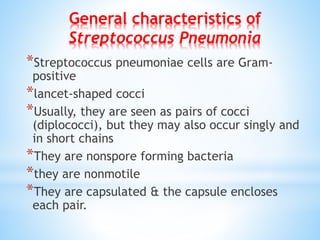
Streptococcus pneumoniae is a gram-positive bacterium that typically appears as diplococci and is characterized by its virulence factors, such as its capsule and various proteins that facilitate infection and immune evasion. It can cause diseases including pneumonia, meningitis, and bacteremia, with transmission occurring through respiratory droplets. Treatment options vary based on antibiotic resistance, with penicillin being the drug of choice for sensitive strains and alternatives like third-generation cephalosporins or vancomycin for resistant cases.