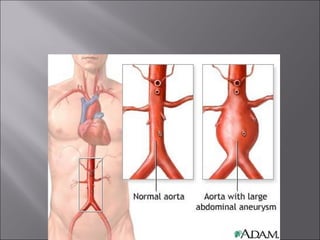
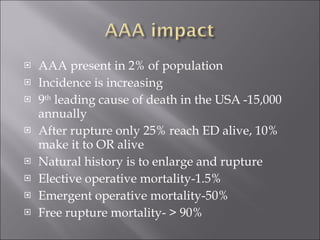
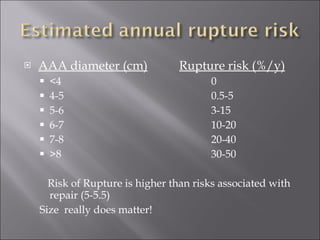
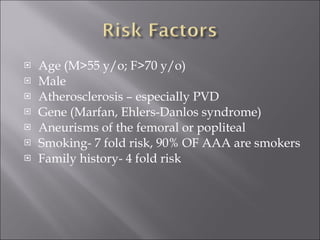
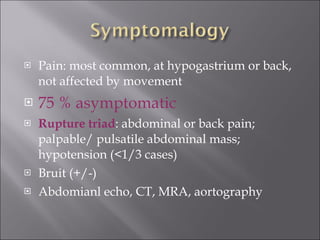
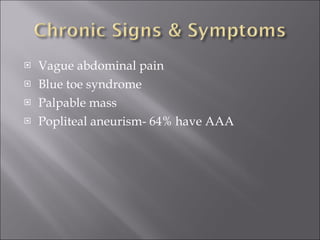
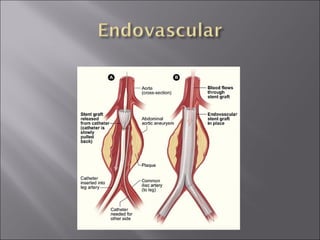
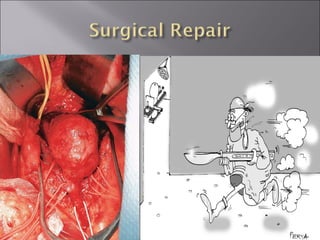
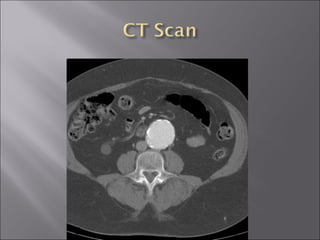
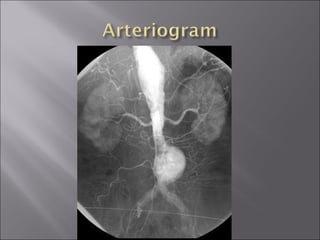
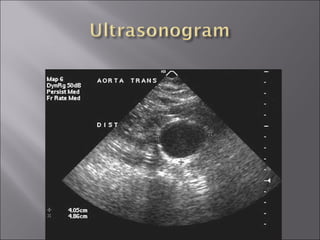
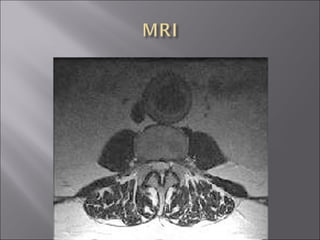
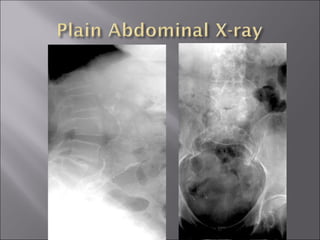
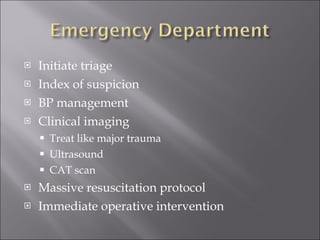
An abdominal aortic aneurysm (AAA) is a pathological dilatation of the normal aortic lumen that can be either fusiform or saccular in shape. AAAs affect about 2% of the population and rupture risk increases with diameter. Elective repair has a mortality of 1.5% while emergency repair has a 50% mortality rate. Screening is recommended for men aged 65-75 who smoke and men and women over 50 with a family history. Surgical repair or endovascular repair depends on aneurysm anatomy, with endovascular repair allowing for shorter hospital stays and recovery times. Prompt recognition and treatment of a ruptured AAA is critical to reduce high mortality rates from rupture.