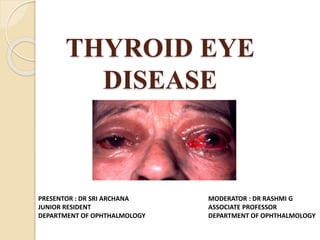
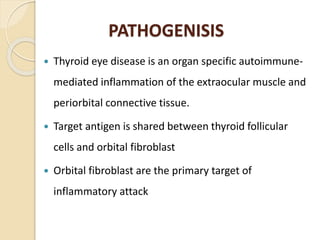
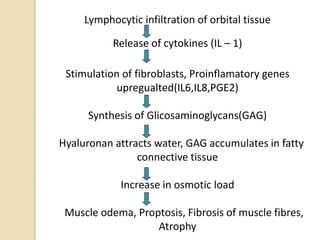
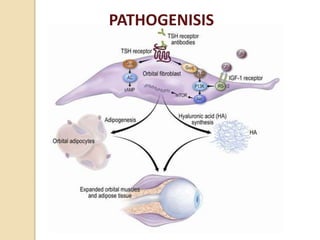
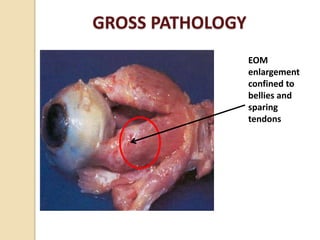
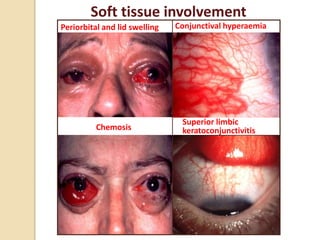
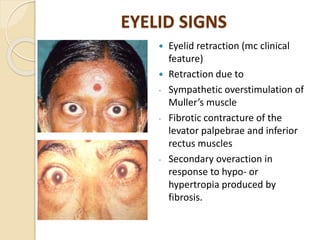
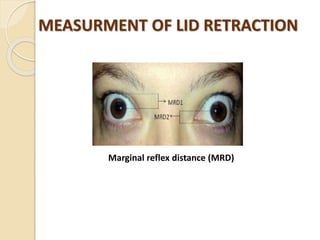
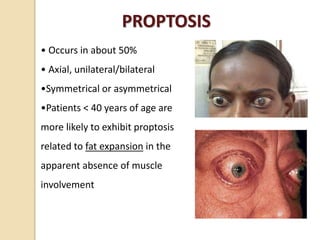
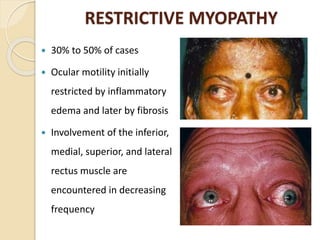
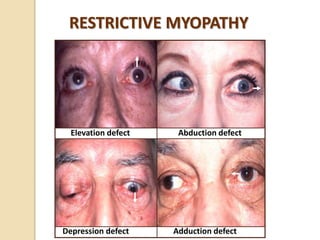
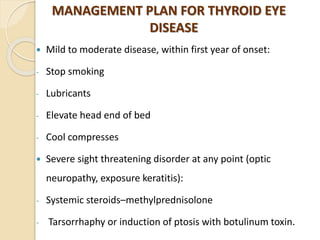
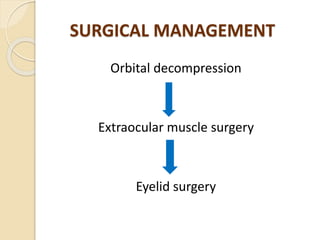
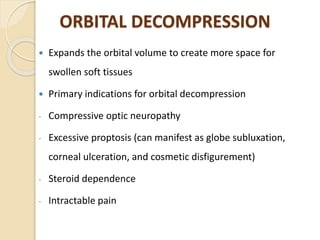
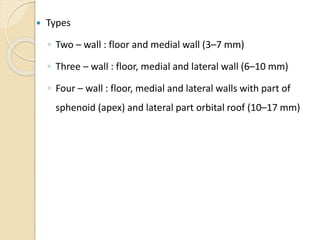
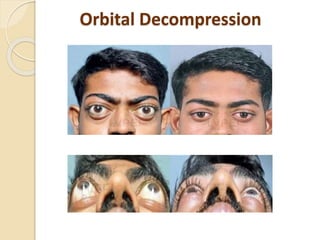
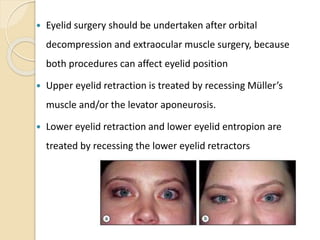
Thyroid eye disease (TED) is an autoimmune inflammatory disorder affecting the eye muscles and surrounding tissues. It is commonly associated with Graves' disease. Symptoms include eye pain, swelling of eyelids, and issues with eye movement. Examination may reveal eyelid retraction, proptosis, and restrictive myopathy. Management involves medications like steroids to reduce inflammation during active phases, with surgery to correct eye muscle issues and proptosis during inactive phases. The goal is to improve symptoms, eye health, and appearance.