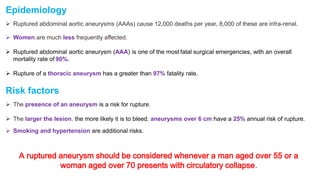
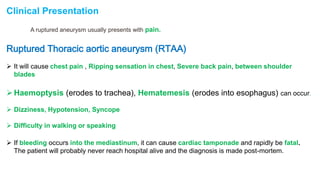
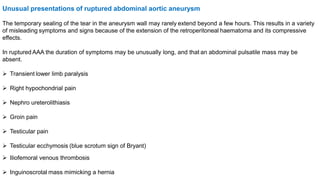
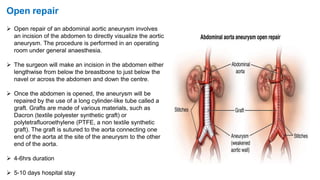
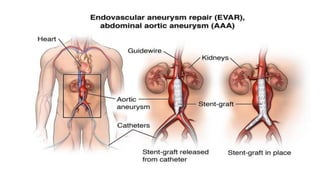
The document discusses ruptured aneurysms of the aorta, specifically focusing on ruptured abdominal aortic aneurysms (RAAAs). It describes the typical presentation of RAAAs, which includes abdominal or back pain, hypotension, and the potential presence of a pulsatile abdominal mass. It notes that RAAAs have a high mortality rate if not treated emergently through open repair or potentially endovascular aneurysm repair (EVAR). Unusual presentations of RAAAs are also discussed, which can include symptoms like leg paralysis or groin/testicular pain that mimic other conditions and delay diagnosis.