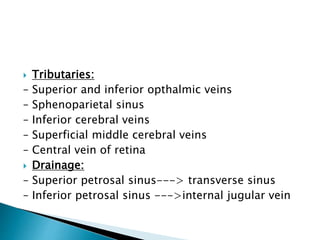
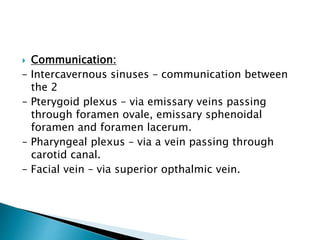
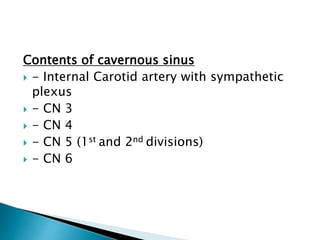
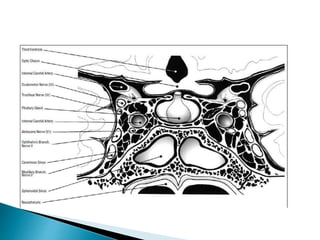
1. The cavernous sinus is located on either side of the body of the sphenoid bone and contains several important structures like cranial nerves and blood vessels.
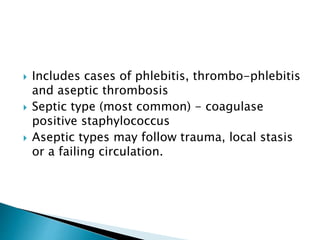
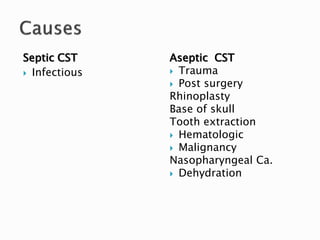
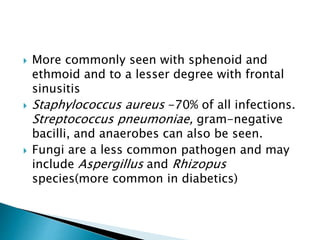
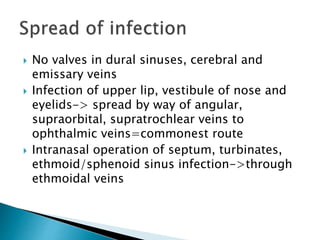
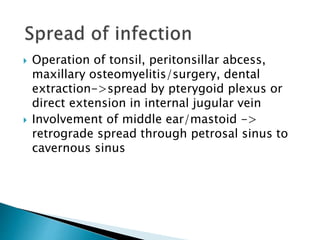
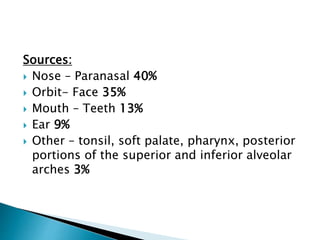
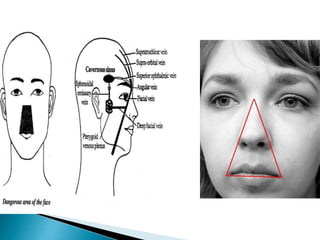
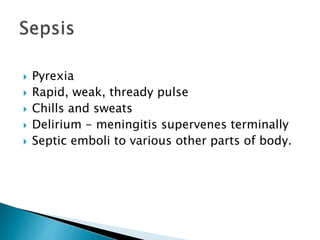
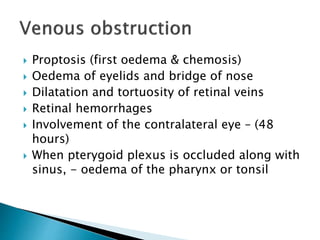
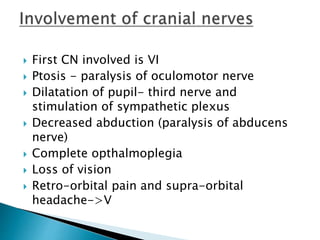
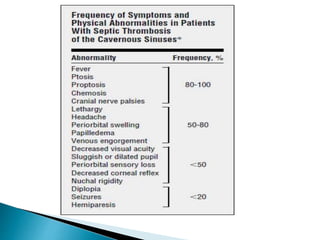
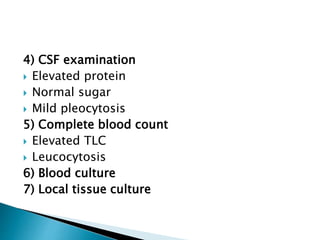
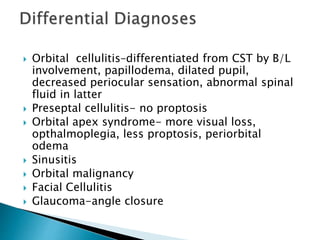
2. Septic cavernous sinus thrombosis is usually caused by infection spreading from nearby sites like the nose, orbit, or teeth. Common symptoms include proptosis, ophthalmoplegia, and fever.
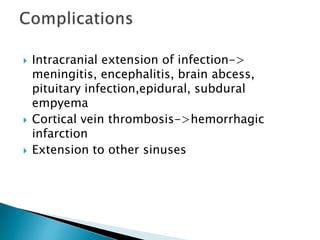
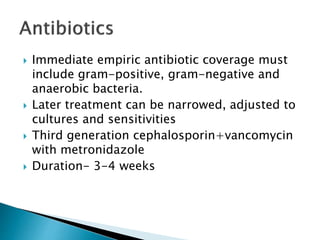
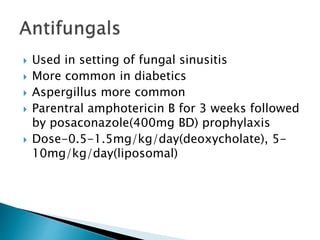
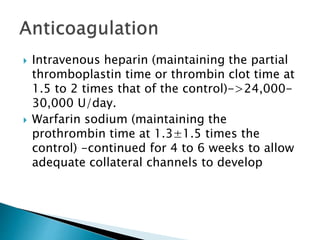
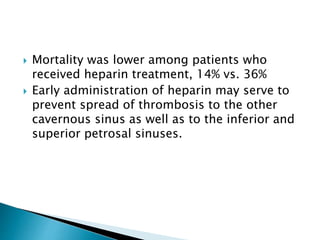
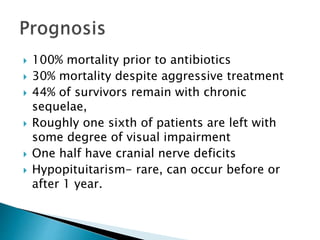
3. Treatment involves intravenous antibiotics, anticoagulation with heparin, and sometimes steroids; early diagnosis and treatment can help reduce mortality and long-term complications, which remain significant risks.