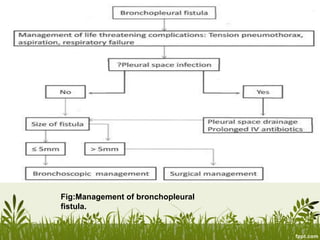
Bronchopleural fistula is an abnormal connection between the bronchial tree and pleural space. It most commonly occurs after pulmonary resection surgery, with reported incidence rates of 1.5-28%. Patients at higher risk include those with lung infections, trauma, or underlying lung disease. BPFs are classified as acute, sub-acute, or chronic depending on time of onset and presentation. Acute BPF presents urgently with breathing difficulties while chronic BPF involves infection and fibrosis. Treatment involves managing life-threatening complications, controlling infections, and closing the fistula through surgery or drainage.


![CONTINUE…
• Varoli et al7 classified fistulas according to
the time of onset after the operation:
1) early [1 to 7 days]
2) intermediate [8 to 30days]
3) late fistulas [more than 30 days].](https://image.slidesharecdn.com/bronchopleuralfis-161210164027/85/Bronchopleuralfistula-9-320.jpg)