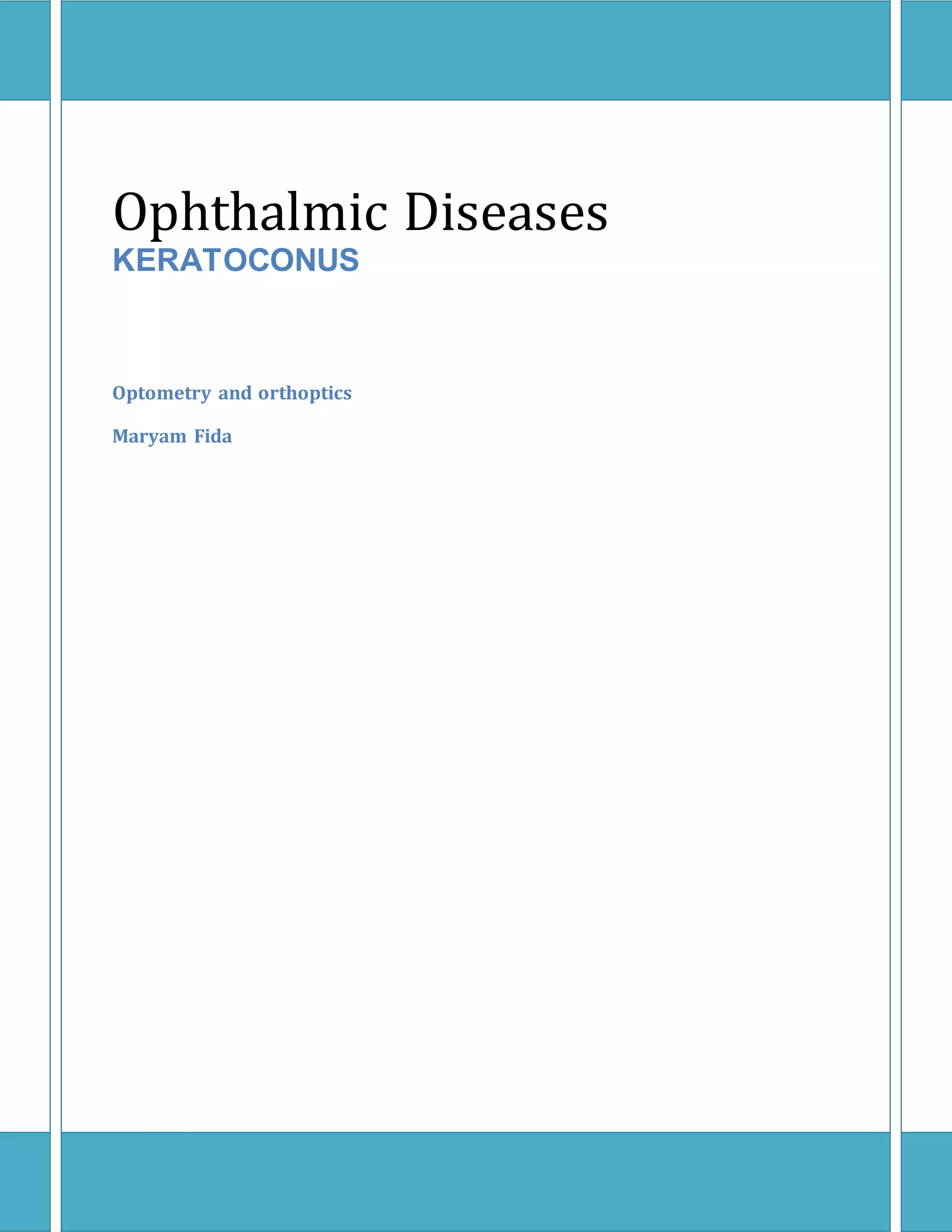
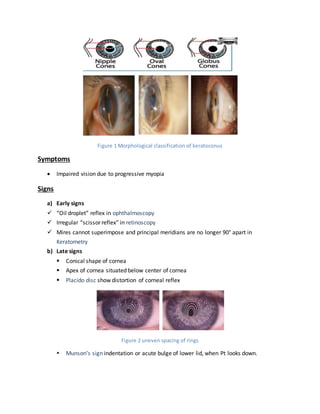
Keratoconus is a progressive, bilateral thinning of the cornea typically seen in girls during puberty, leading to symptoms such as blurry vision and astigmatism. It can be classified based on keratometry and morphology, with notable signs observable through various eye examination techniques. Diagnosis involves patient history, familial assessment, and specialized tests like topography and keratoscopy.