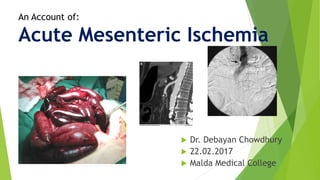
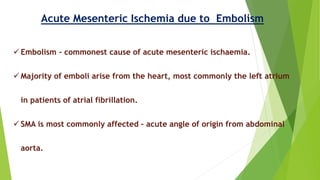
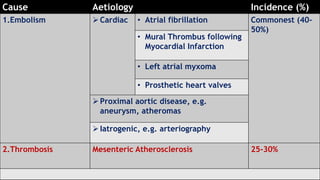
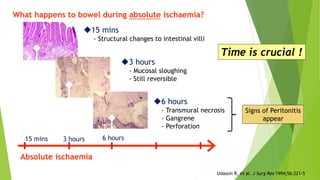
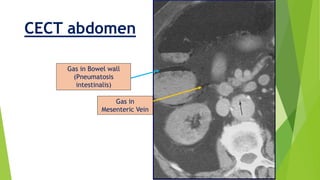
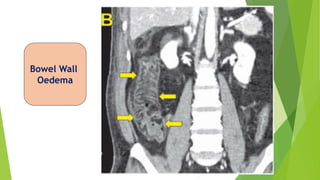
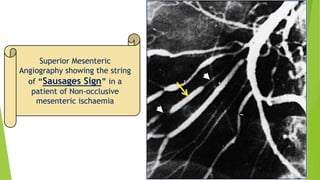
Acute mesenteric ischemia is a life-threatening condition caused by interrupted blood flow to the intestines. It has a high mortality rate of 60-80% if not treated promptly. The document discusses the definition, causes, clinical presentation, diagnostic tests and management of acute mesenteric ischemia. Key diagnostic tests include bloodwork, abdominal imaging like CT angiography and angiography. Treatment involves fluid resuscitation, antibiotics, stopping vasoconstrictors, and often emergency surgery to revascularize the intestines or resect non-viable bowel segments. Prompt diagnosis and treatment are critical given the rapid progression of intestinal tissue damage from ischemia.