Embed presentation
Download to read offline
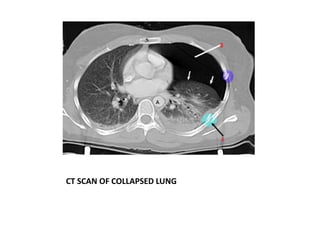
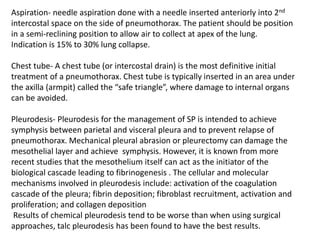
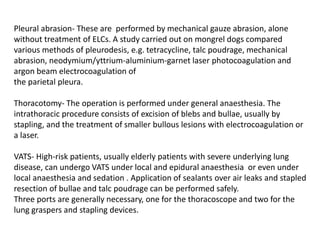
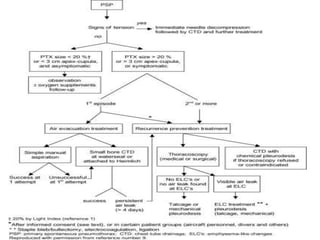
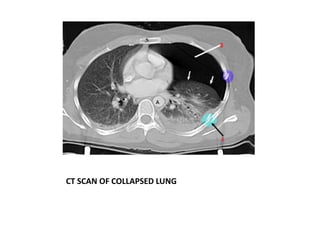
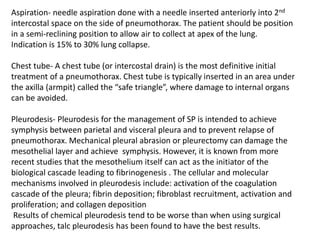
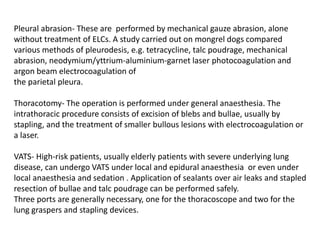
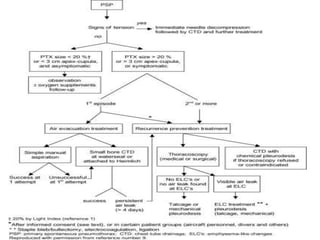
Pneumothorax can be spontaneous, caused by underlying lung conditions (secondary) or trauma/medical procedures (non-spontaneous). It is diagnosed through chest x-ray or ultrasound identifying air in the pleural space. Management includes needle aspiration for small pneumothoraces or chest tube insertion for larger ones. Further treatment may involve procedures like pleurodesis, abrasion, or surgery to prevent recurrence. Physiotherapy focuses on improving ventilation and clearing secretions through techniques like breathing exercises, positioning, and airway clearance.