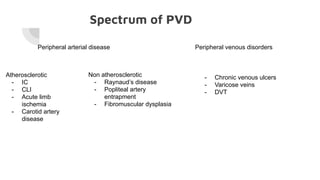
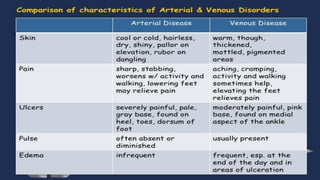
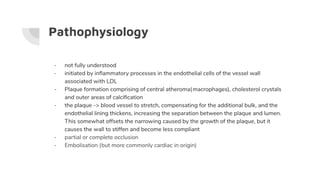
- Peripheral vascular disease (PVD) refers to disorders affecting arteries, veins and lymphatics outside the heart and brain. More commonly it affects the arteries.
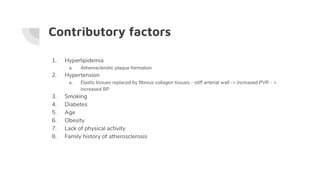
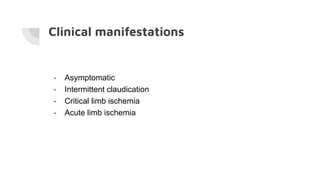
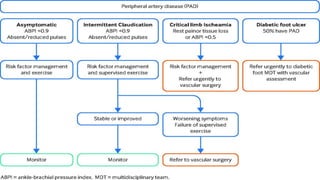
- PVD ranges from asymptomatic to critical limb ischemia with pain, ulcers or gangrene. Risk factors include smoking, diabetes, hypertension, hyperlipidemia, age and family history.
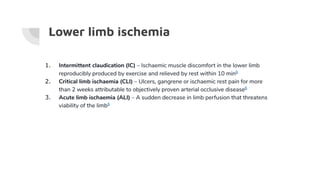
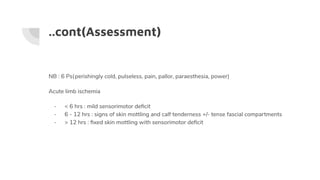
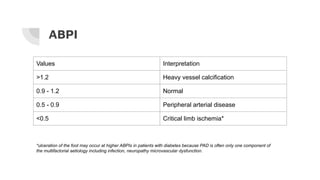
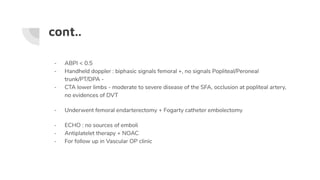
- Clinical features depend on location and severity, from intermittent claudication to critical limb ischemia. Investigations include ankle-brachial pressure index and imaging of arteries.
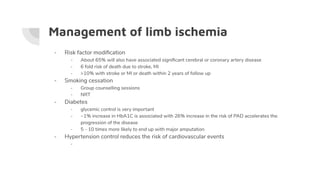
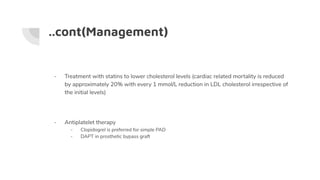
- Management involves risk factor modification, exercise/drugs for claudication, endovascular procedures, surgery like bypass, and amputation for critical cases. Compression therapy