RSV is a common virus that usually causes mild upper respiratory tract infections but can sometimes lead to pneumonia or bronchiolitis in young children. It is transmitted through respiratory secretions and contaminated surfaces. While infection leads to immunity against that RSV subtype, reinfection is still possible. Diagnosis involves antigen detection, viral culture, or PCR from respiratory samples. Treatment is supportive, though ribavirin may help severe cases. Development of an effective vaccine remains an ongoing effort.

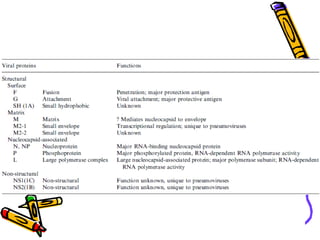
![• RNA genome is 15-16 kb long
• Genome encodes 11 proteins
• Nine are structural (L, G, F, N, P, M,
M2-1, M2-2 and SH)
• Two are non-structural (NS1 and
NS2)
[RSV is divided into two antigenic
subgroups (A and B) on the basis of G
surface glycoprotein]](https://image.slidesharecdn.com/rsv-170310013213/85/Respiratory-Syncytial-Virus-RSV-6-320.jpg)