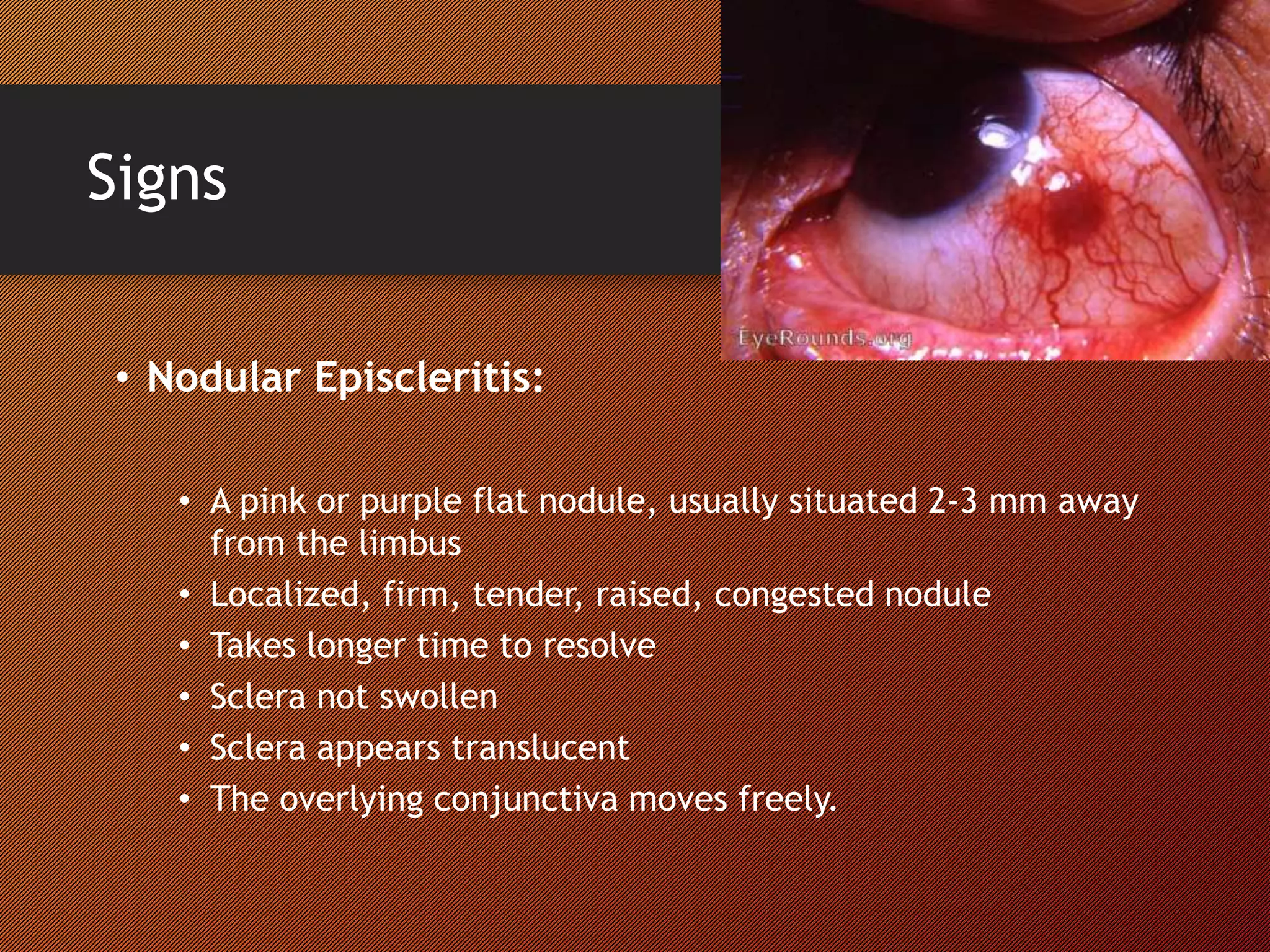
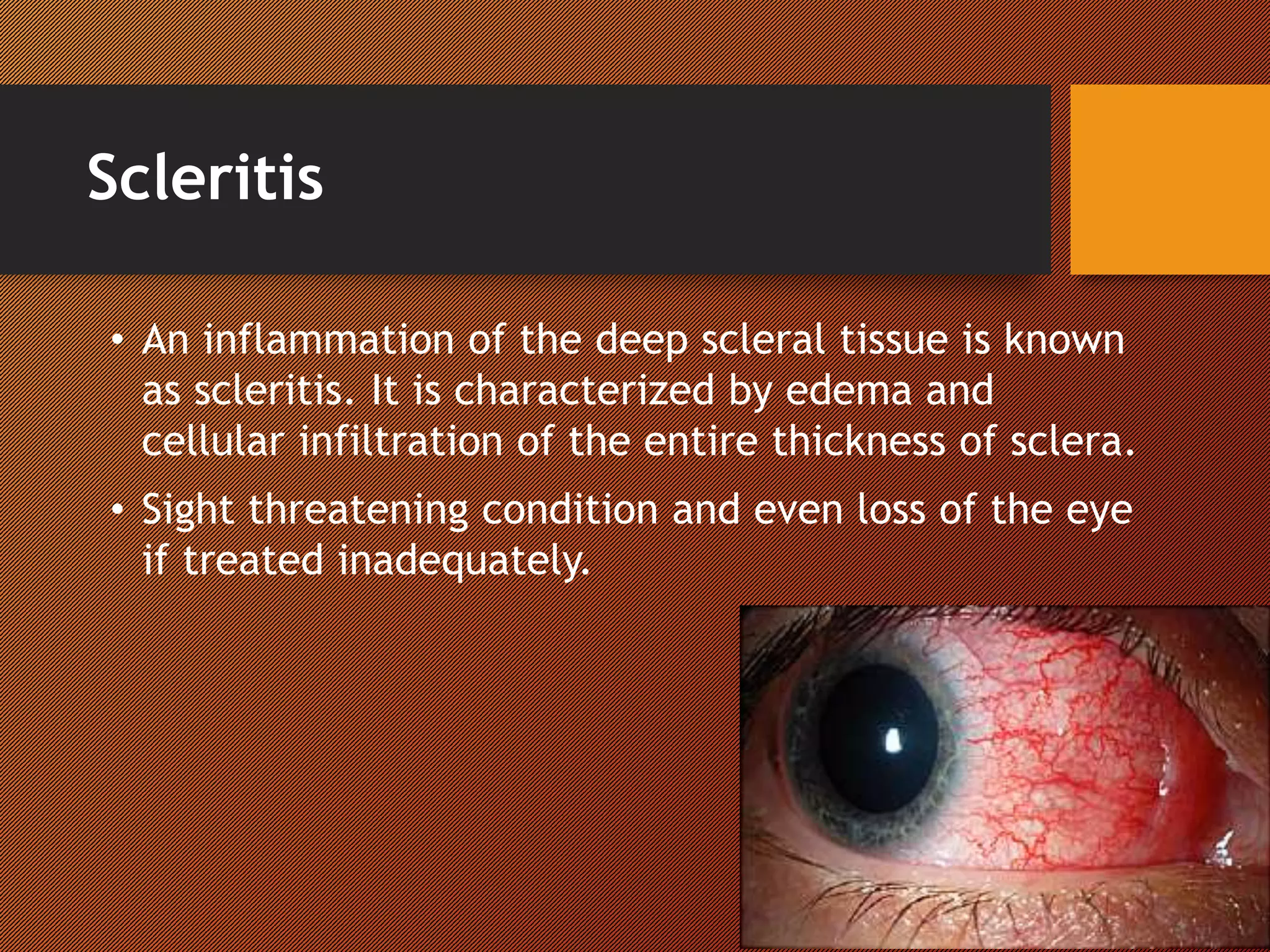
The document discusses two types of scleral inflammation: episcleritis, which is generally benign and self-limiting, and scleritis, which can be sight-threatening. Episcleritis typically affects younger adults with symptoms like localized redness and mild pain, while scleritis is associated with autoimmune diseases and leads to more severe symptoms and complications. Treatment for episcleritis may be minimal, whereas scleritis requires more aggressive therapies, including corticosteroids and immunosuppressants.