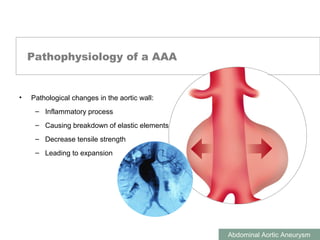
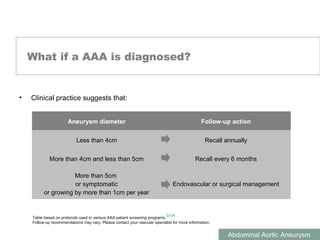
This document discusses abdominal aortic aneurysms (AAAs). It notes that Albert Einstein died from an AAA, which affects over 700,000 people in Europe. AAAs are a silent killer as they often show no symptoms. The main risk factors are being male, smoking history, hypertension, family history, and increasing age. Ultrasound is an effective way to diagnose AAAs. If left untreated, AAAs over 5cm have a high risk of rupture. Small AAAs under 4cm should be monitored annually, while larger AAAs may require surgical or endovascular treatment.