This document discusses ischaemia of the lower limbs, including definitions, causes, clinical features, investigations and management. Some key points:
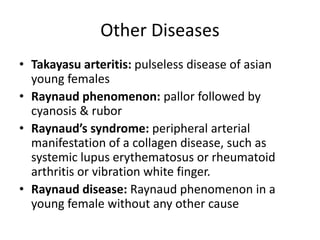
- Peripheral vascular disease refers to obstruction or deterioration of arteries other than those supplying the heart or brain.
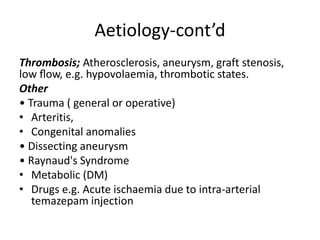
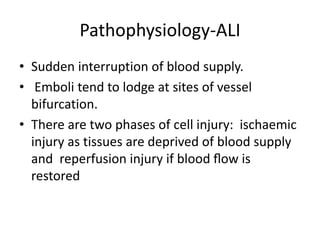
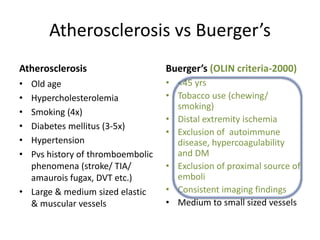
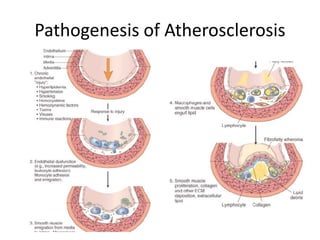
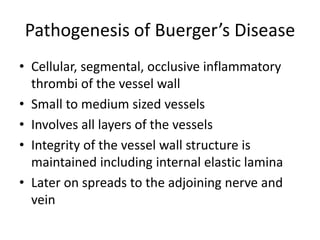
- Causes of acute limb ischaemia include embolism (often from the heart) and thrombosis (due to atherosclerosis, aneurysm, etc.).
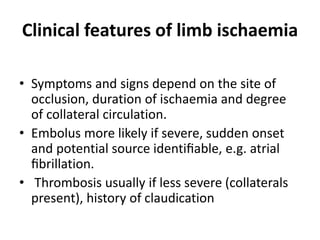
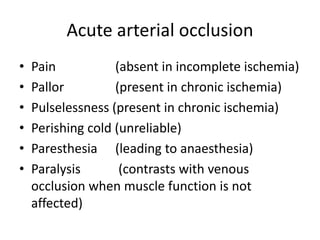
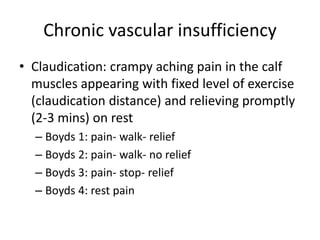
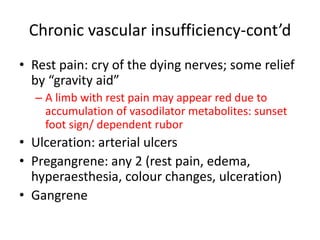
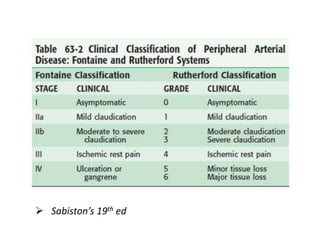
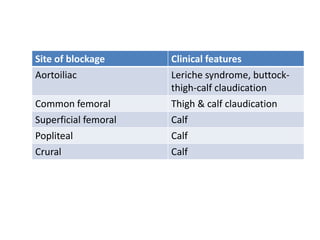
- Clinical features depend on location and duration of ischaemia, and can include pain, pallor, pulselessness, paralysis. Beyond 6 hours ischemia is usually irreversible.
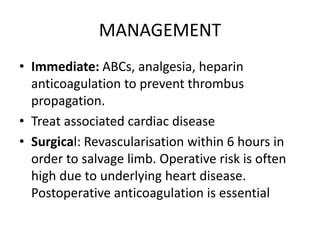
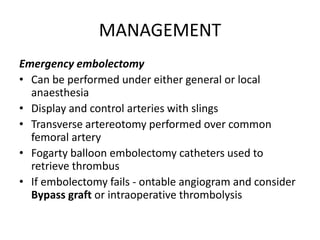
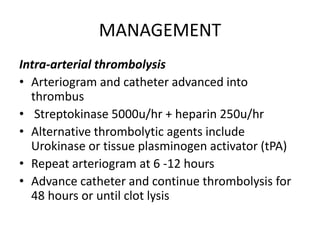
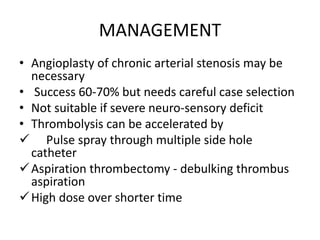
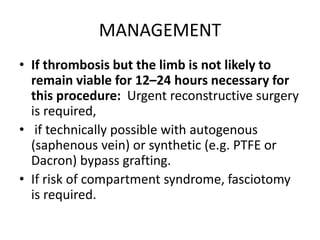
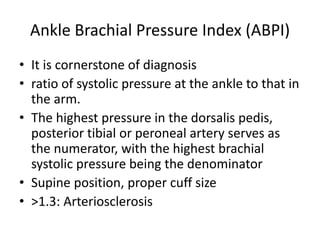
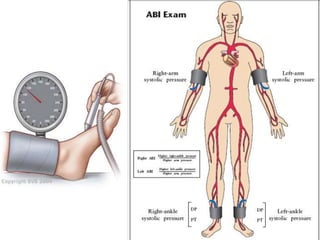
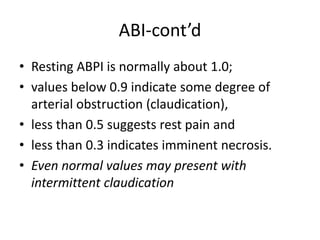
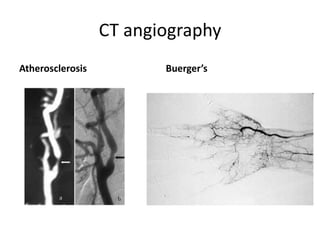
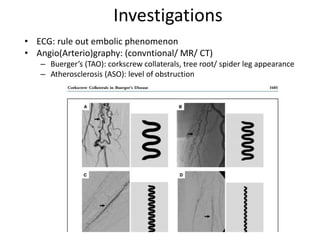
- Investigations include blood tests, imaging like Doppler ultrasound and angiography. Management involves treating the cause, and surgical