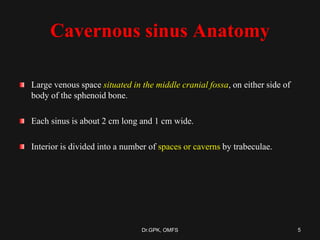
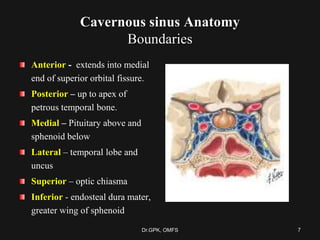
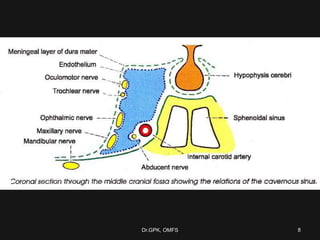
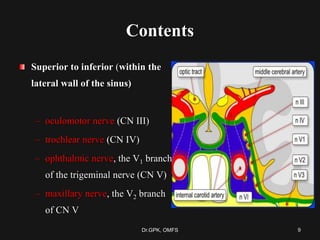
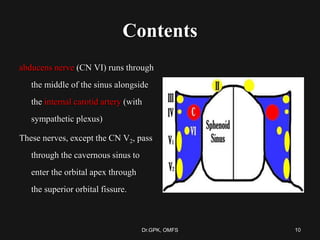
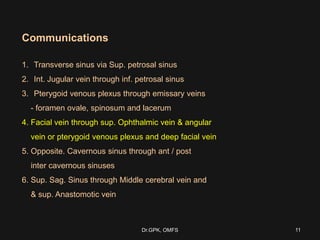
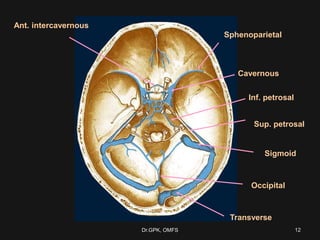
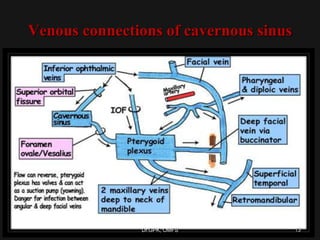
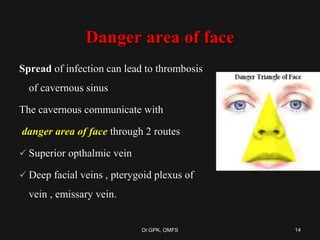
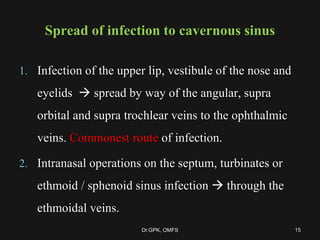
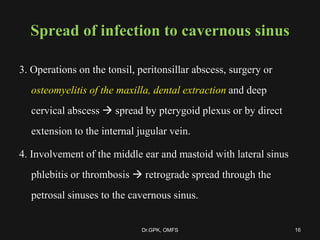
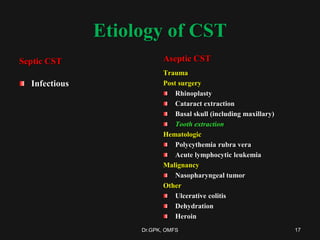
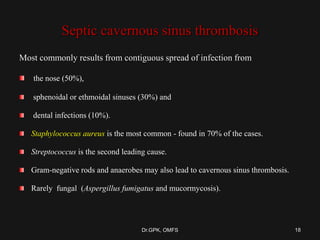
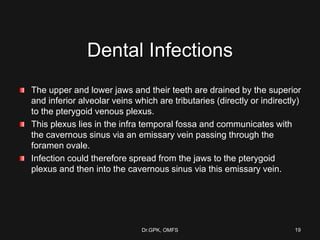
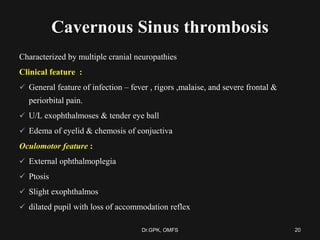
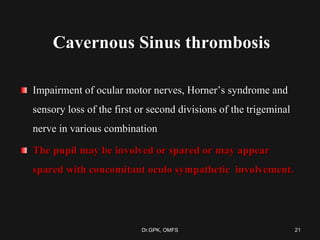
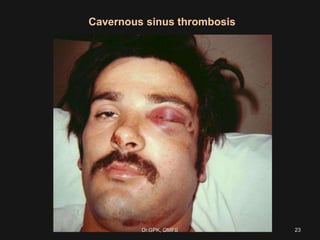
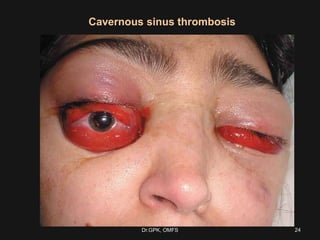
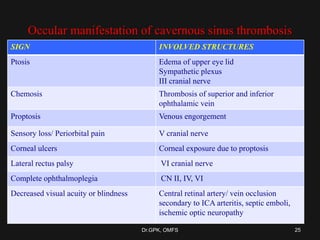
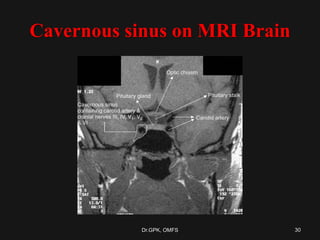
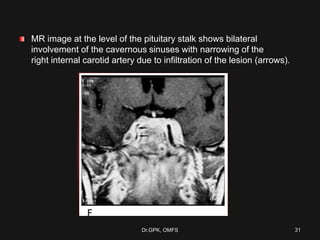
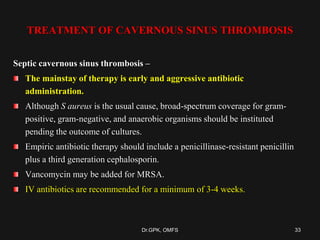
The document discusses cavernous sinus thrombosis, covering its anatomy, etiology, clinical features, and treatment options. It highlights the significance of infection spread from areas such as the face and dental regions leading to thrombosis, along with the importance of timely medical management. Early aggressive antibiotic therapy is crucial for septic cases, while the role of anticoagulation remains uncertain due to potential complications.