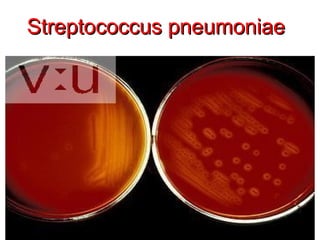
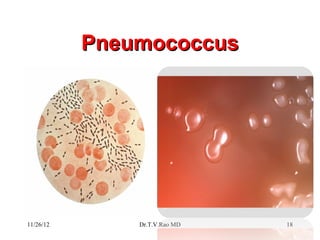
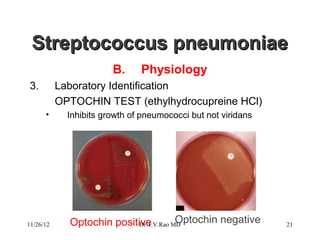
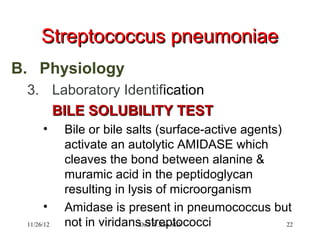
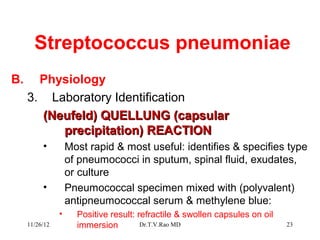
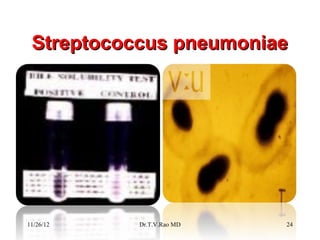
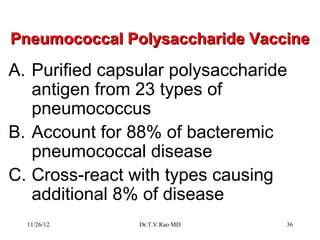
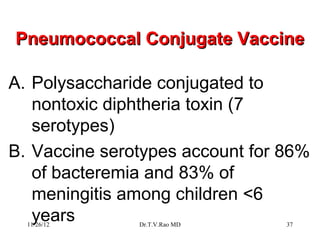
Streptococcus pneumoniae, commonly known as pneumococcus, is a Gram-positive bacterium that is a major cause of pneumonia. It has over 90 known serotypes and uses an antiphagocytic polysaccharide capsule as a main virulence factor. Identification methods include culture characteristics such as being optochin positive and bile soluble as well as serological tests like the Quellung reaction.