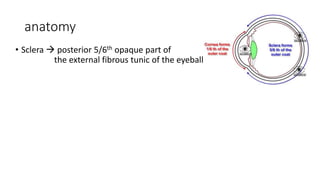
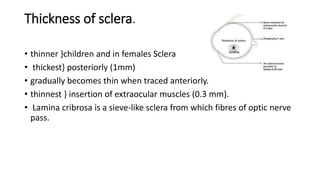
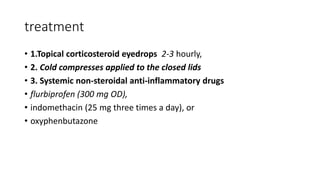
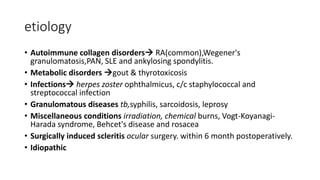
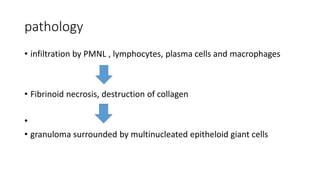
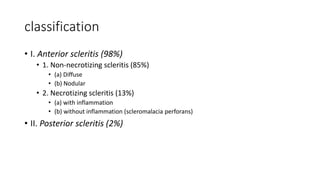
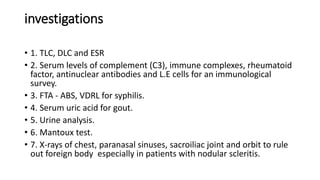
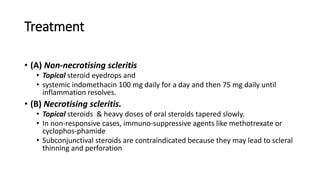
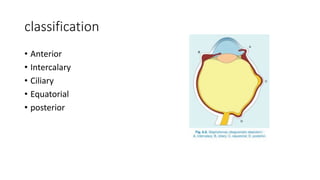
The document discusses diseases of the sclera, focusing on its anatomy, layers, inflammation types (episcleritis and scleritis), symptoms, complications, and treatment options. It describes the differences between various forms of scleritis, their etiology, typical symptoms, and necessary diagnostic procedures, emphasizing the importance of timely treatment. Additionally, it addresses conditions like blue sclera and staphylomas, outlining their characteristics and associated risks.