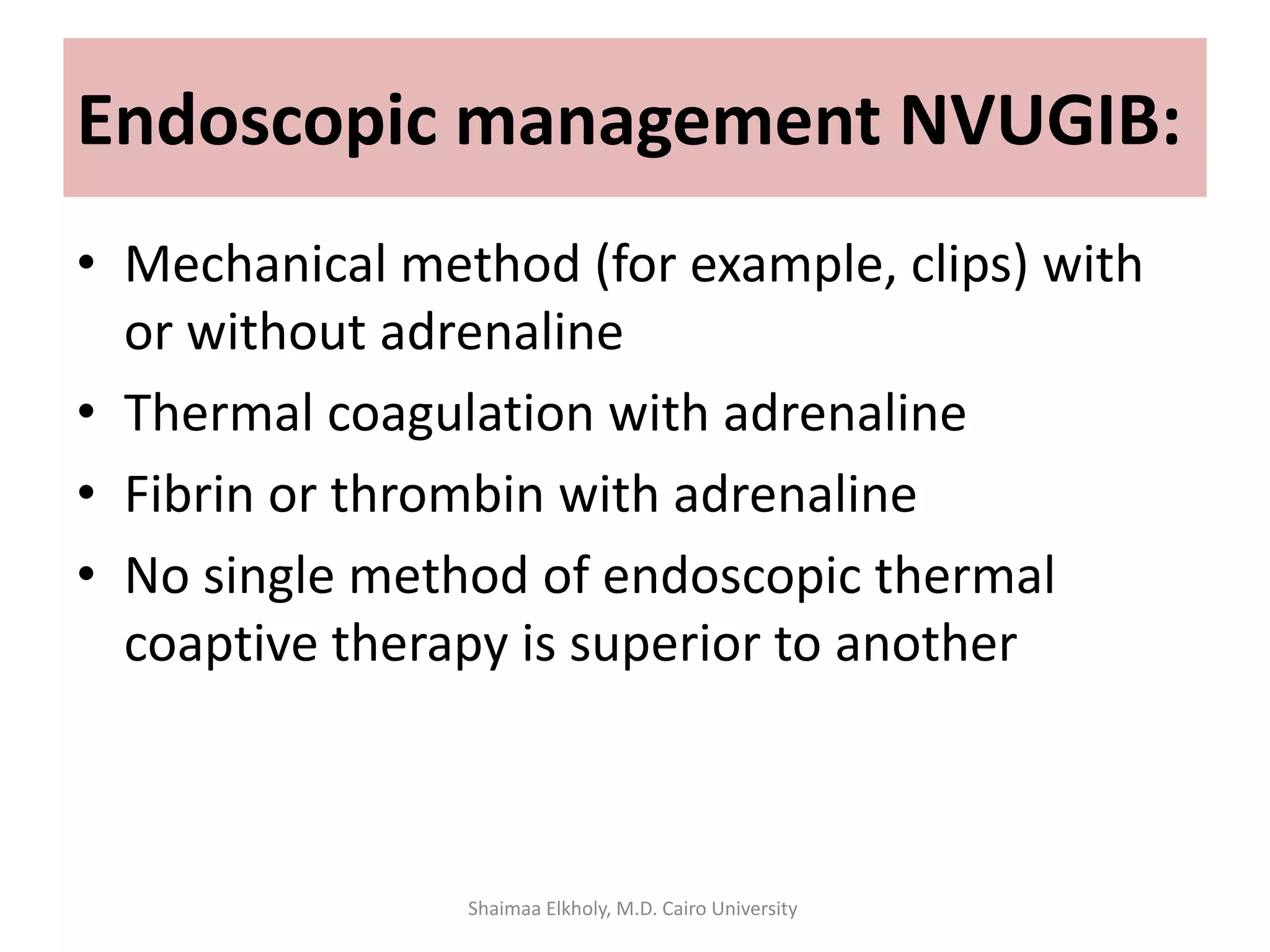
The document discusses the approach to upper gastrointestinal bleeding (UGIB), detailing its definitions, epidemiology, and management strategies. It highlights the mortality rates associated with UGIB and the common causes, primarily peptic ulcer disease and variceal hemorrhages, along with treatment protocols such as resuscitation and endoscopic interventions. Finally, it emphasizes the need for risk assessment and tailored management based on individual patient factors.