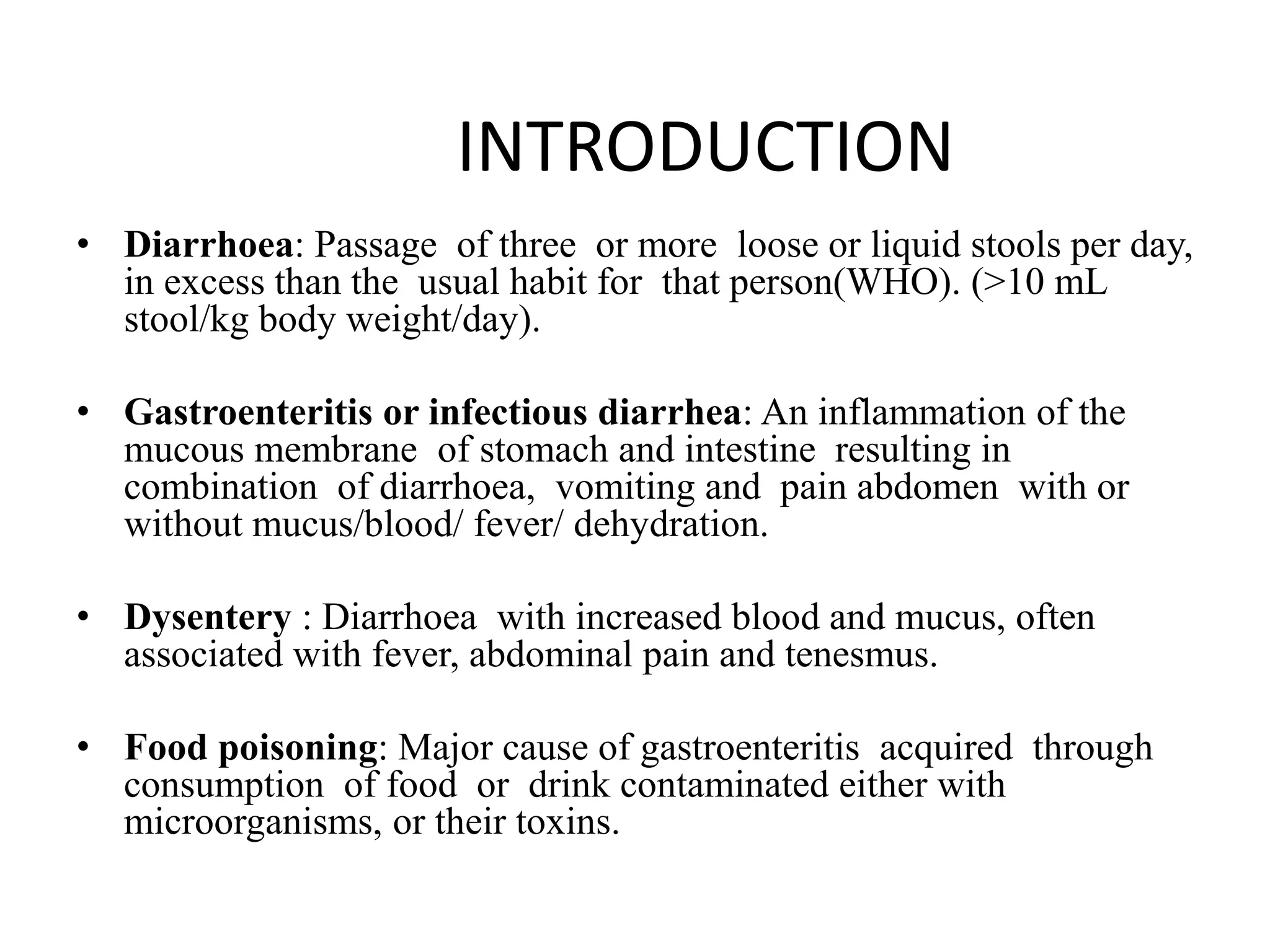
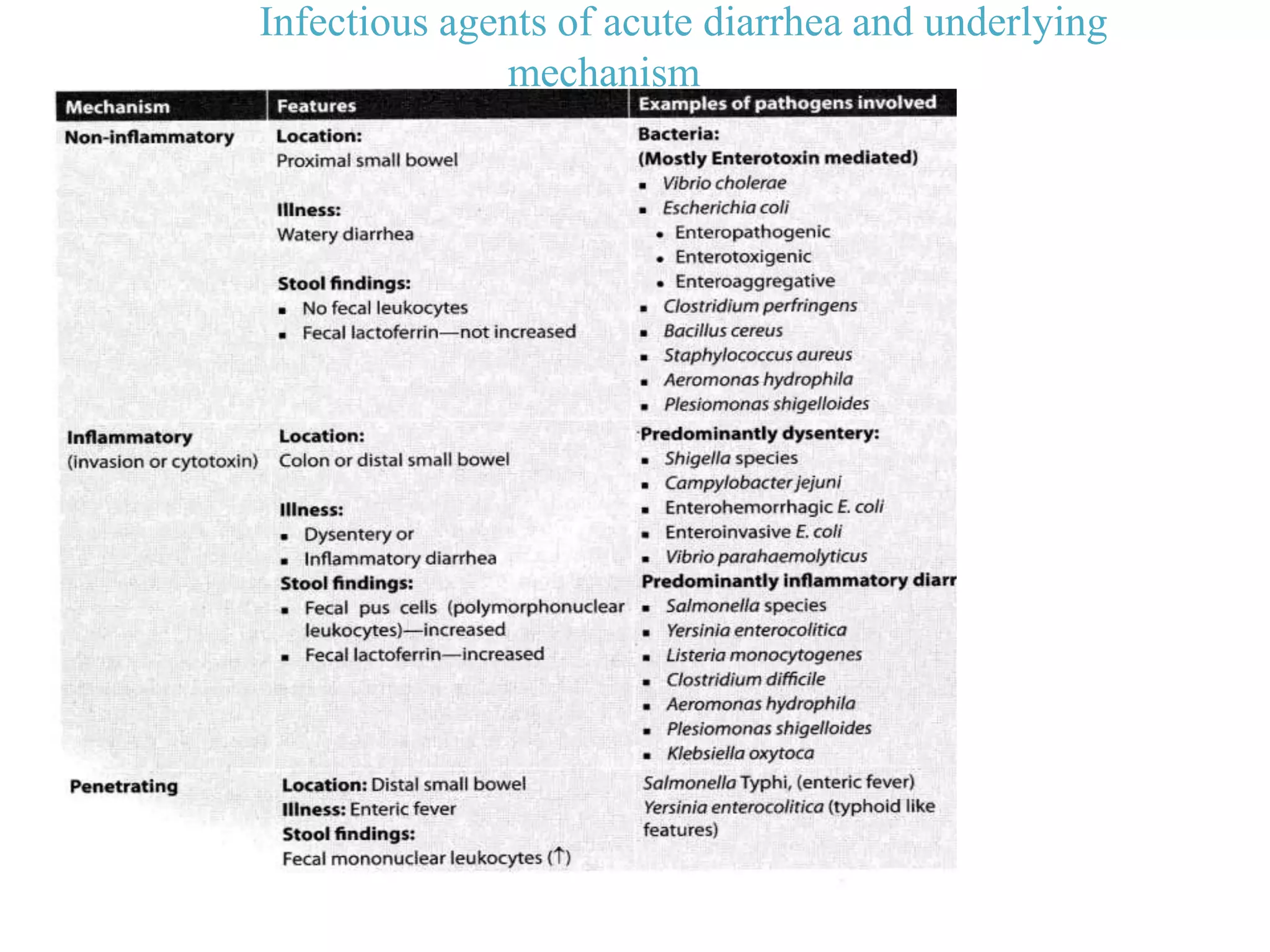
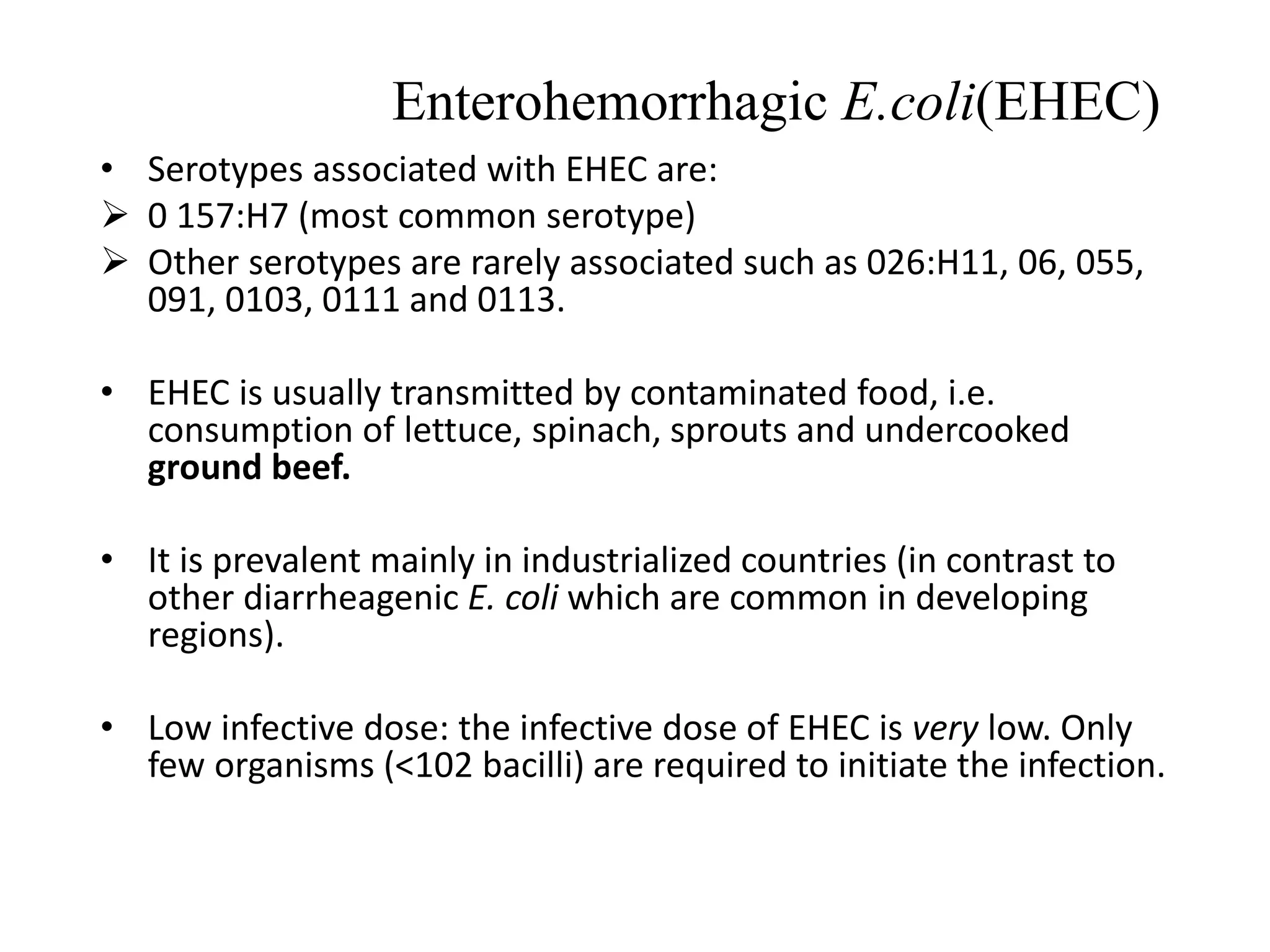
Bacterial diarrhea and dysentery can be caused by a variety of bacteria including E. coli, Vibrio cholerae, Shigella, Salmonella, Campylobacter, and Clostridium. These bacteria cause diarrhea through different mechanisms including production of enterotoxins or neurotoxins that damage intestinal cells, or through invasion and infection of the intestinal mucosa. Symptoms range from watery diarrhea to bloody diarrhea and depend on the specific bacterium. Treatment focuses on fluid replacement and antibiotics when needed.