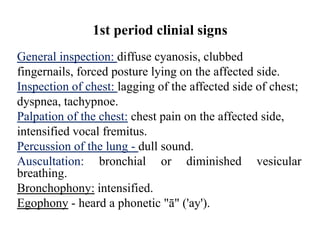
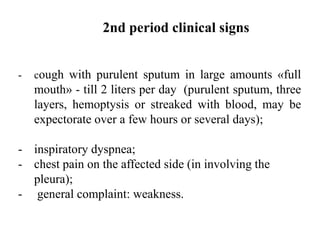
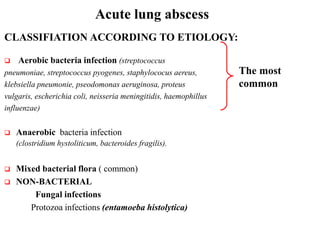
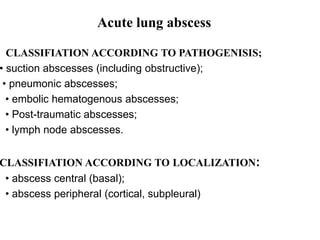
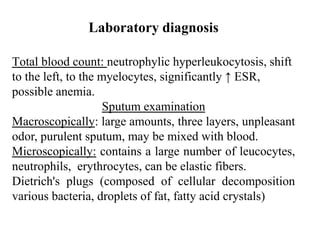
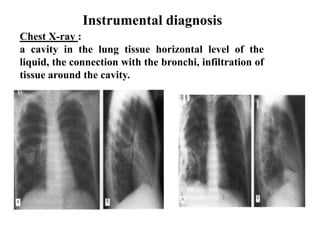
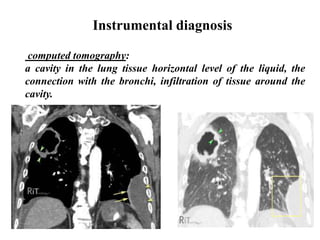
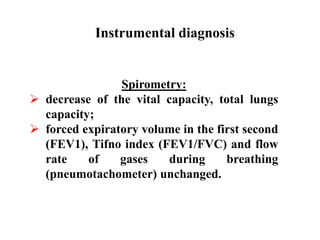
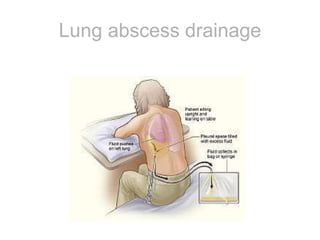
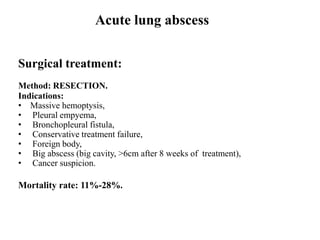
Acute lung abscess is defined as a localized cavity with pus resulting from lung tissue necrosis within a few weeks. Clinical signs include fever, cough, chest pain, and expectoration. Diagnosis involves chest x-ray showing a cavity connected to bronchi, and sputum examination revealing purulent material. Treatment includes antibiotics, drainage, or surgery depending on the size and location of the abscess. Surgical options include wedge resection, lobectomy, or pneumonectomy.