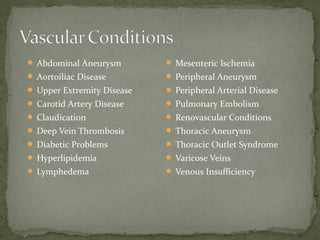
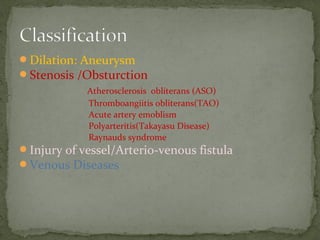
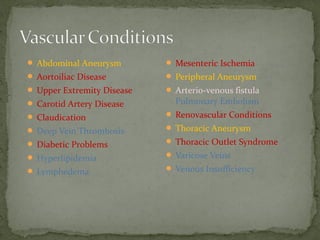
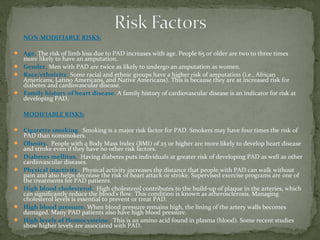
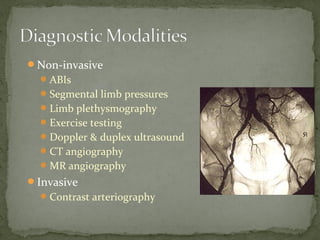
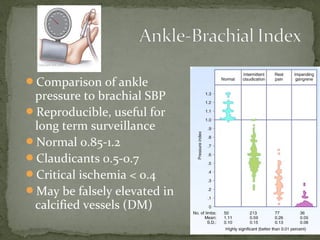
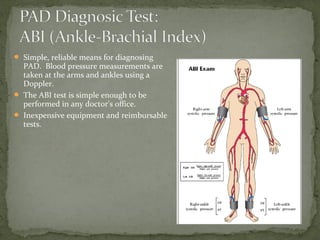
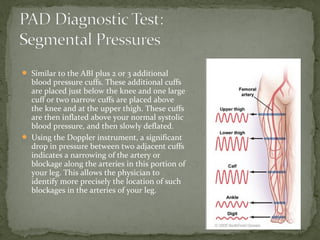
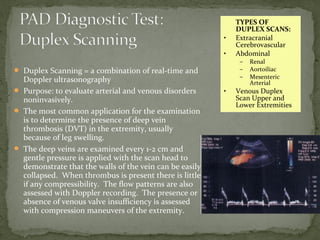
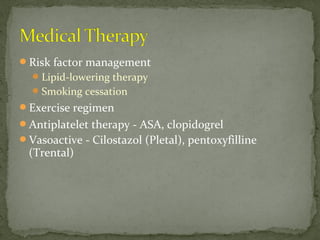
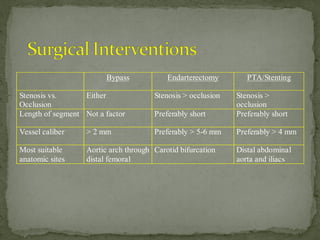
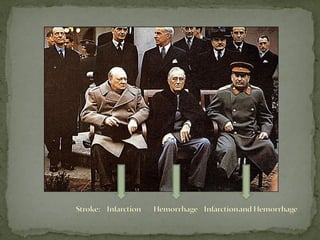
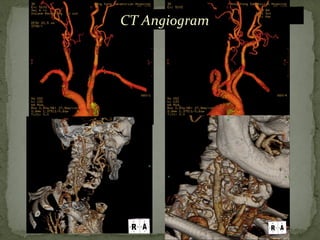
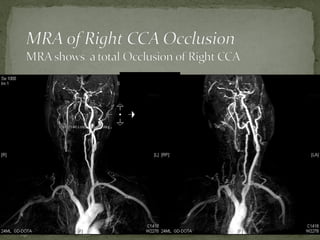
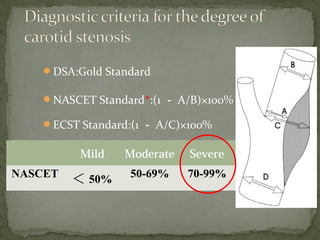
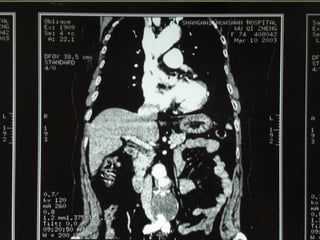
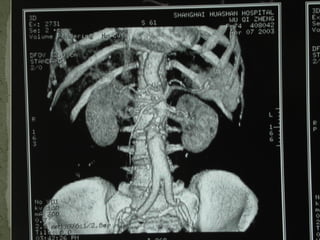
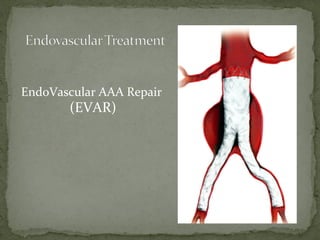
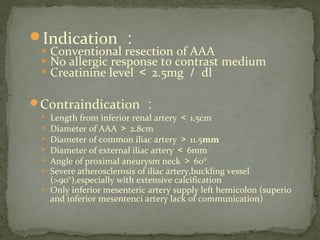
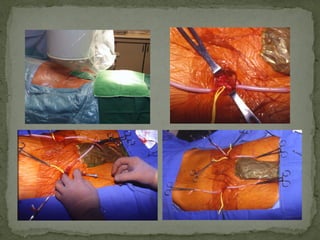
Peripheral vascular disease refers to narrowing of blood vessels outside the heart and brain, often affecting legs. It has many causes including atherosclerosis, aneurysms, arterial injuries or clots. Diagnosis involves tests like ankle-brachial indexes, duplex ultrasound, CT or MR angiography. Treatment depends on symptoms and location but may include risk factor modification, medications, angioplasty, stenting or surgery.