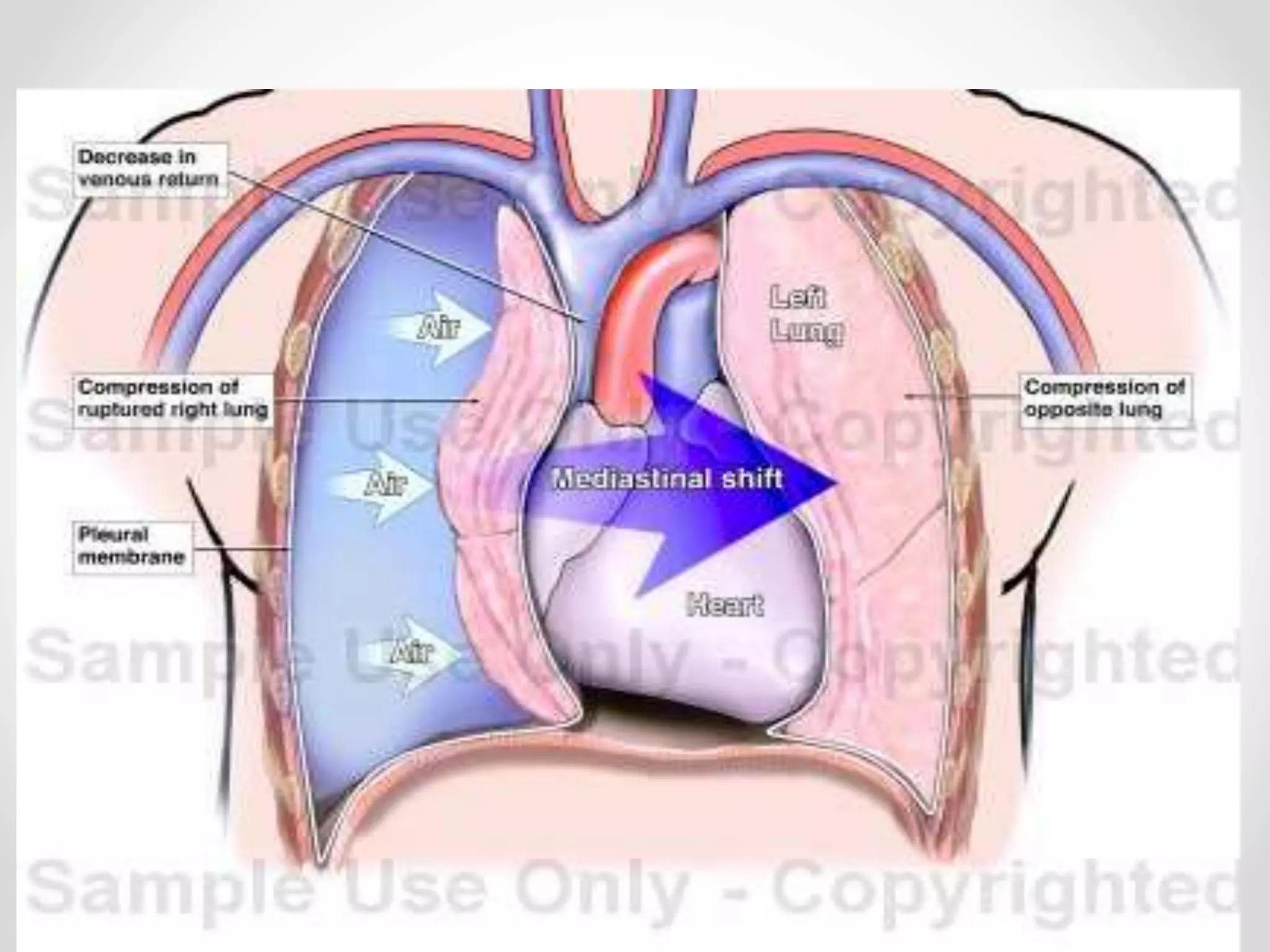
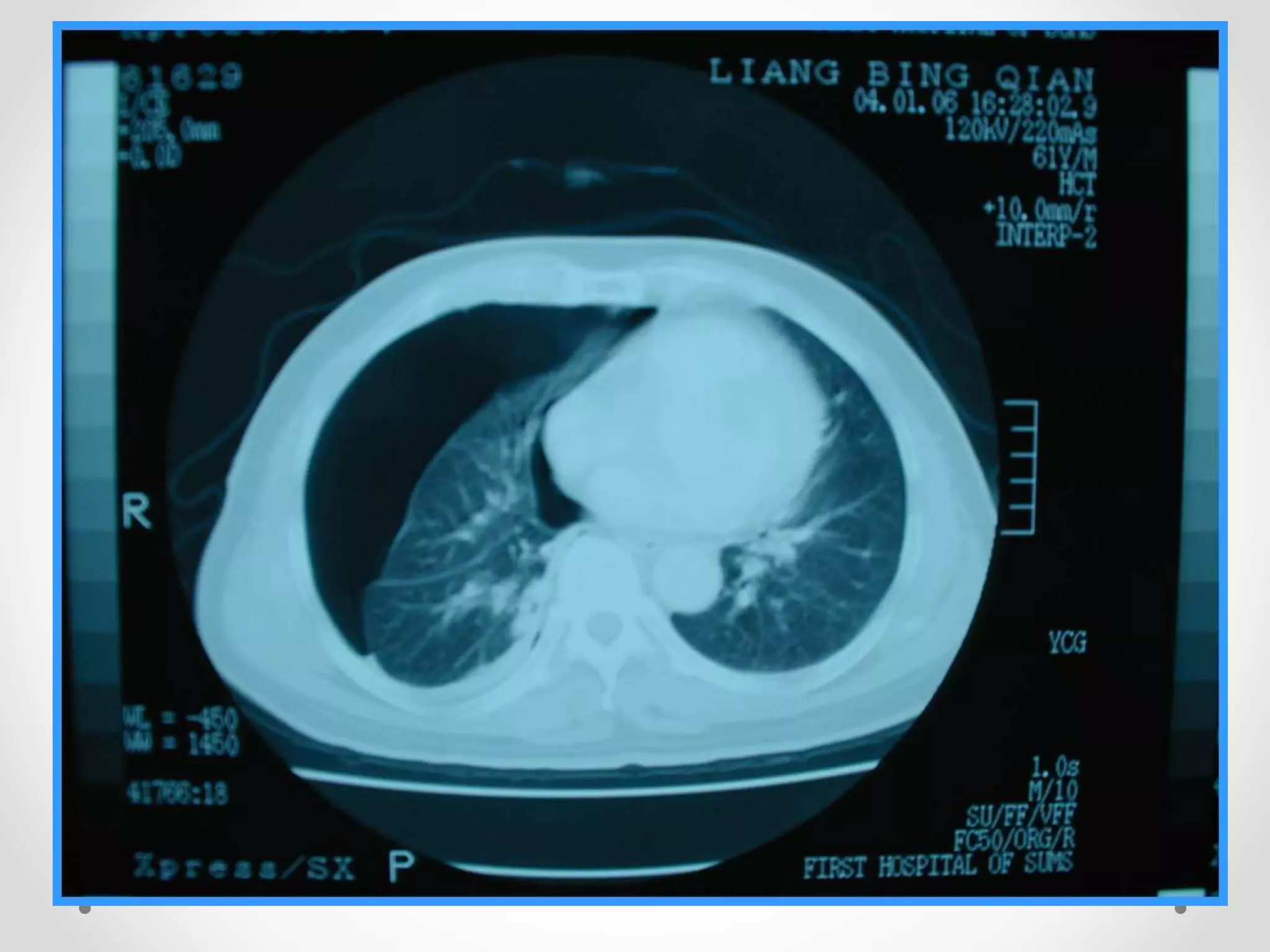
Pneumothorax is defined as air in the pleural space between the lungs and chest wall. It is classified as spontaneous, traumatic, or iatrogenic. A tension pneumothorax occurs when air enters the pleural space during inspiration but cannot escape during expiration, causing rising pressure and potential cardiovascular compromise. Symptoms include chest pain and breathlessness. Diagnosis is made through chest x-ray showing increased radiolucency. Small primary pneumothorax may resolve on its own, while secondary pneumothorax requires tube drainage. Tension pneumothorax is a medical emergency treated with needle decompression followed by tube insertion.






![Clinical features
• Sudden onset of unliateral pleuritic chest pain
• Breathlessness
[In pts with a small pneumothorax, physical examination may
be normal ]](https://image.slidesharecdn.com/pneumothorax-171013103109/75/Pneumothorax-11-2048.jpg)









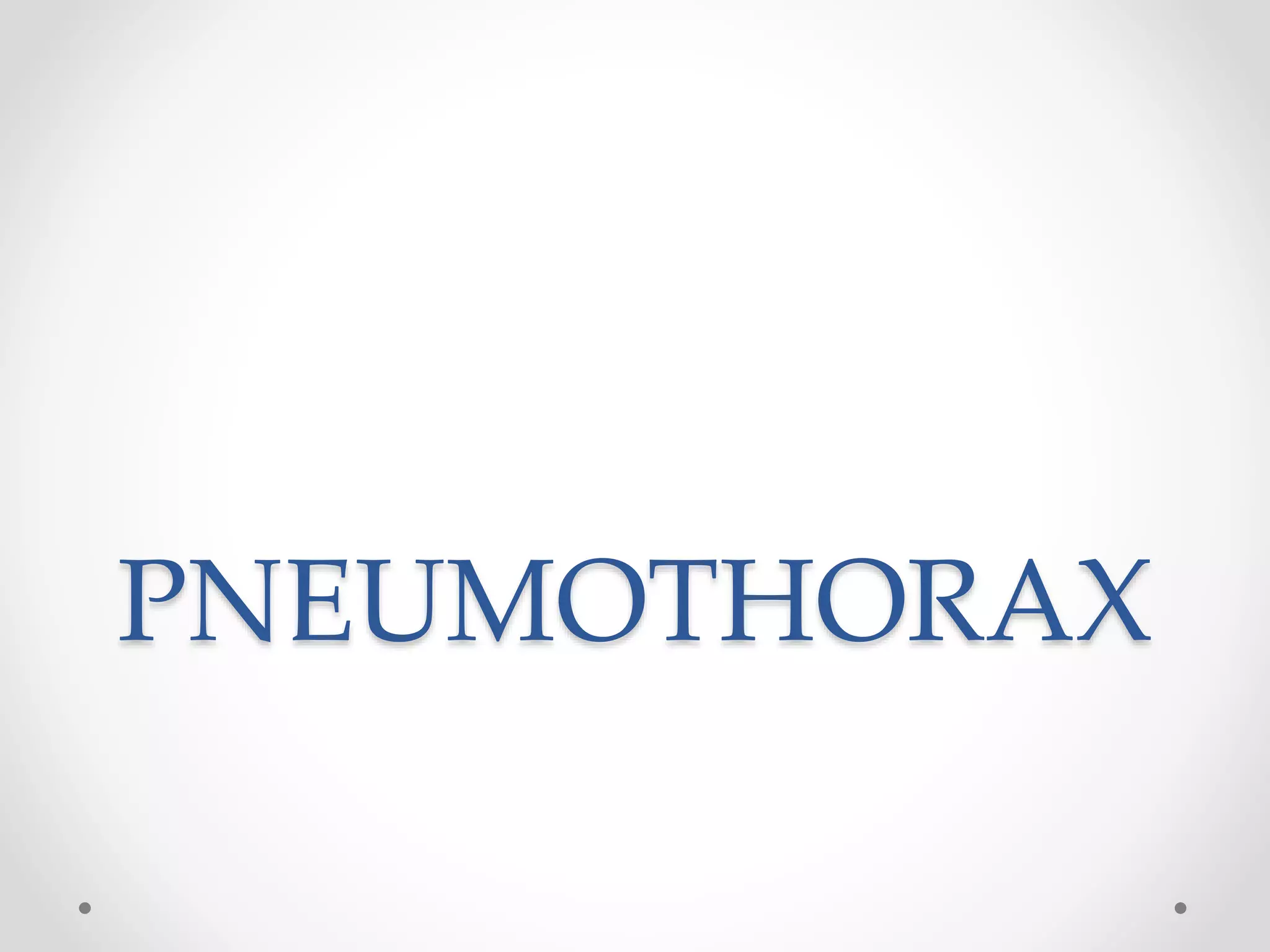
![Secondary pneumothorax
Even a small secondary pneumothorax may
cause respiratory failure, so all such patients require
↓
Intercostal tube drainage
[Intercostal drains are inserted in the 4th ,5th or 6th intercostal
space in the midaxillary line ,connected to an under
waterseal]](https://image.slidesharecdn.com/pneumothorax-171013103109/75/Pneumothorax-24-2048.jpg)