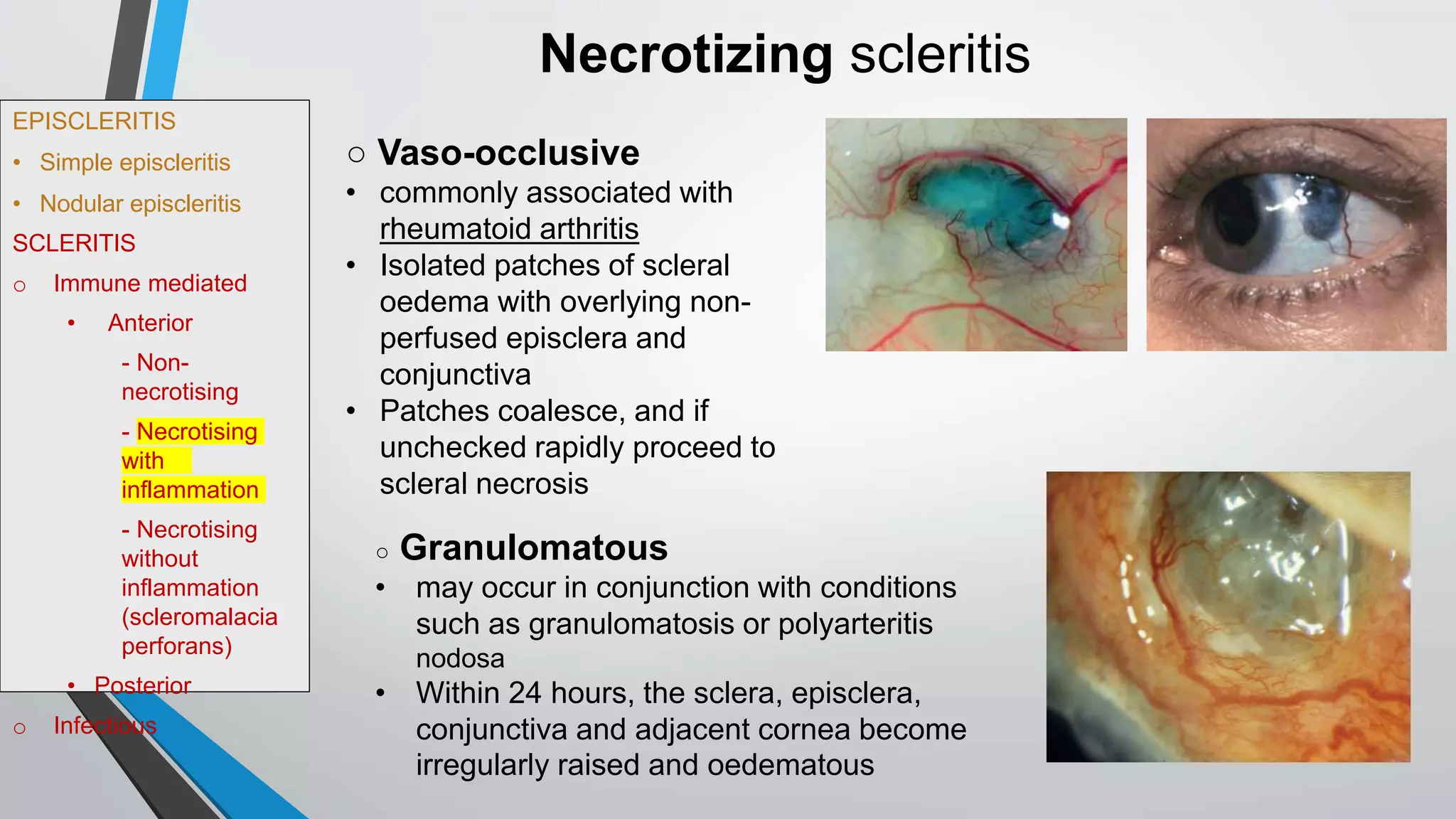
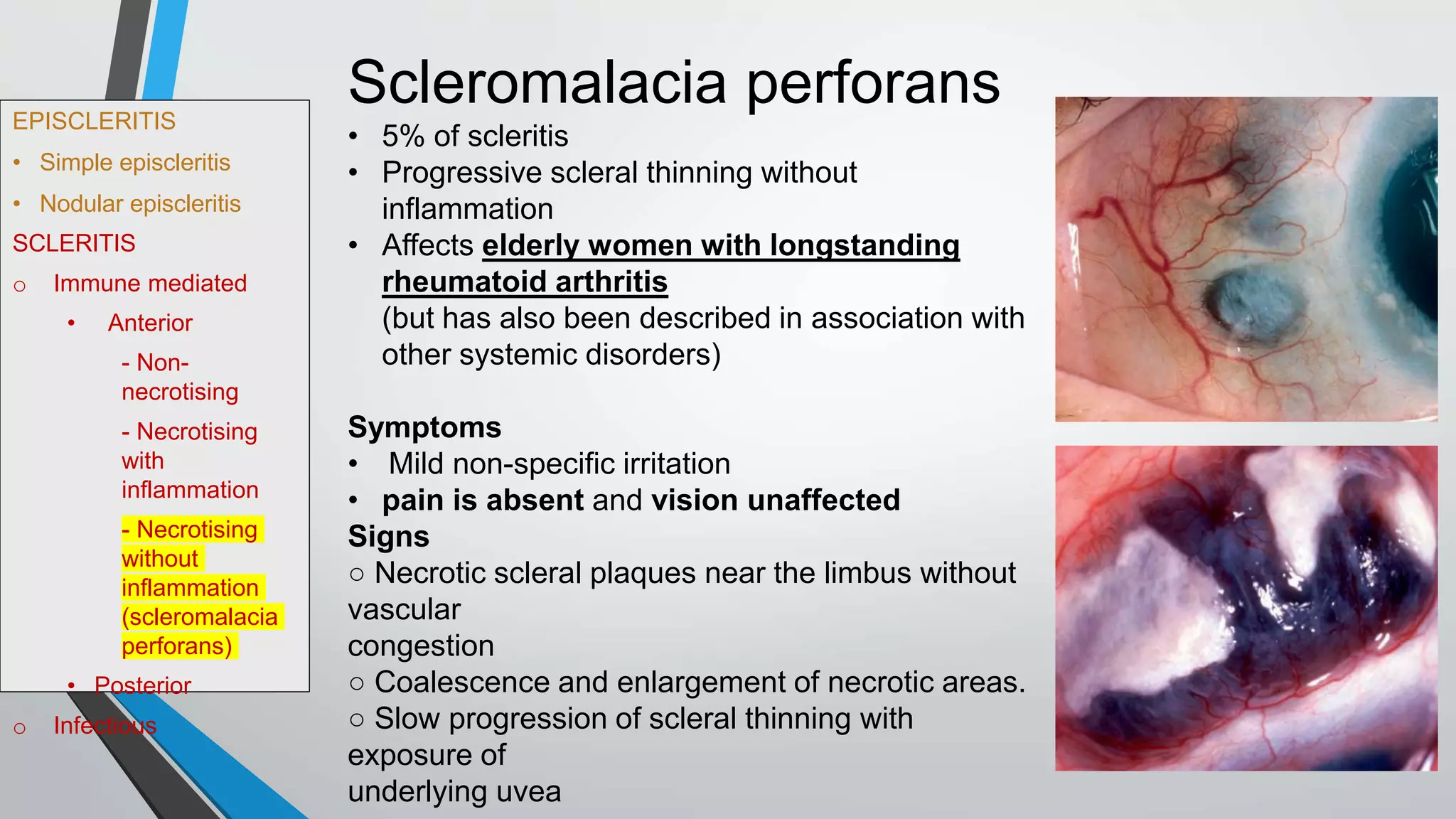
The document discusses diseases of the sclera, including episcleritis and scleritis. Episcleritis is a benign inflammation of the outer layer of the eyeball that comes in two forms - simple and nodular. Scleritis is a deeper inflammation that involves the entire thickness of the sclera. Scleritis can be immune-mediated, infectious, or necrotizing. Treatment depends on the type but may include topical steroids, NSAIDs, or systemic steroids and immunosuppressive drugs.






































![EPISCLERITIS
• Simple episcleritis
• Nodular episcleritis
SCLERITIS
o Immune mediated
• Anterior
- Non-
necrotising
- Necrotising
with
inflammation
- Necrotising
without
inflammation
(scleromalacia
perforans)
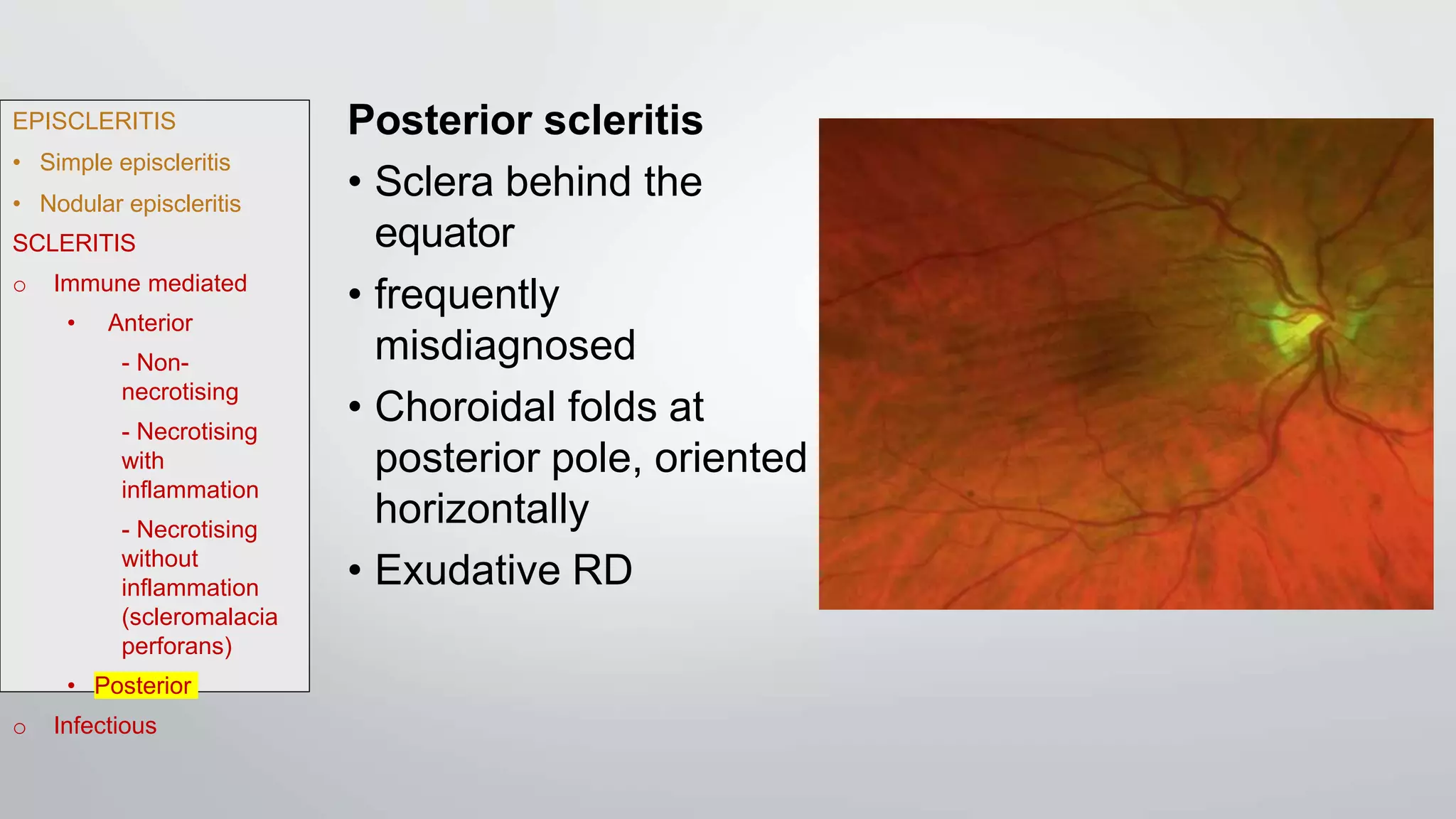
• Posterior
o Infectious
• Topical steroids - do not affect the natural history of the scleral
inflammation, but may relieve symptoms and oedema in non-necrotizing
disease
• Systemic NSAIDs should be used alone only in non-necrotizing disease
• Periocular steroid injections may be used in non-necrotizing disease
but their effects are usually transient; [contraindicated in necrotizing
scleritis]
• Systemic steroids (e.g. prednisolone is 1–1.5 mg/kg/day) are used
when NSAIDs are inappropriate or inadequate (necrotizing disease).
Intravenous methylprednisolone may be used for emergent cases.
• Immunosuppressives and/or biological blockers - if control is
incomplete with steroids alone, as a steroid-sparing measure
cyclophosphamide, azathioprine, methotrexate, ciclosporin, tacrolimus and
others;
Treatment of immune-mediated scleritis](https://image.slidesharecdn.com/diseasesofscleraeyeamnikhil-221006171741-f8ceb9cc/75/Diseases-of-sclera-43-2048.jpg)


