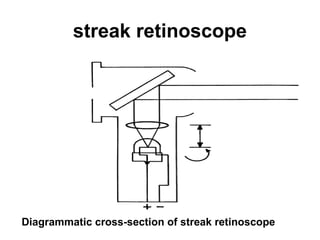
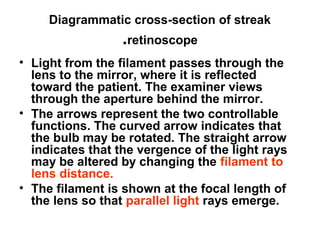
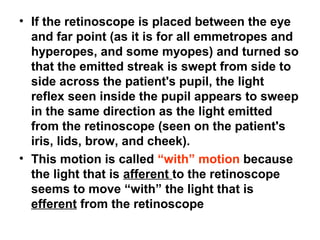
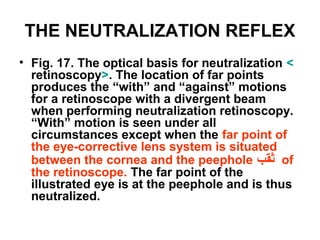
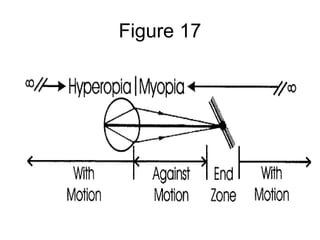
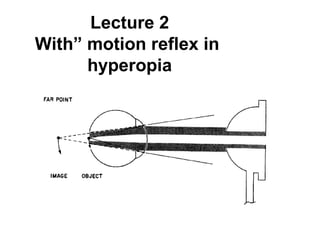
This document discusses the history and optics of the retinoscope, an instrument used in eye examinations to objectively determine a patient's refractive error. It describes how early models used spots or streaks of light and how modern streak retinoscopes work. The retinoscopist can control the orientation and vergence of the emitted light streak and uses this to evaluate the patient's refractive state based on the appearance of the light reflected from their retina. Neutralization retinoscopy involves keeping the retinoscope at a fixed distance while changing the light vergence to determine the refractive error that produces a neutralized reflex from the patient's eye.
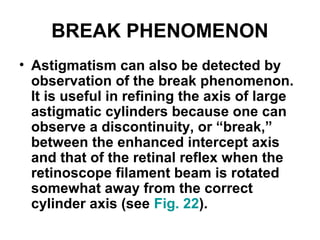

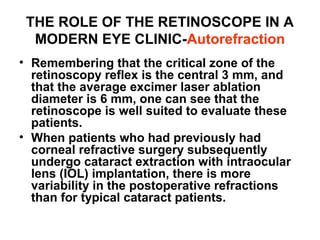
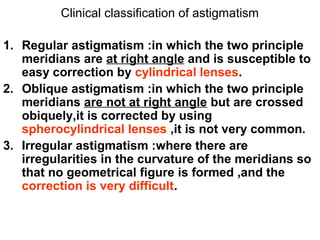
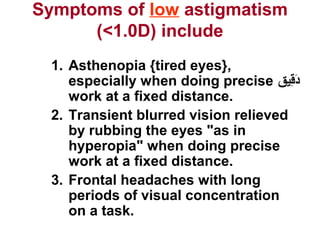
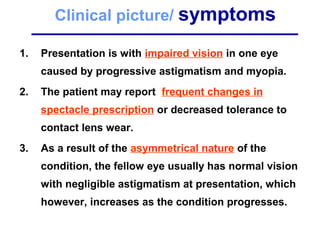
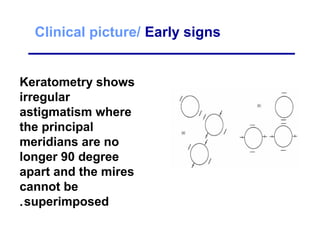
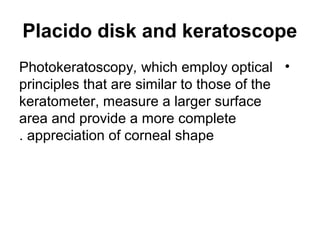
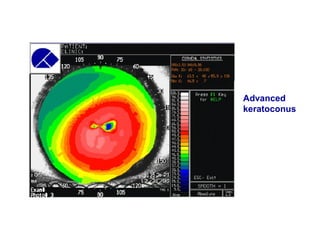
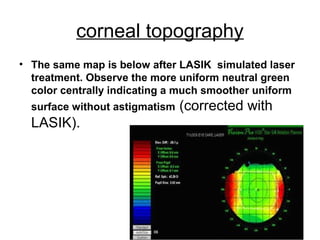
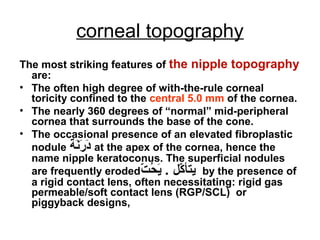
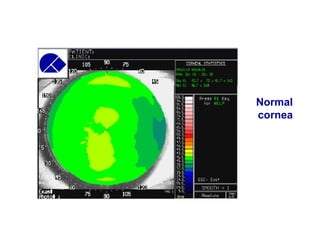
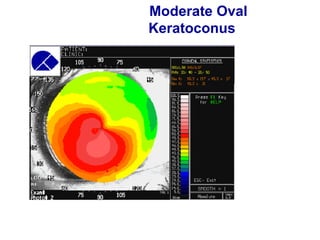
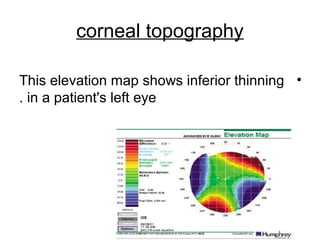
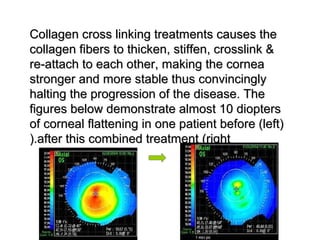
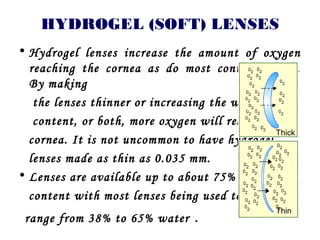
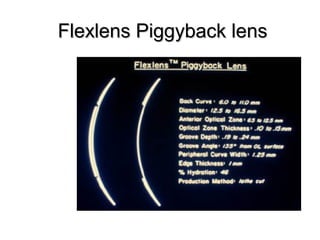
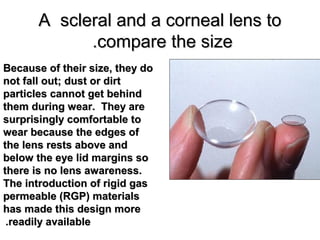
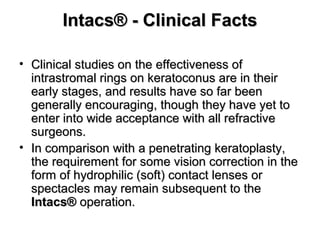
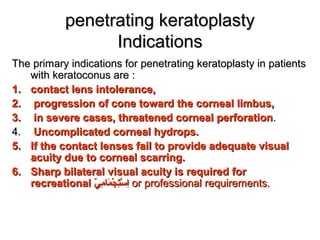
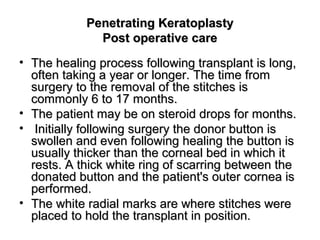
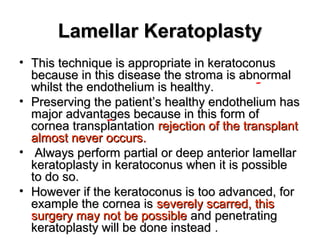
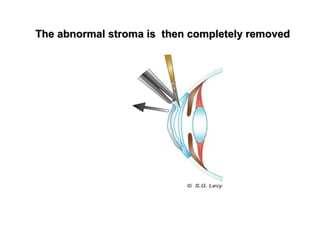
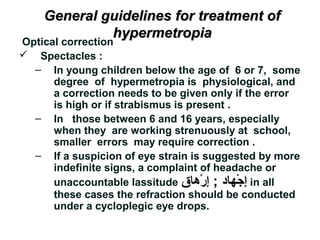
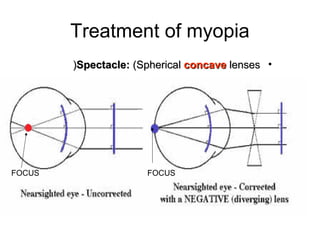
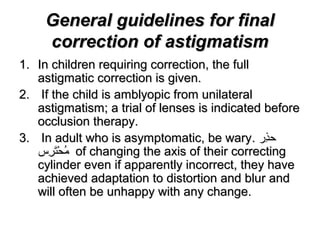
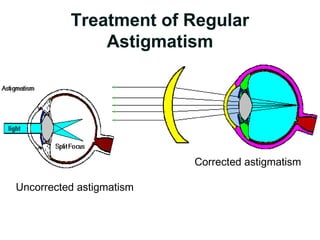
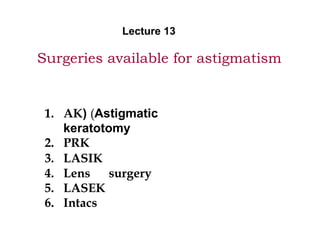
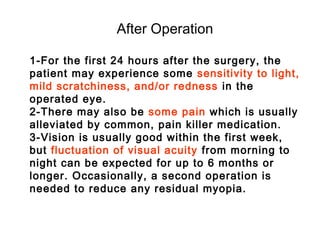
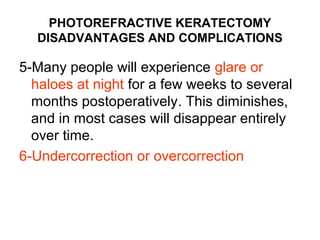
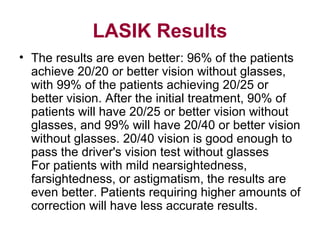
![Spherical Lens Technique
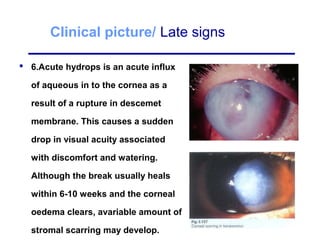
• A simple conversion then needs to be performed before
presenting the patient with the proper spectacle
prescription, as follows:
• Q: A patient is neutralized with the following lenses at a
working distance of 66 cm: [+ 3.50 axis 90] and
[+ 4.25 axis 180]. What is the eyeglasses prescription?
A: Step 1: Subtract the working distance. In this case,
the working distance is 66 cm, which is equal to 1.50 D:
[+ 3.50 axis 90] - 1.50 = + 2.00 axis 90
[+ 4.25 axis 180] - 1.50 = + 2.75 axis 180
Step 2: Transpose from cross-cylinder notation to plus-
cylinder notation:
+ 2.00 sphere + ([+ 2.75 - 2.00] axis 180)
Objective prescription = +2.0 DS+ 0.75 DC x 180](https://image.slidesharecdn.com/retinoscopy-1231056925696931-1/85/Retinoscopy-113-320.jpg)
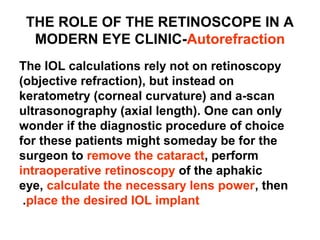
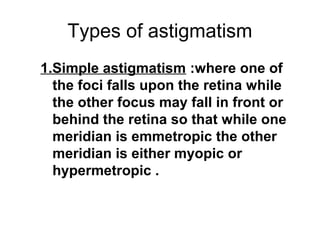
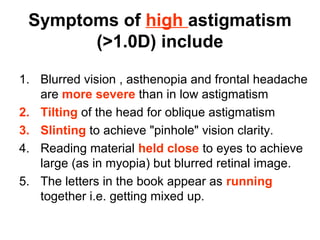
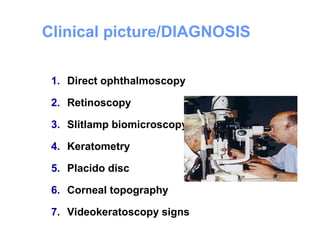
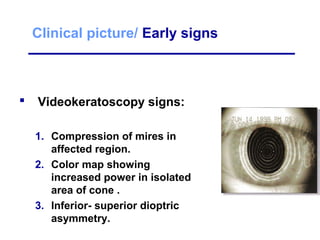
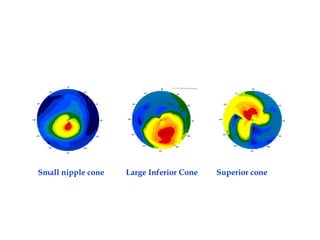
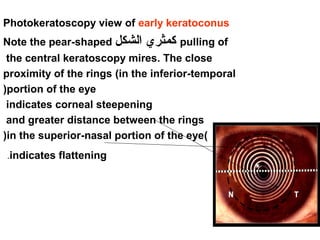
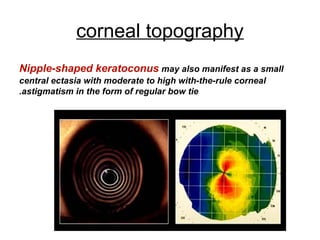
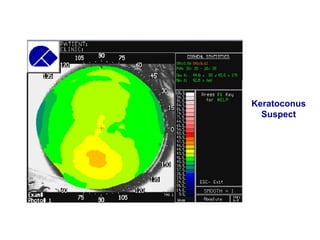
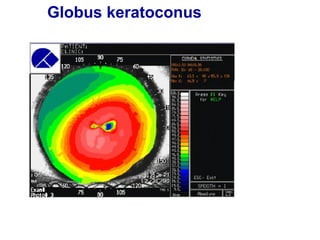
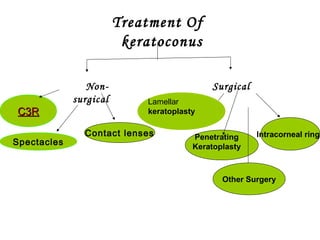
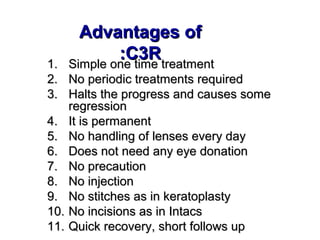
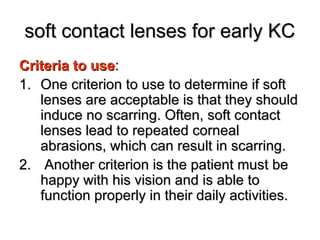
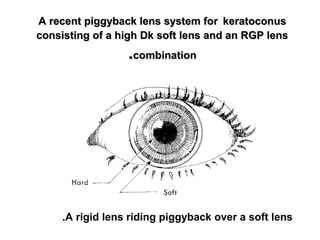
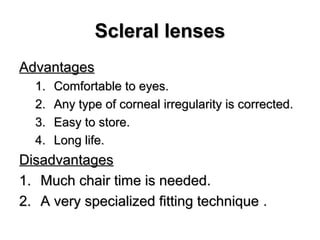
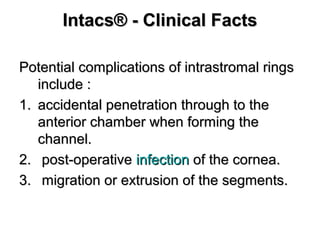
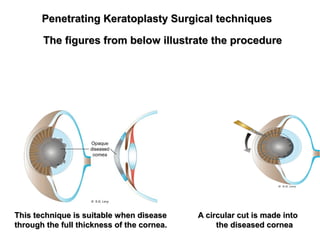
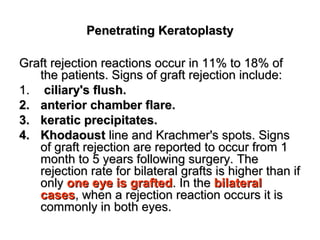
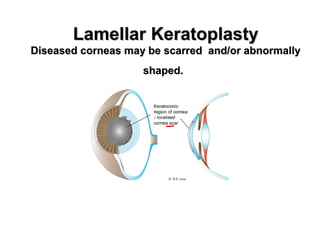
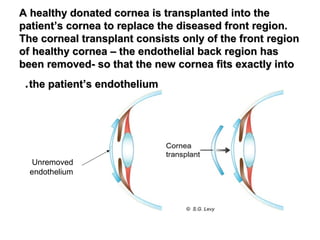
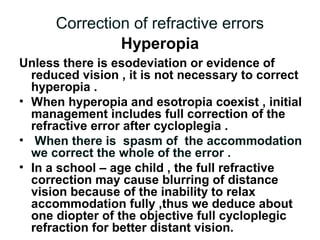
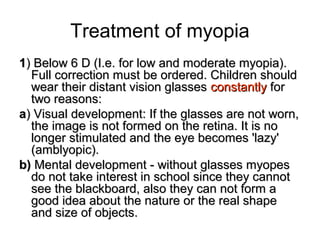
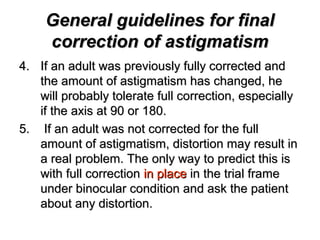
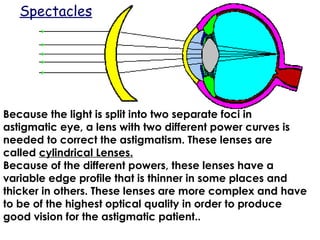
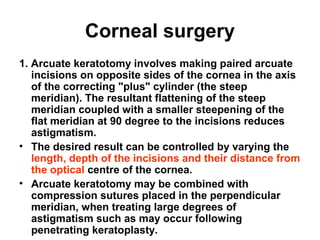
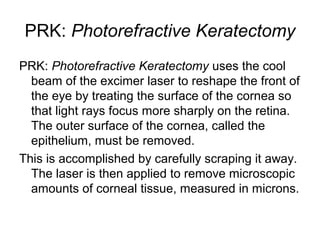
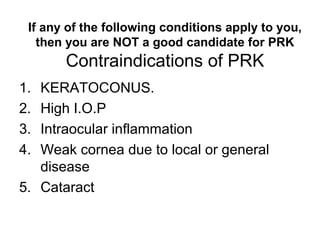
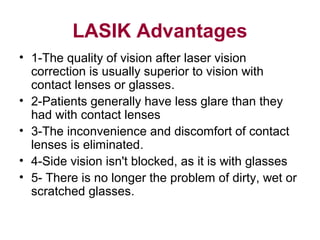
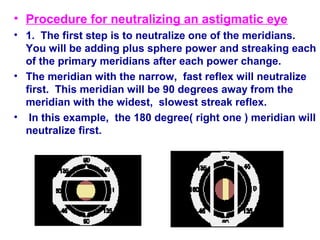
![Plus-Cylinder Technique
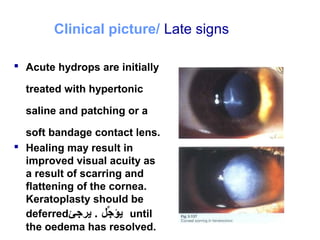
• The working distance is then subtracted from the
spherical lens only, and the spectacle prescription is
easily determined as follows:
• Q: A patient is neutralized with the following lenses
at a working distance of 66 cm: [+ 3.50 sphere] and
[+ 0.75 axis 180]. What is the eyeglasses prescription?
• A: Step 1: Subtract the working distance from the
spherical lens only. In this case, the working distance
is 66 cm, which is equal to 1.50 D:
[+ 3.50 sphere] - 1.50 = + 2.00 sphere
Step 2: Add the cylindrical lens to the new power of
the spherical lens:
+ 2.00 sphere + [+ 0.75 axis 180]
Objective prescription= 2.00 + DS + 0.75 DC x180](https://image.slidesharecdn.com/retinoscopy-1231056925696931-1/85/Retinoscopy-116-320.jpg)
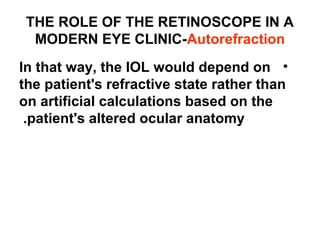
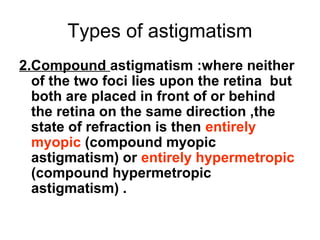
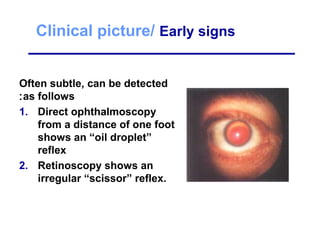
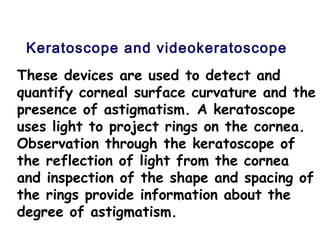
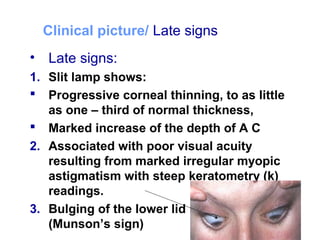
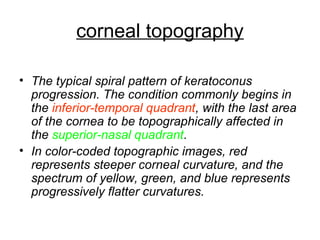
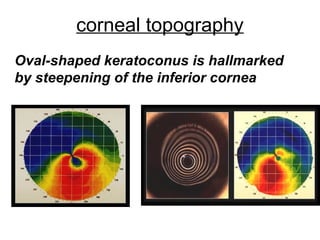
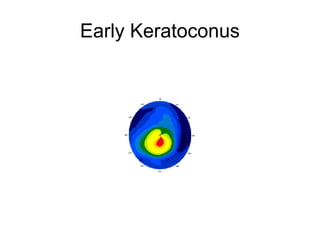
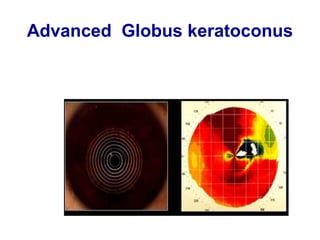
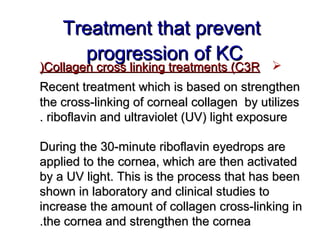
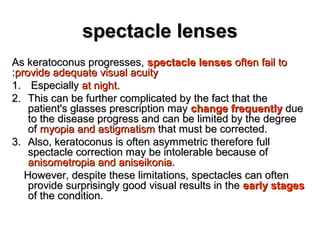
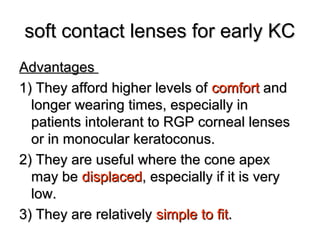
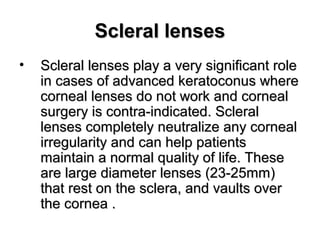
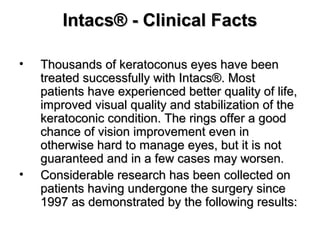
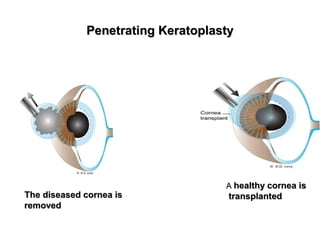
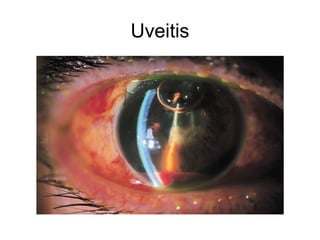
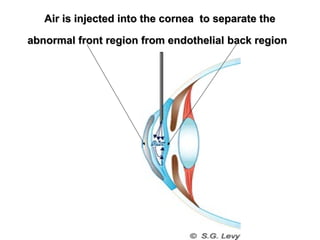
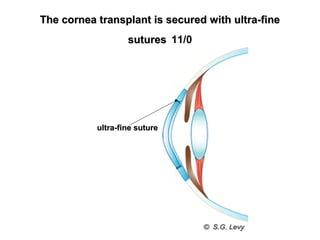
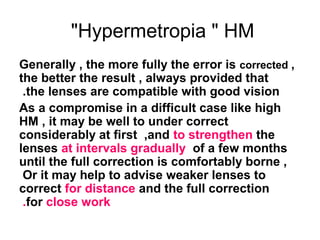
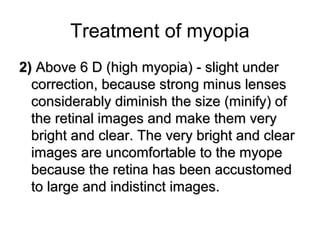
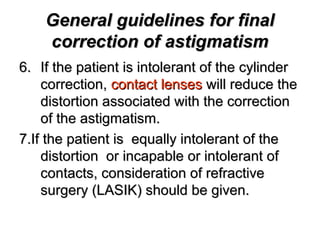
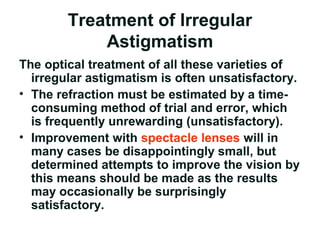
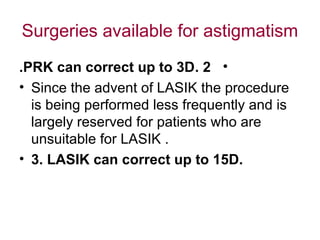
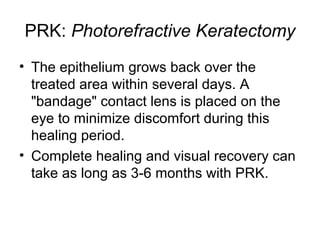
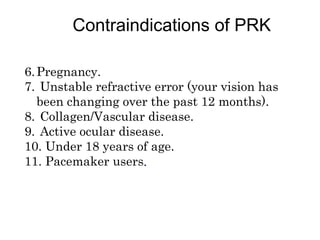
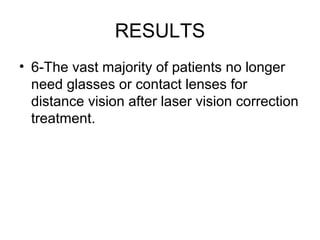
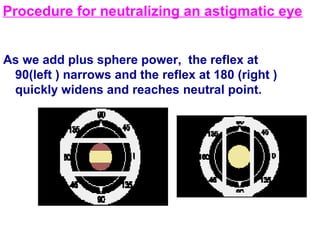
![Minus-Cylinder Technique
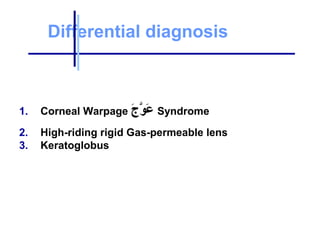
• Q: A patient is neutralized with the following
lenses at a working distance of 66 cm: [+ 4.25
sphere] and [-0.75 axis 90]. What is the
eyeglasses prescription?
A: Step 1: Subtract the working distance from
the spherical lens only. In this case, the working
distance is 66 cm, which is equal to 1.50 D:
)+ 4.25 -1.50 (= + 2.75 sphere
Step 2: Add the minus cylindrical lens to the
new power of the spherical lens:
• + 2.75 sphere + (-0.75 axis 90(
90 × 0.75 - 2.75 + =](https://image.slidesharecdn.com/retinoscopy-1231056925696931-1/85/Retinoscopy-118-320.jpg)

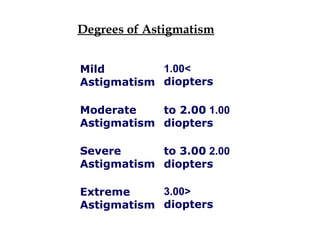
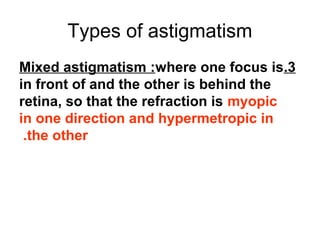
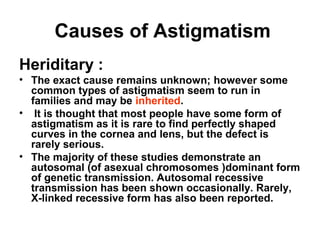
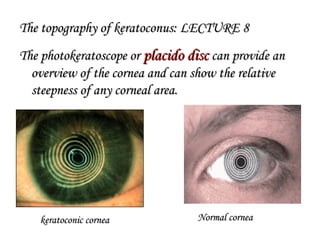
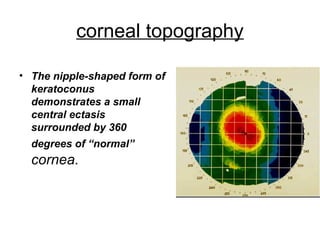
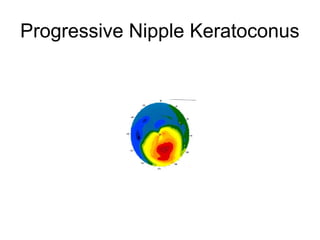
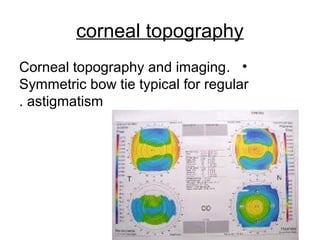
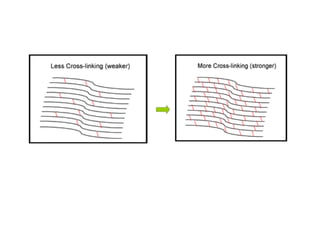
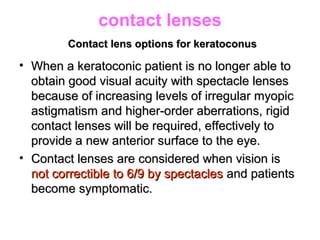
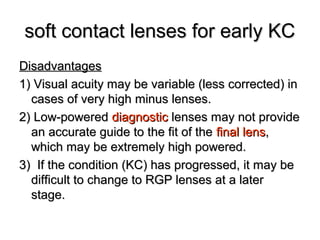
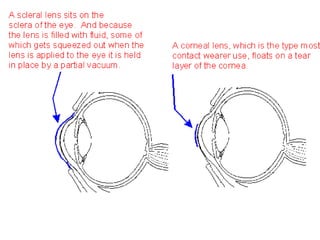
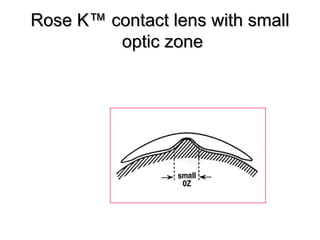
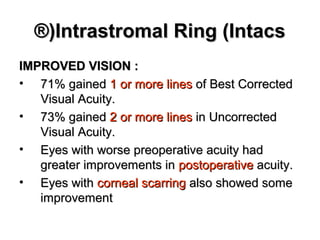
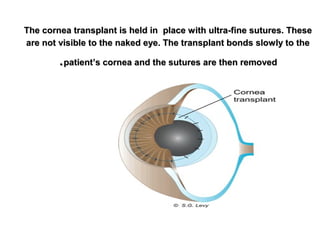
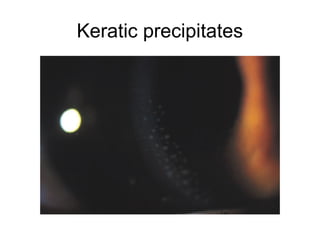
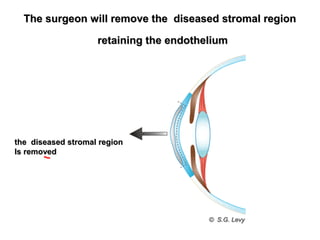
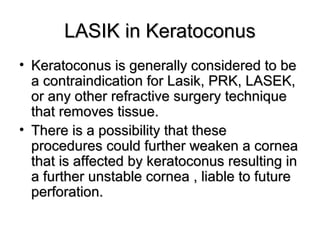
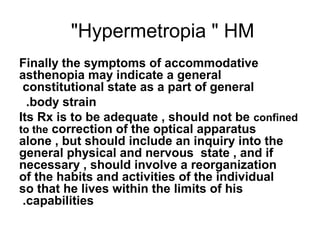
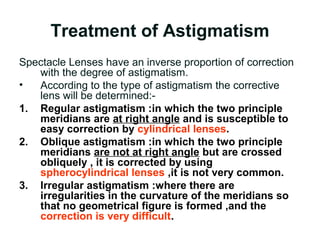
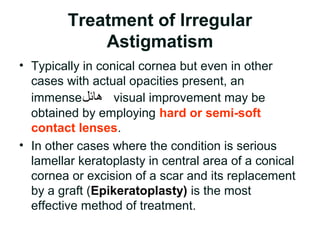
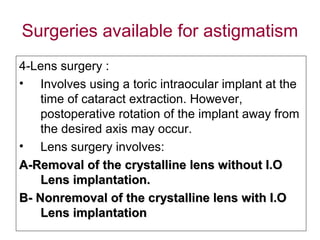
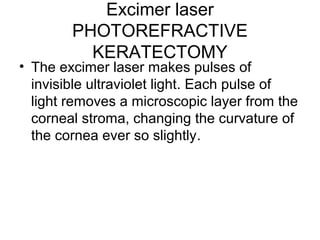
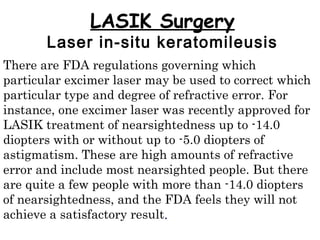
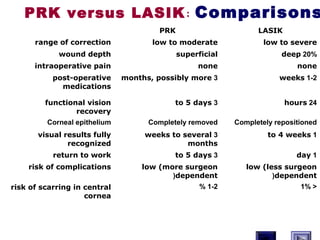
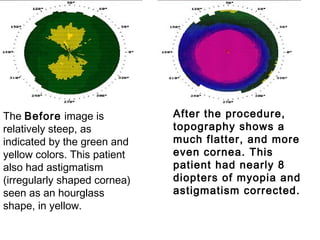
![Autorefraction
• Where the automated refractor is at an undeniable ال
حدَ a جَْر يُض ال . كرَ a نَْريُض disadvantage to the retinoscope is in
evaluating patients with irregular astigmatism, either
from pathology (e.g., keratoconus, pellucid marginal
degeneration) or postsurgically (e.g., corneal
transplant, laser in situ keratomileusis [LASIK]). All
the automated refractor operator can do is press a
button while having the patient fixate on the target.
• The automated refractor then either calculates a
“best fit” refraction or flashes an error message that
there too much irregular astigmatism exists to make
a reading.( Over cylinder)](https://image.slidesharecdn.com/retinoscopy-1231056925696931-1/85/Retinoscopy-133-320.jpg)