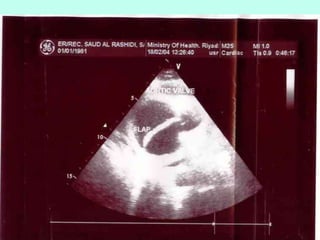
1) Aortic dissection is a tear in the inner layer of the aorta that allows blood to flow between the layers of the aortic wall, creating a false passageway. It was first documented in King George II of England in 1760.
2) Symptoms include a sudden, severe chest pain that can radiate to the back. Diagnosis is often challenging, but can be made through imaging like CT, MRI, or TEE ultrasound.
3) Type A dissections involving the ascending aorta require emergency surgery, while Type B dissections of the descending aorta can sometimes be treated medically to reduce blood pressure. Without treatment, mortality is high within the first few weeks.