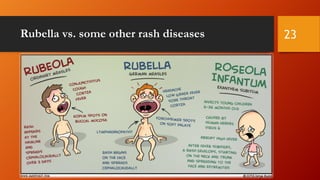
- Rubella, also known as German measles, is a viral infection that can cause birth defects if a pregnant woman is infected.
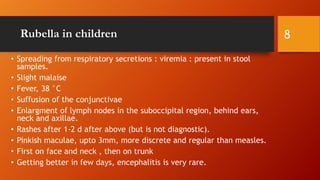
- It is caused by the rubella virus and spreads through respiratory droplets. While it usually causes a mild illness in children, it poses risks during pregnancy.
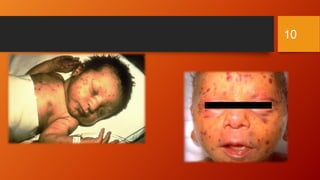
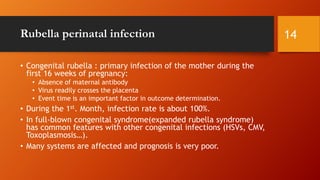
- If a pregnant woman is infected during the first trimester, the virus can cross the placenta and infect the fetus, possibly resulting in congenital rubella syndrome which can affect multiple organs and body systems in the baby.