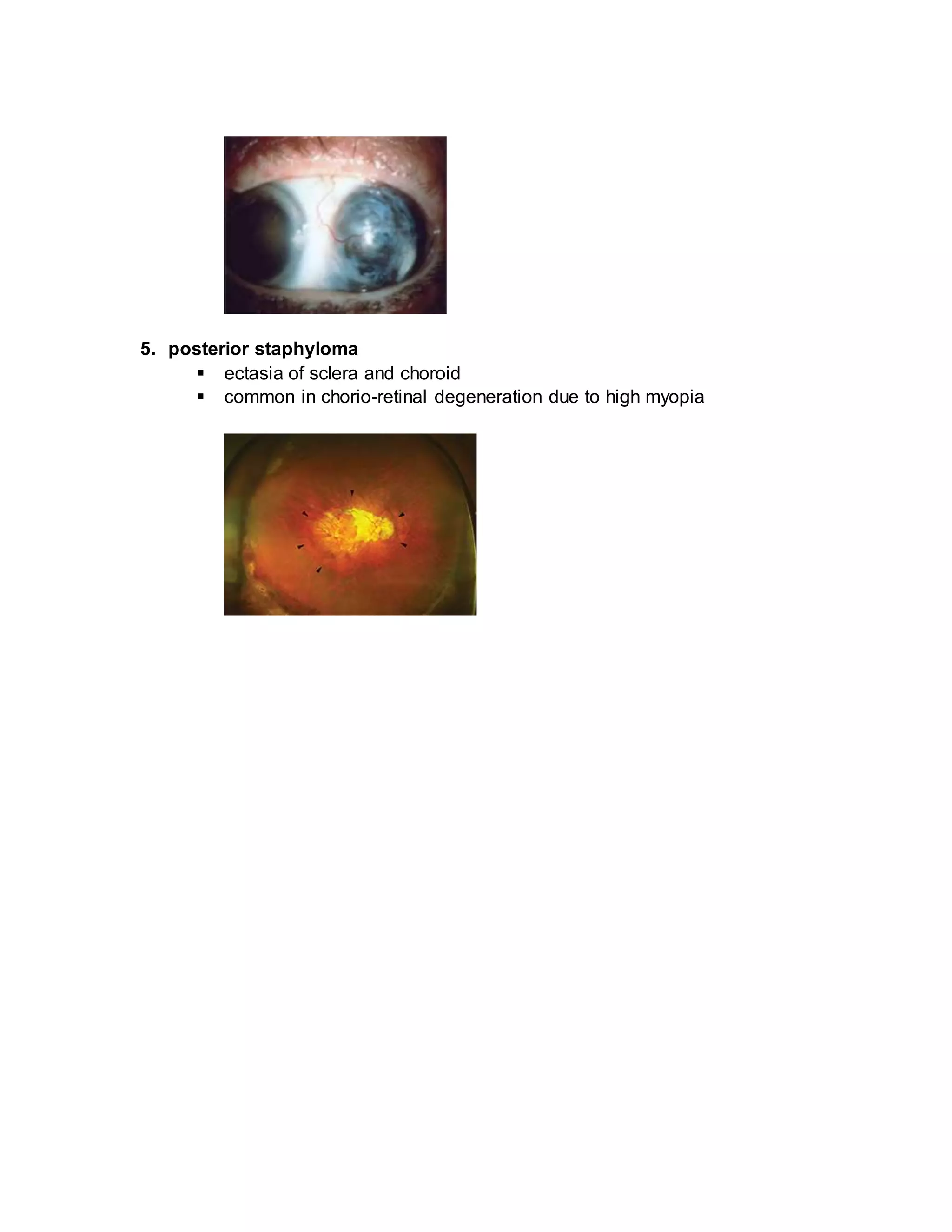
The document discusses the anatomy and conditions related to the sclera, including types of scleritis and episcleritis, as well as staphyloma. It highlights the sclera's role in maintaining eye shape, its vascularization, and its response to various diseases. Additionally, it categorizes the types, symptoms, and pathologies associated with these conditions, emphasizing their prevalence and clinical implications.