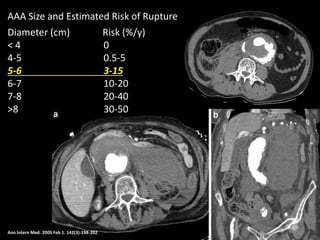
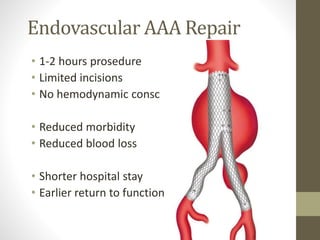
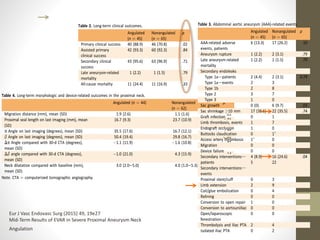
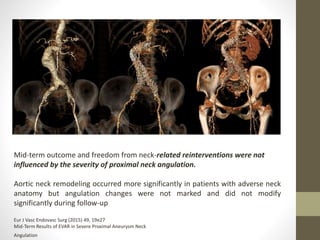
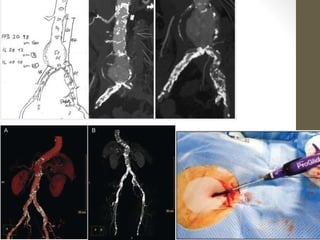
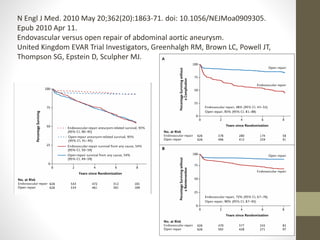
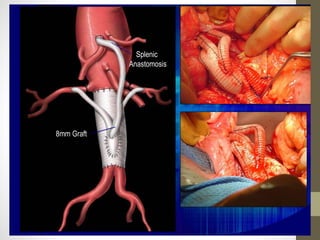
The document discusses the evolution of abdominal aortic aneurysm (AAA) repair techniques from open surgical methods to endovascular aneurysm repair (EVAR), emphasizing changes in patient management and survival outcomes. It highlights the reduced operative mortality and complications associated with EVAR, while also noting higher long-term risks of reintervention and graft-related issues compared to open repair. Ultimately, the shift in surgical practices raises concerns about training and proficiency in traditional techniques amidst increasing complexity in open repairs.