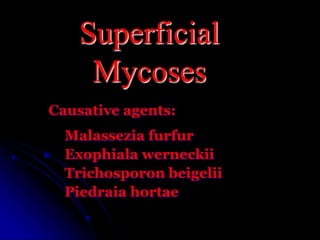
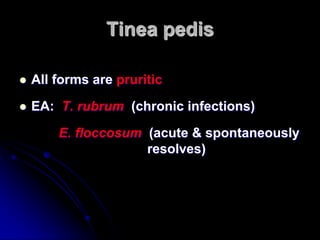
This document summarizes various fungal skin infections (dermatophytoses) caused by dermatophytes. It describes the causative fungi of superficial mycoses and outlines the clinical presentation of common dermatophytoses including tinea corporis, tinea cruris, tinea pedis, tinea manuum, tinea capitis and others. It also provides details on laboratory identification of dermatophytes through microscopic examination and fungal culture characteristics. Key identifying features of common dermatophyte genera like Trichophyton, Microsporum, and Epidermophyton are highlighted.