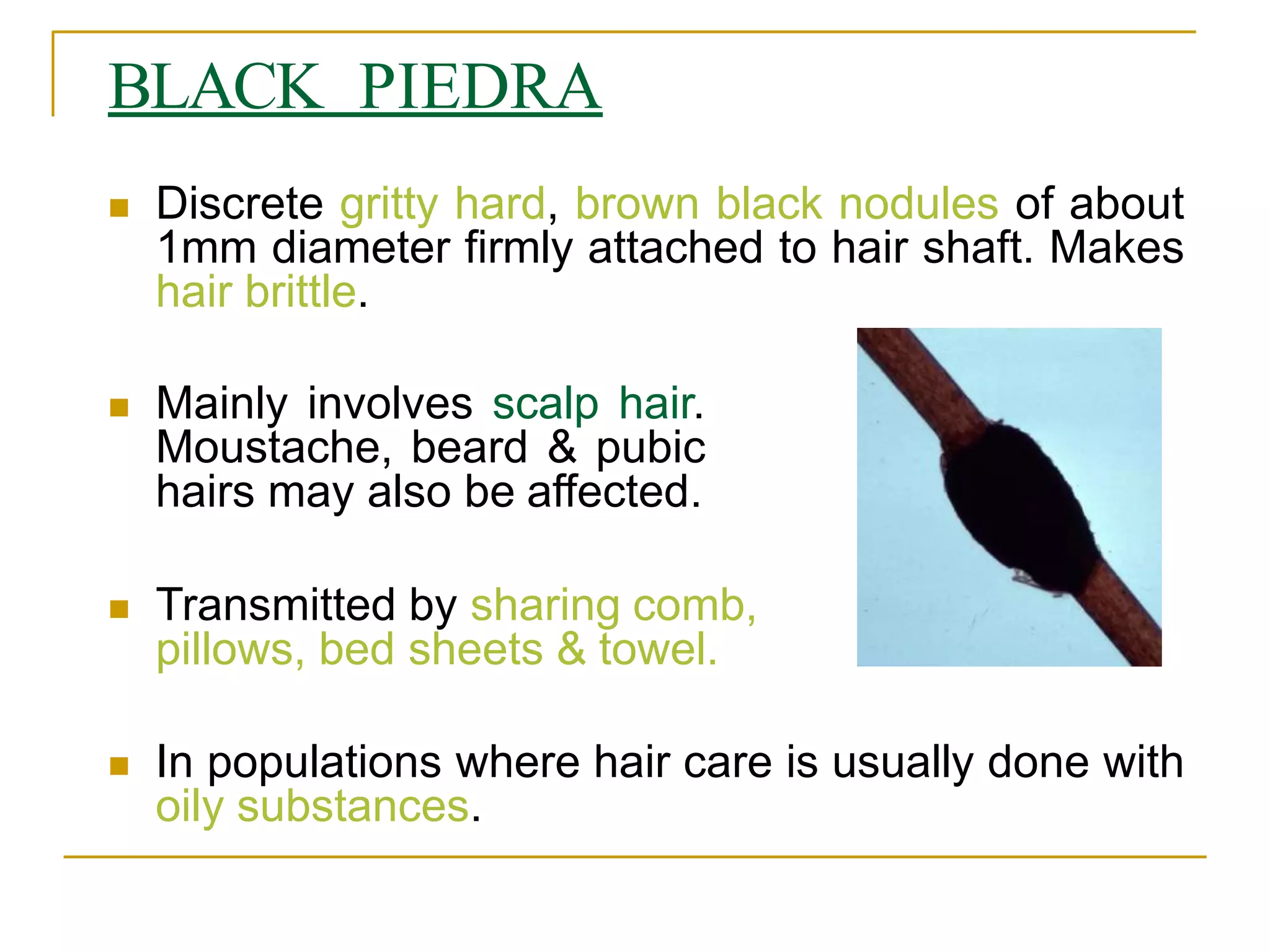
1. Superficial mycoses involve infections of the skin and its appendages by fungi including Malassezia species, dermatophytes, and others.
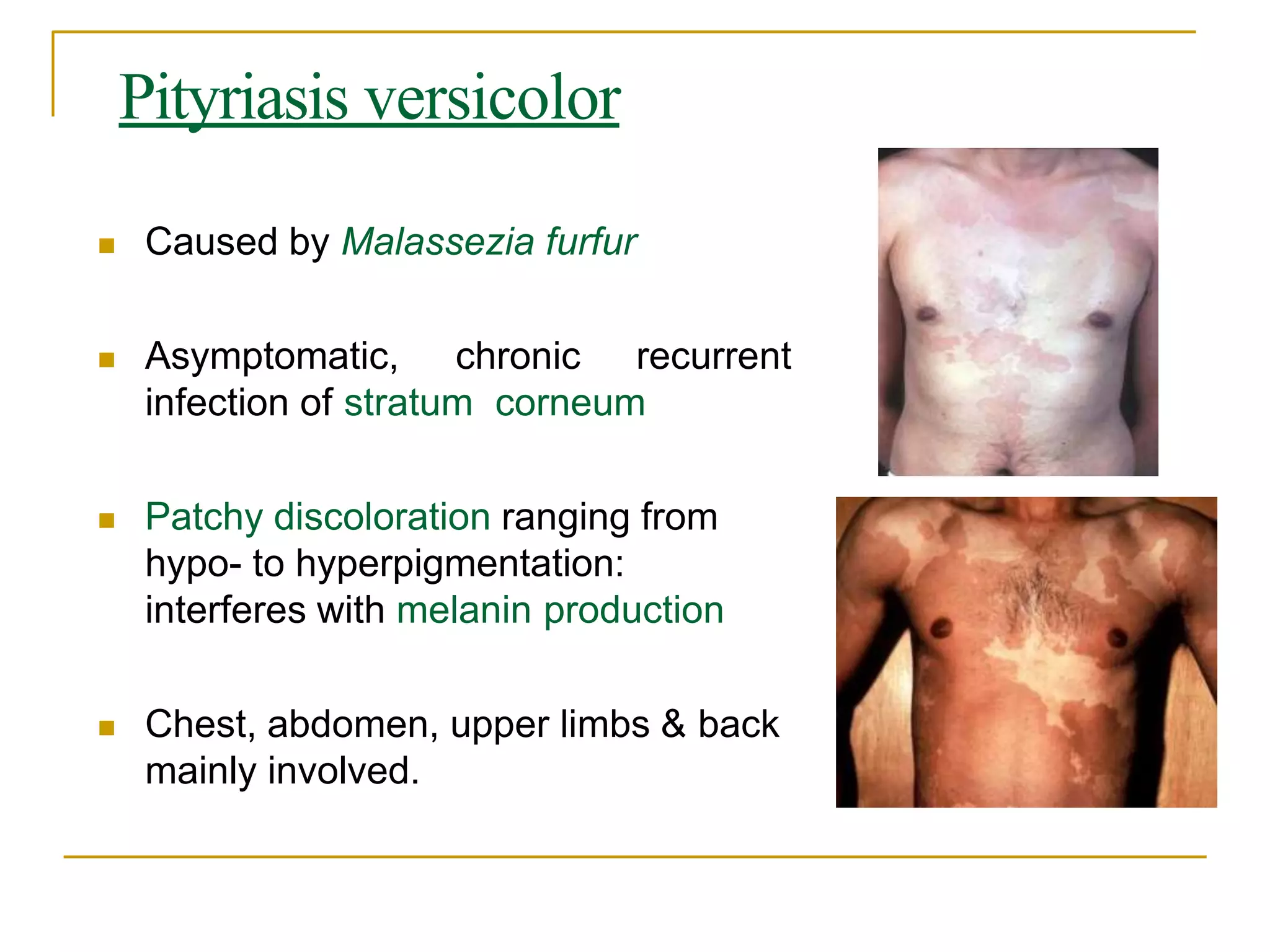
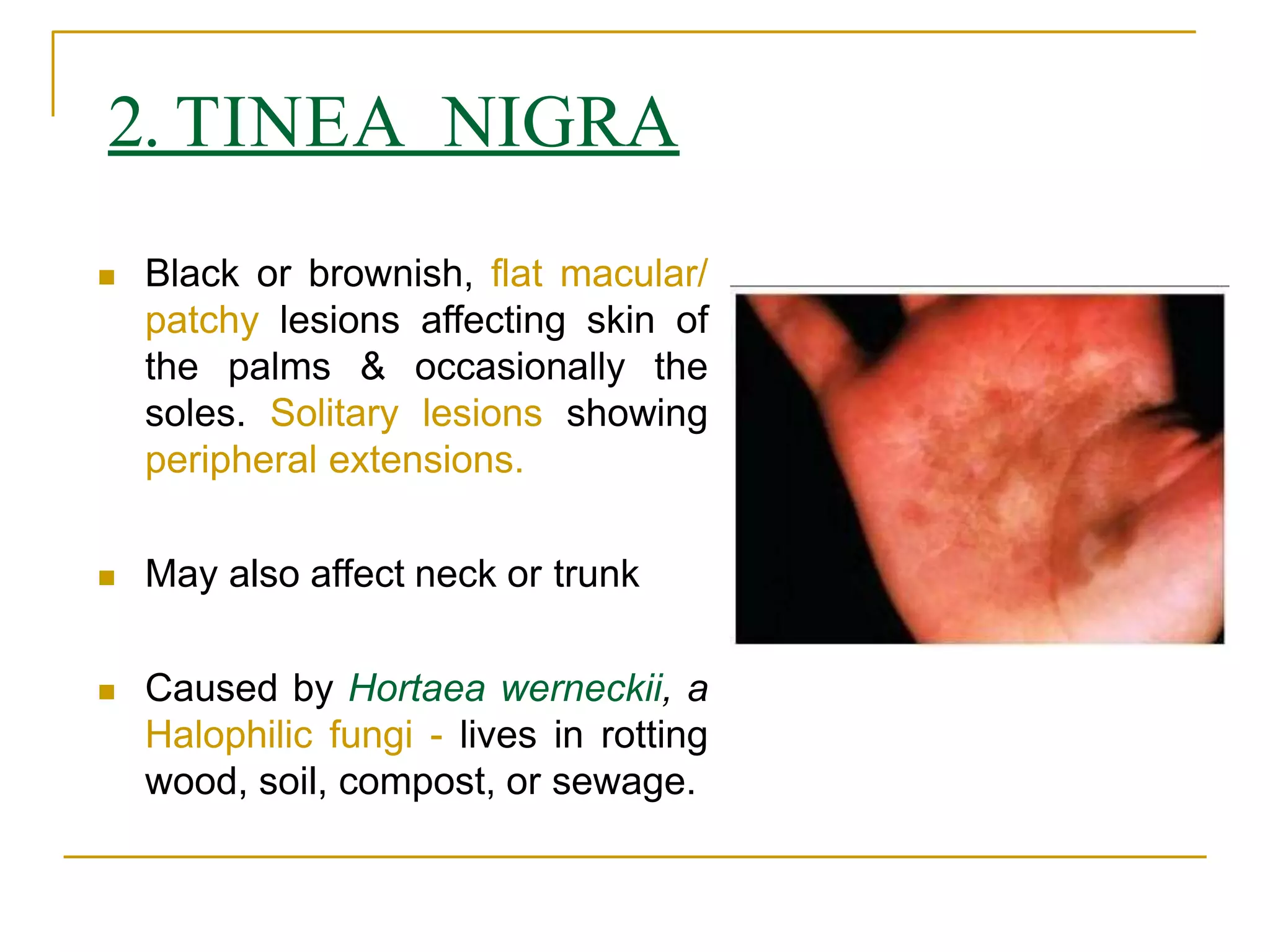
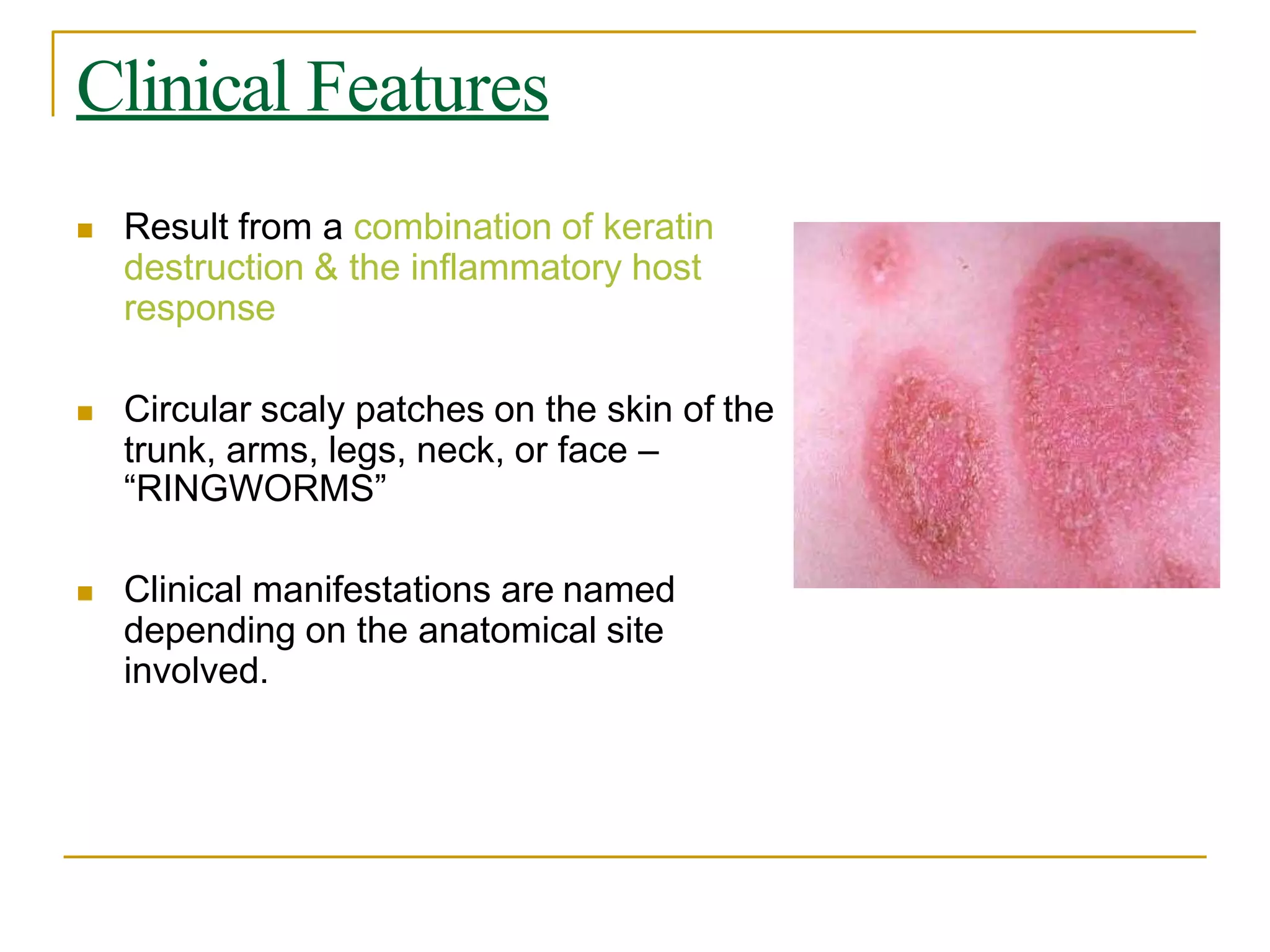
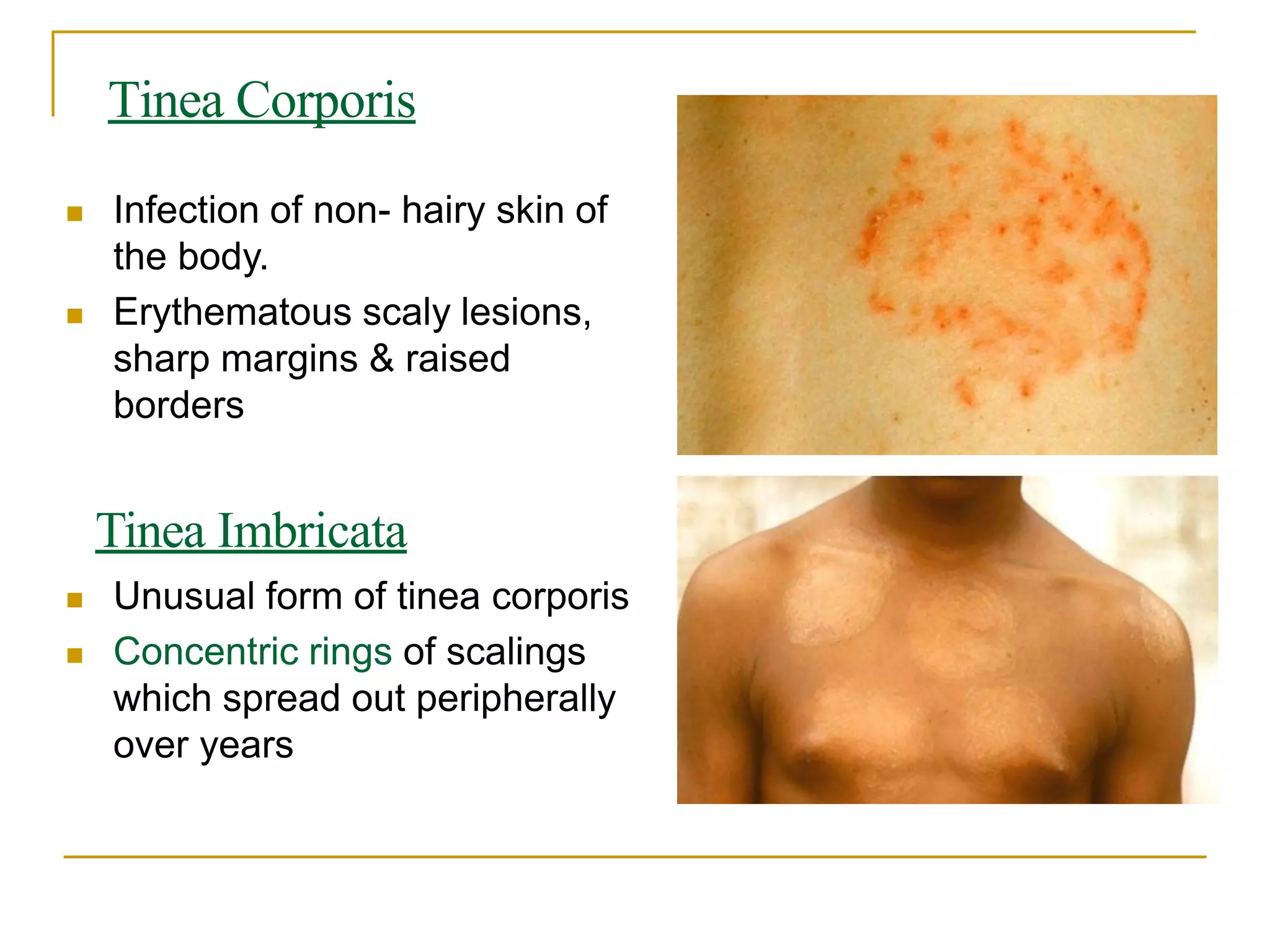
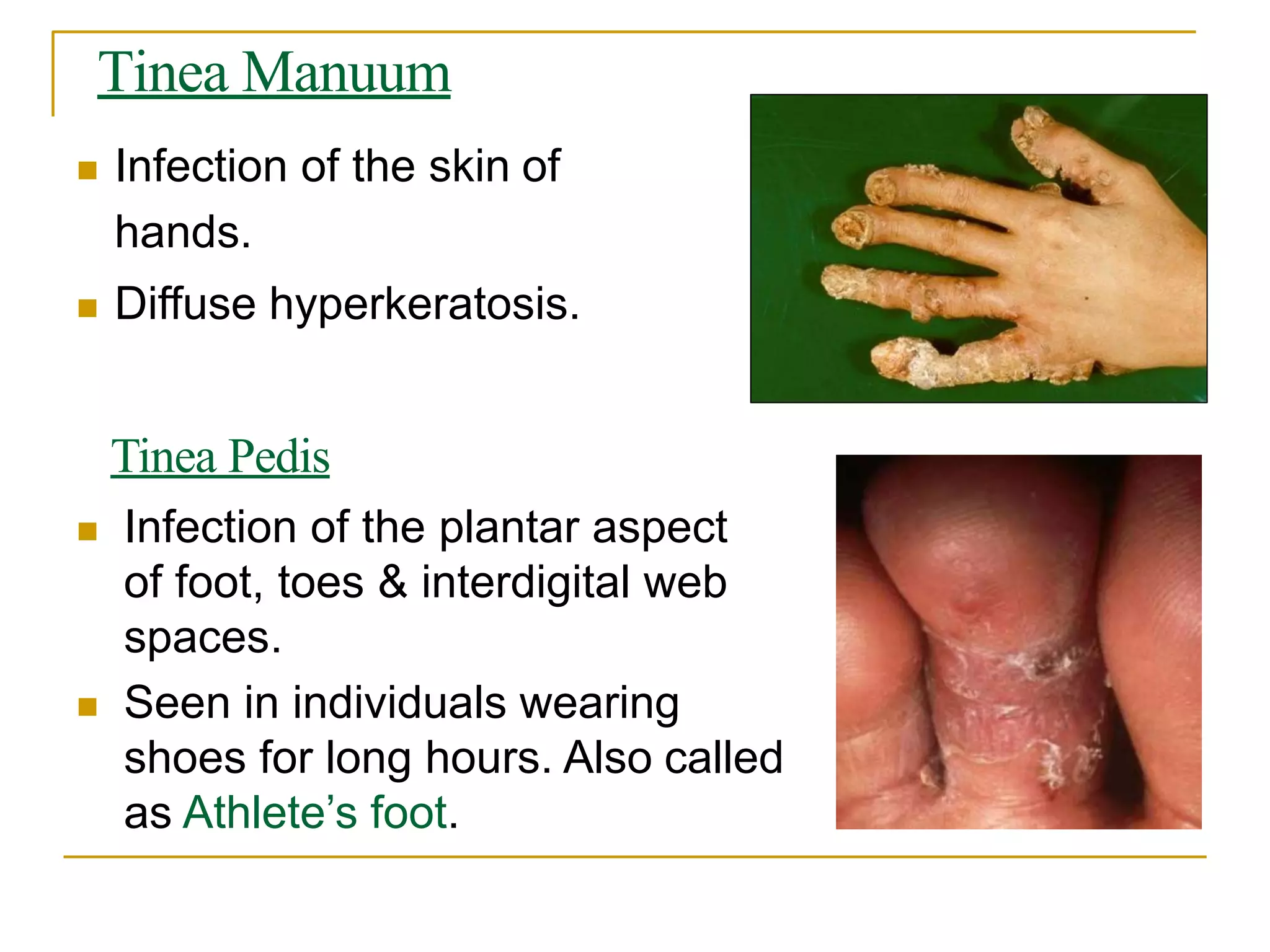
2. Common conditions include pityriasis versicolor caused by Malassezia furfur presenting as discolored patches, and tinea infections like tinea corporis caused by dermatophytes appearing as scaly rings.
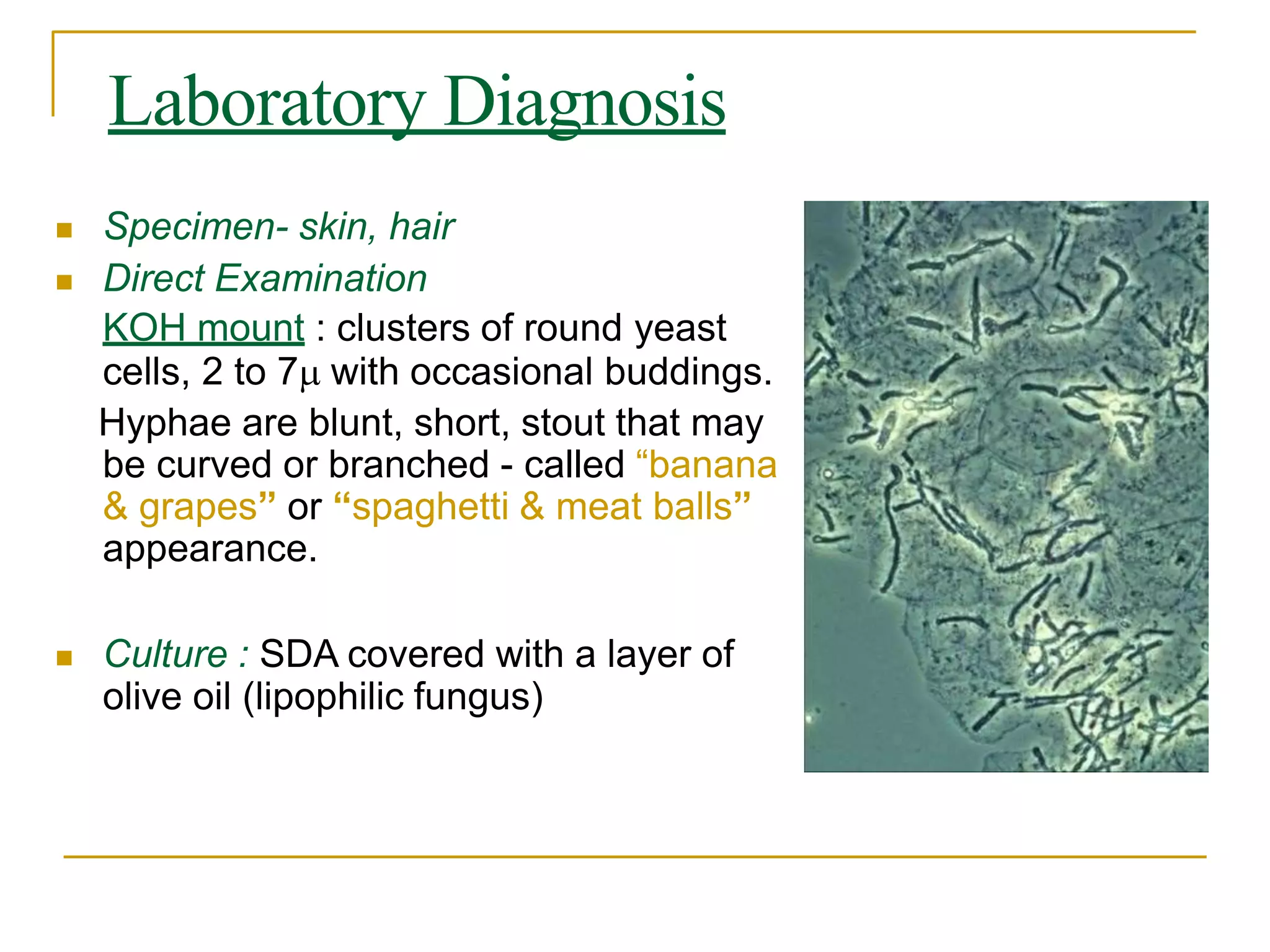
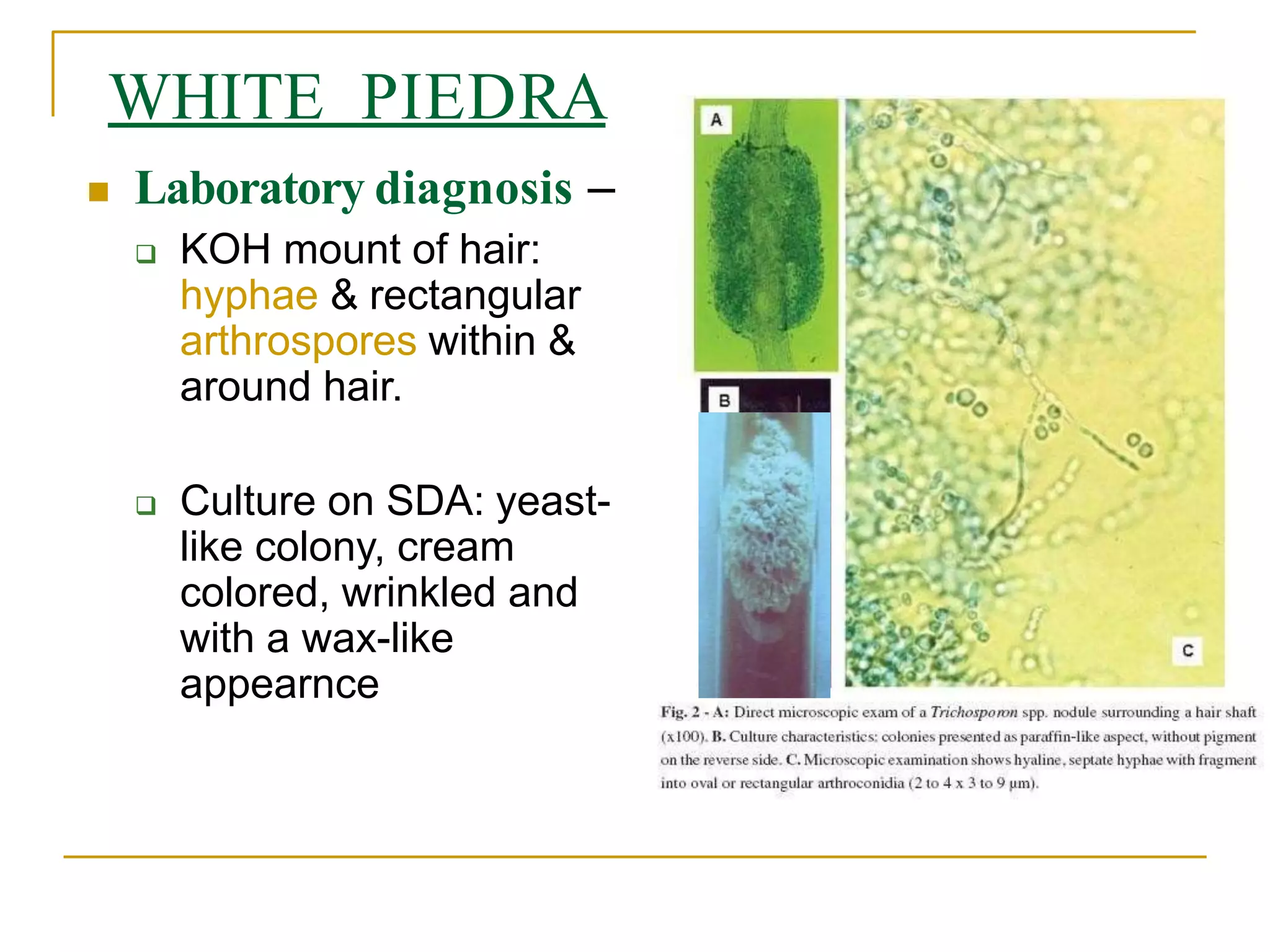
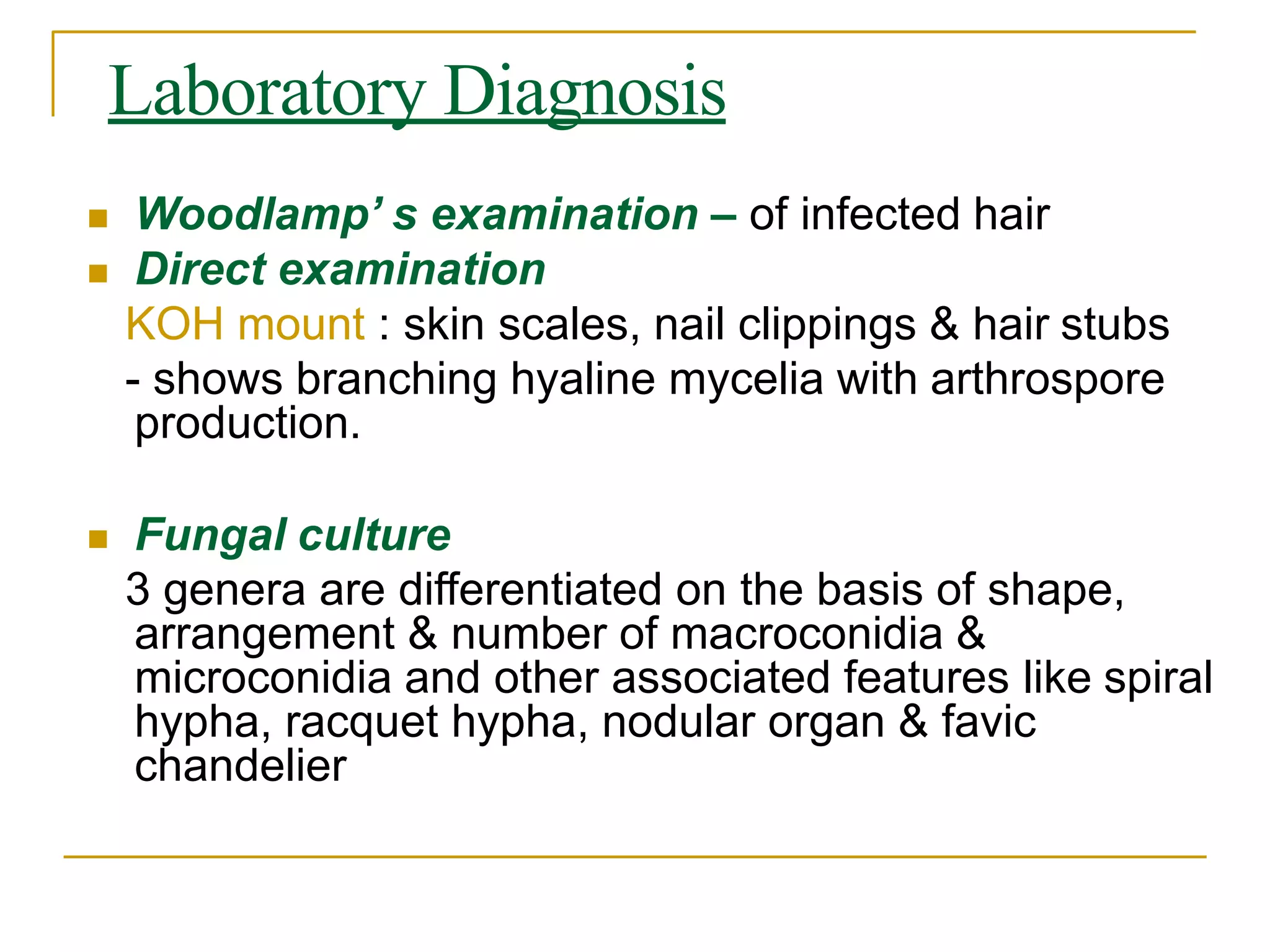
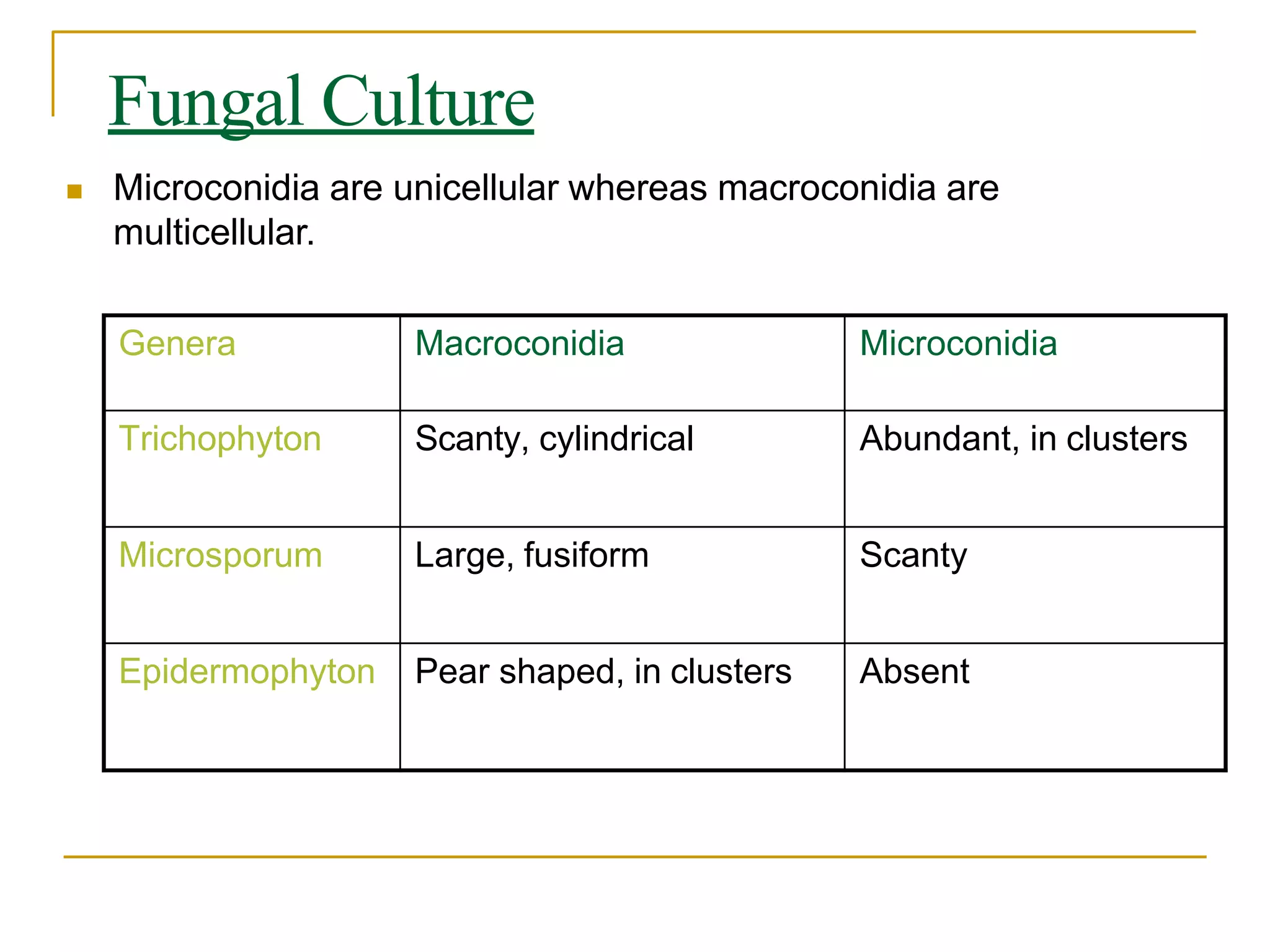
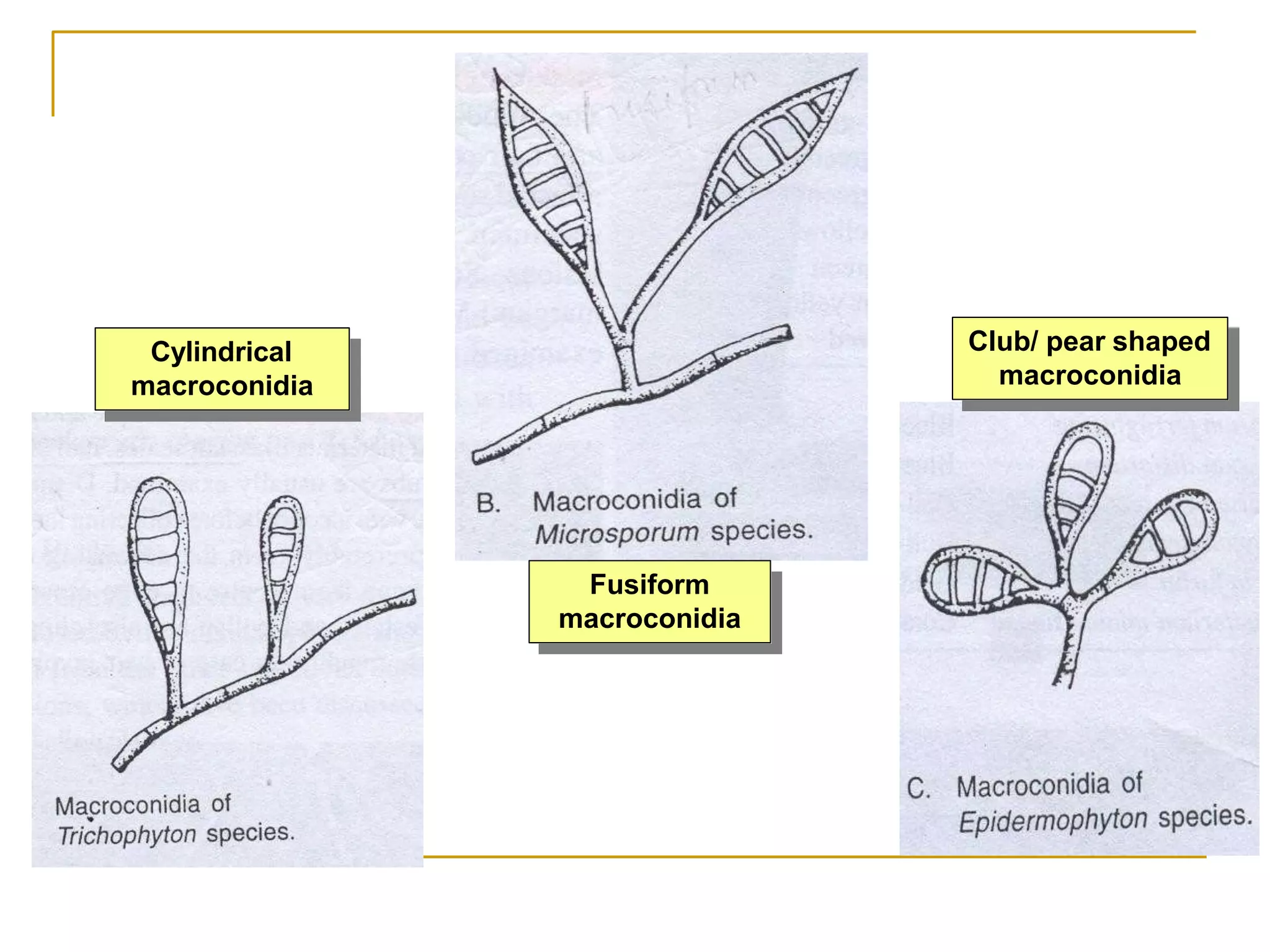
3. Laboratory diagnosis involves potassium hydroxide microscopy of skin and nail samples to visualize fungal elements, and culture to isolate and identify the causative agent. Topical and oral antifungal drugs are used for treatment.