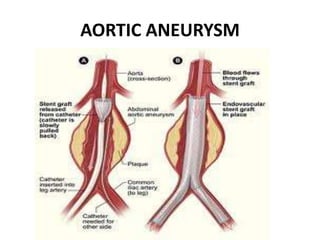
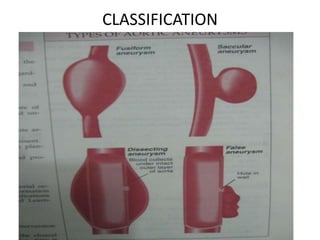
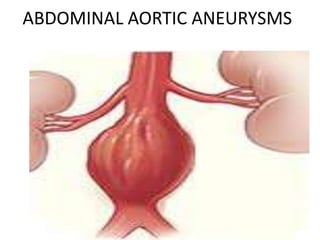
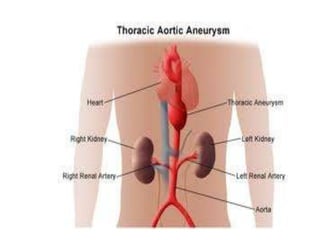
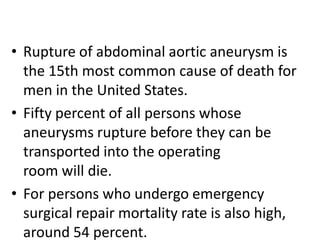
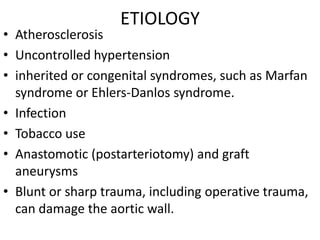
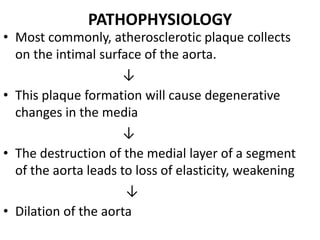
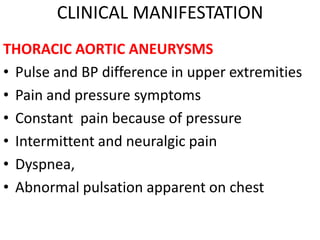
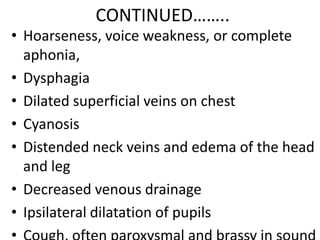
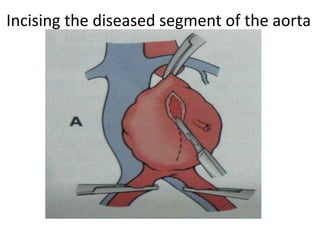
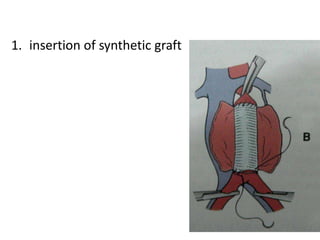
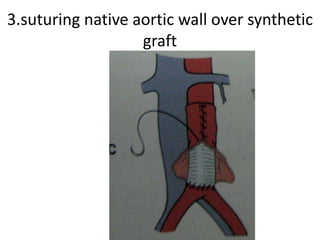
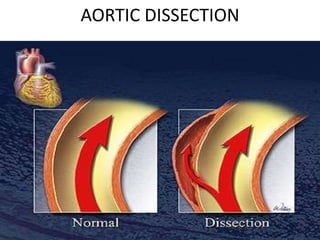
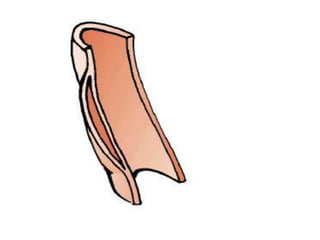
An aortic aneurysm is a dilation of the aorta wall at a weak point. The most common type is abdominal aortic aneurysm, which affects older males. Risk factors include atherosclerosis and smoking. Small aneurysms are monitored while larger aneurysms require surgery to replace the damaged segment. Aortic dissection occurs when blood tears the inner aortic layers, creating a false passageway. It is a medical emergency often presenting with severe chest pain and requires treatment to reduce blood pressure and prevent rupture. Both conditions carry risk of fatal hemorrhage and require lifelong monitoring.