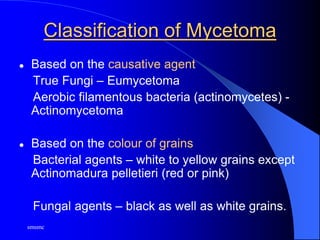
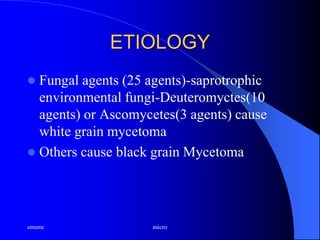
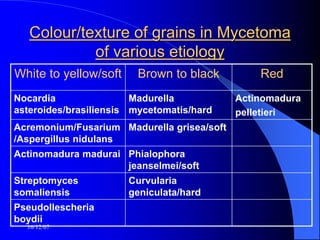
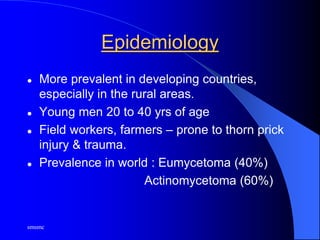
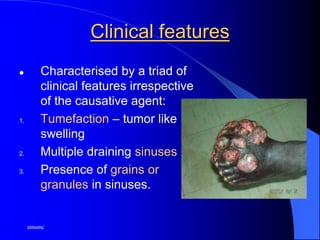
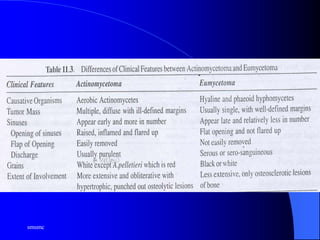
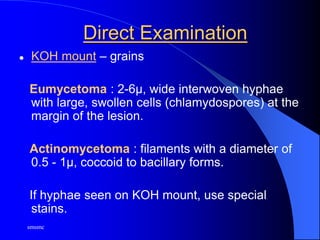
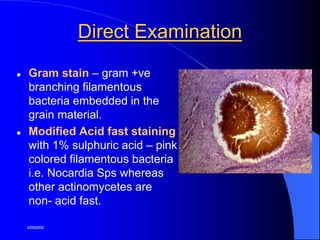
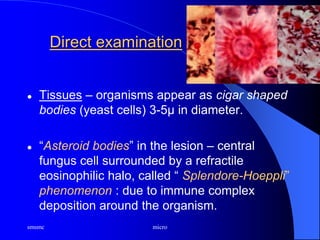
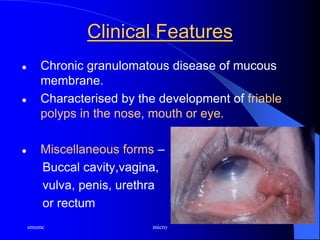
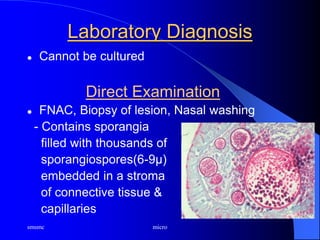
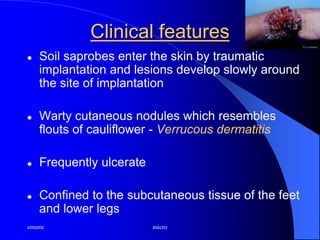
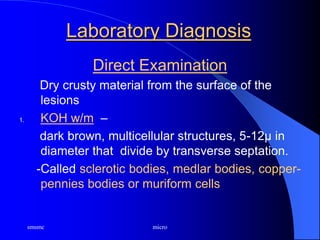
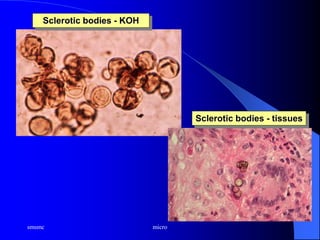
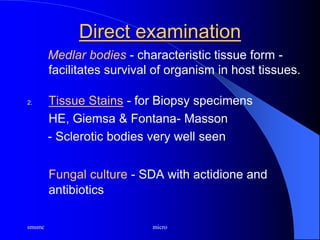
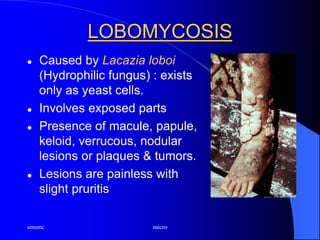
This document provides an overview of subcutaneous mycoses. It discusses several types including mycetoma, sporotrichosis, rhinosporidiosis, chromoblastomycosis, phaeohyphomycosis, and lobomycosis. For each condition, it summarizes the causative agent, clinical features, pathogenesis, diagnosis including direct examination and culture techniques, and treatment approaches. The document emphasizes that these infections usually follow trauma and develop subcutaneously at the site of inoculation, presenting with characteristic clinical features like tumefaction, draining sinuses, and presence of grains or granules.