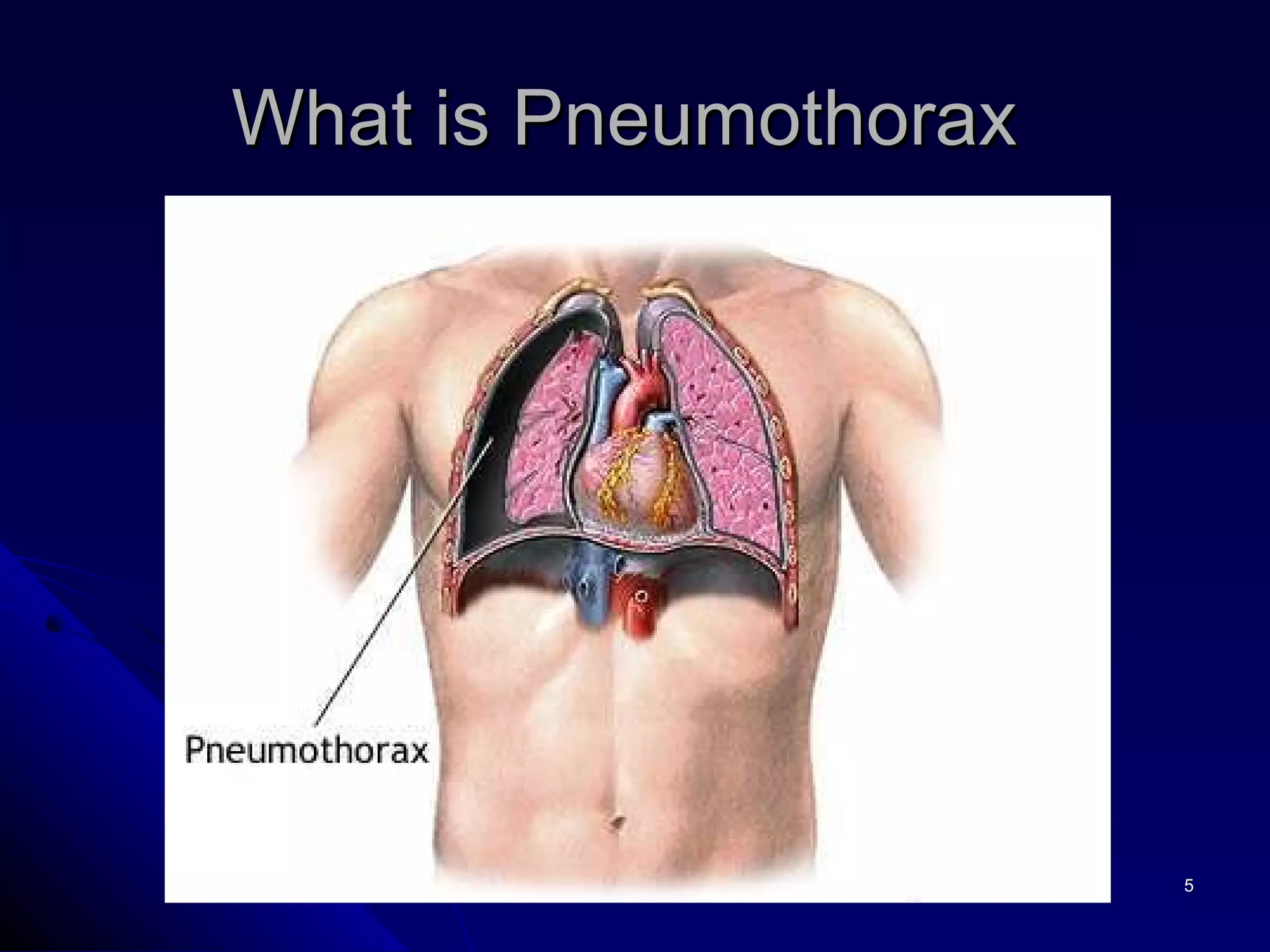
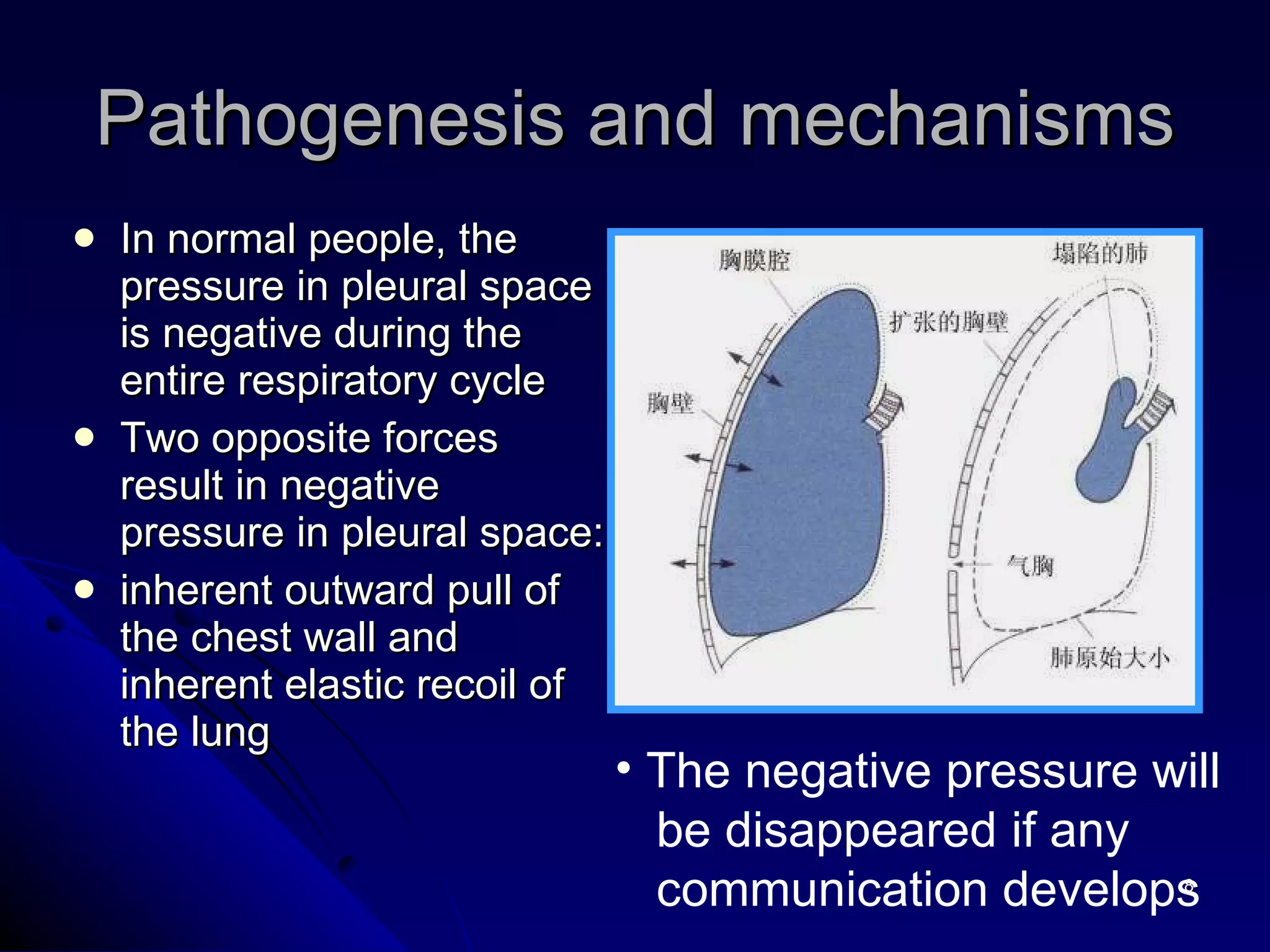
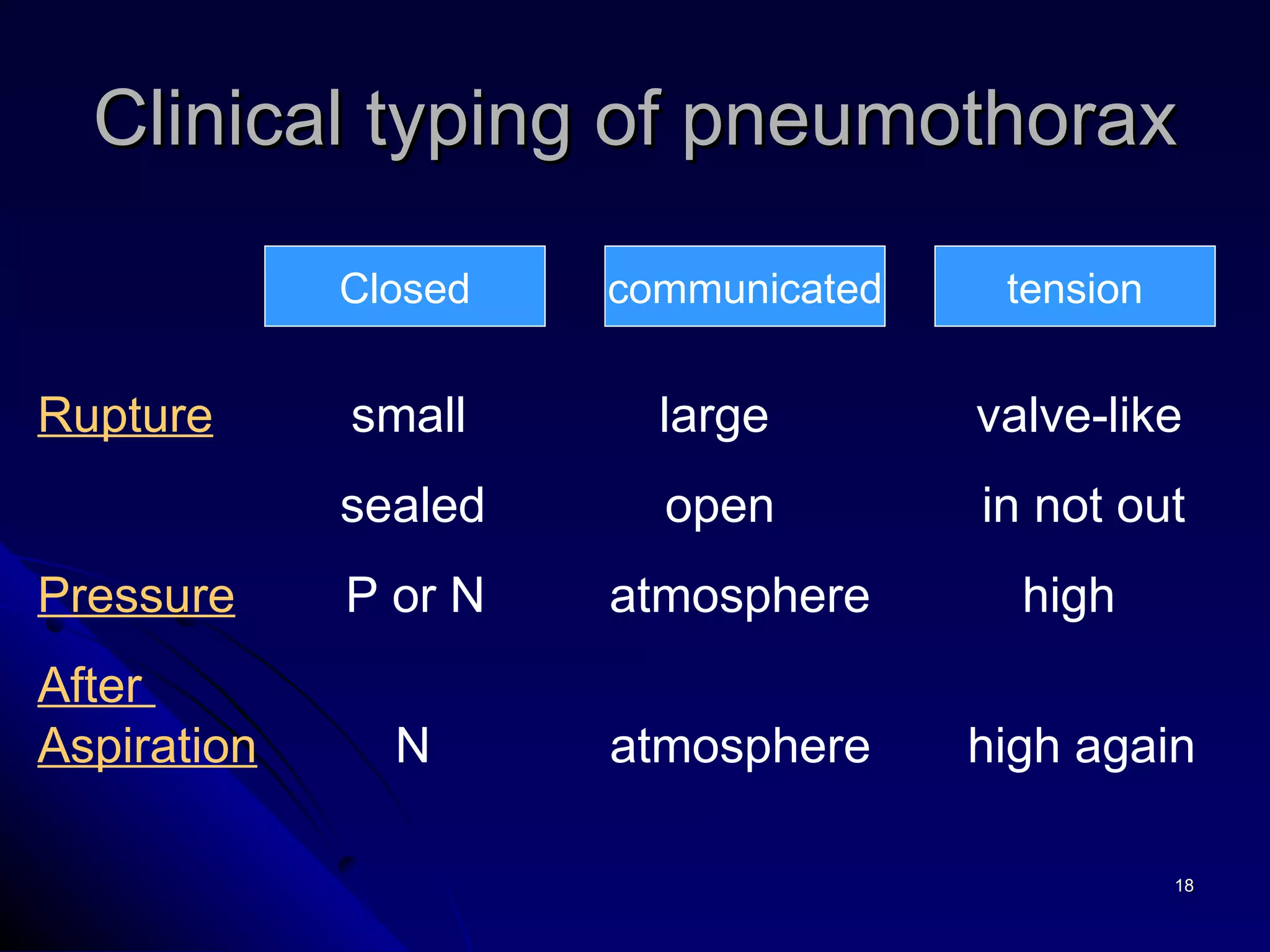
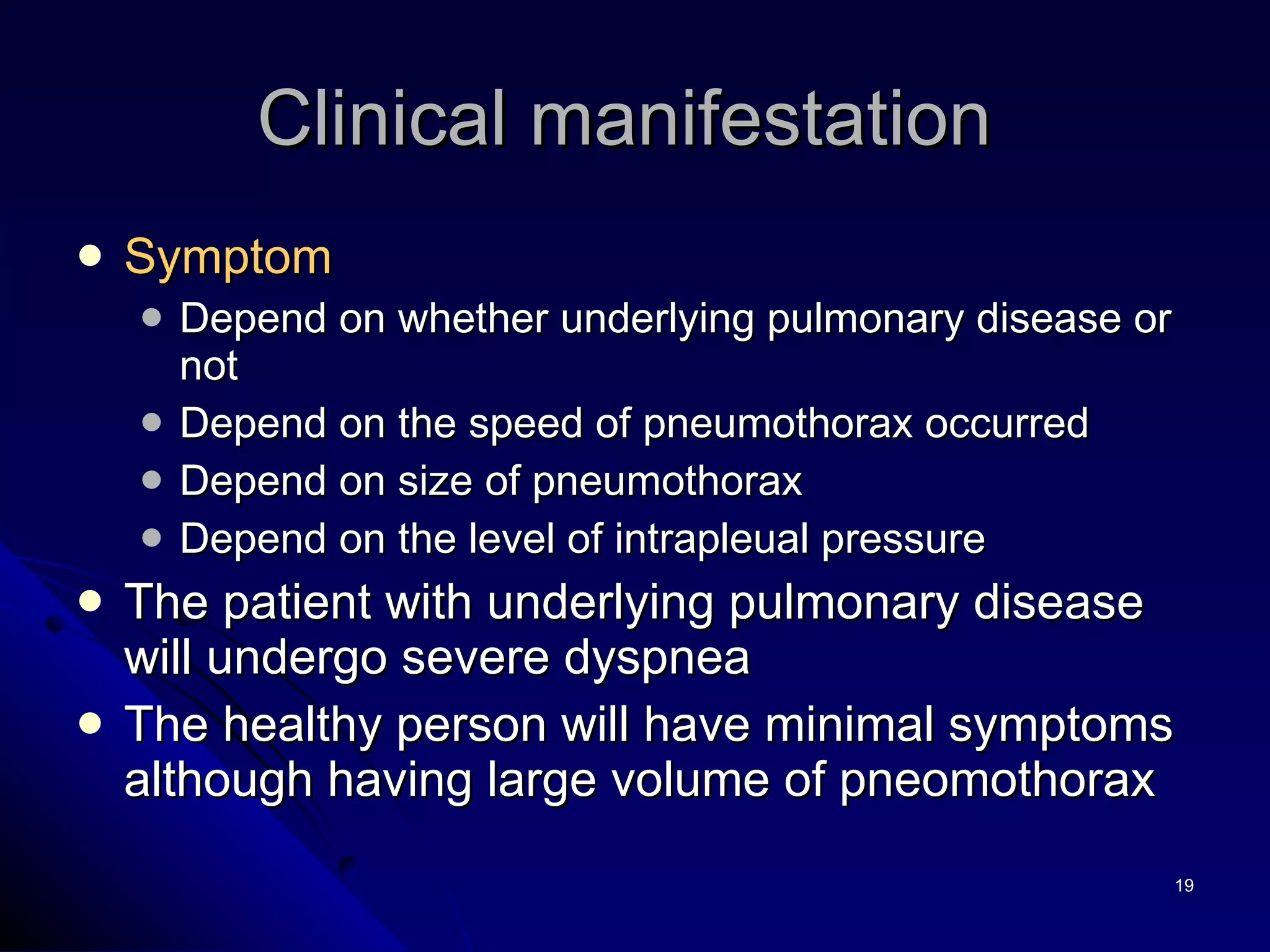
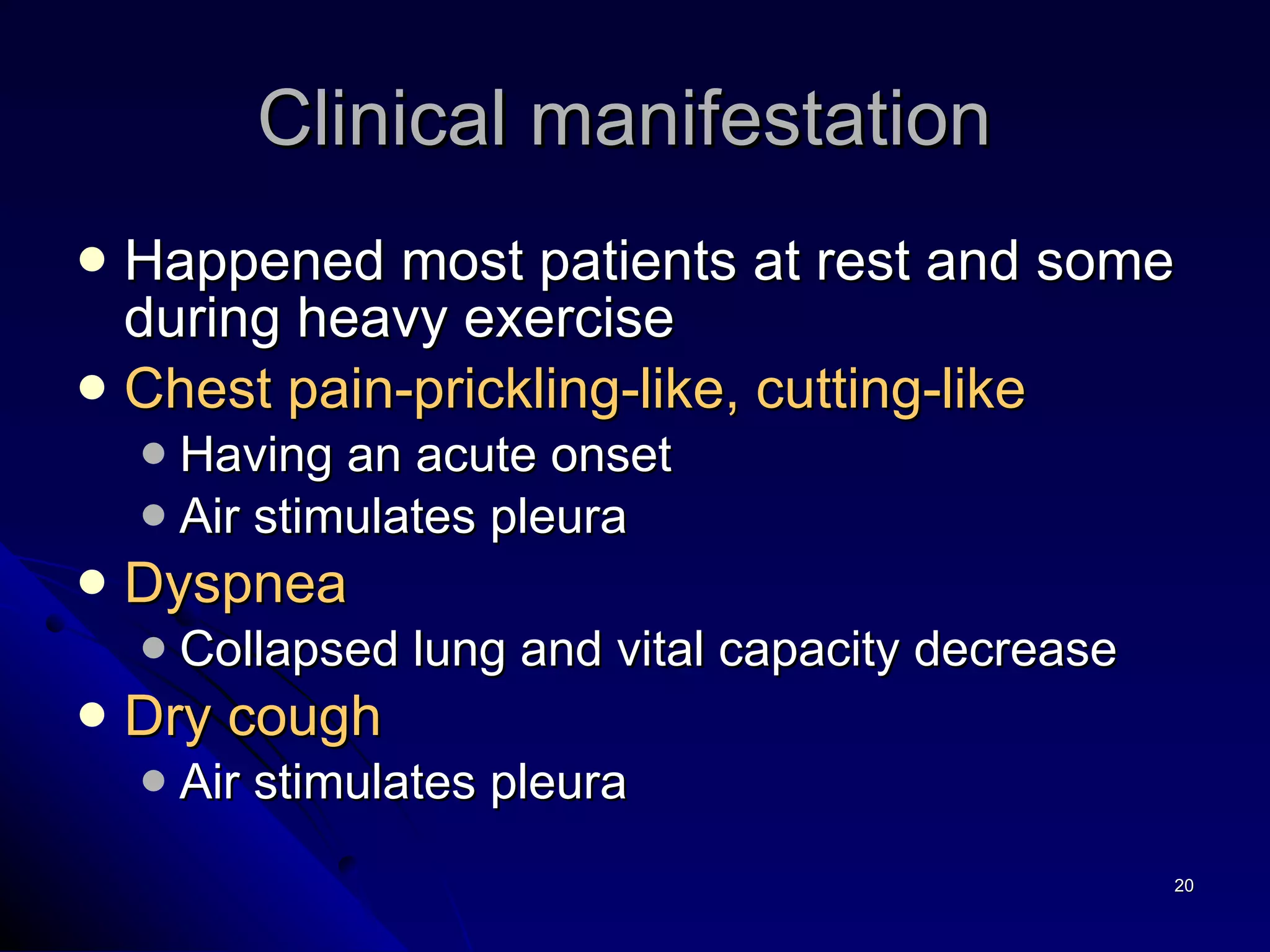
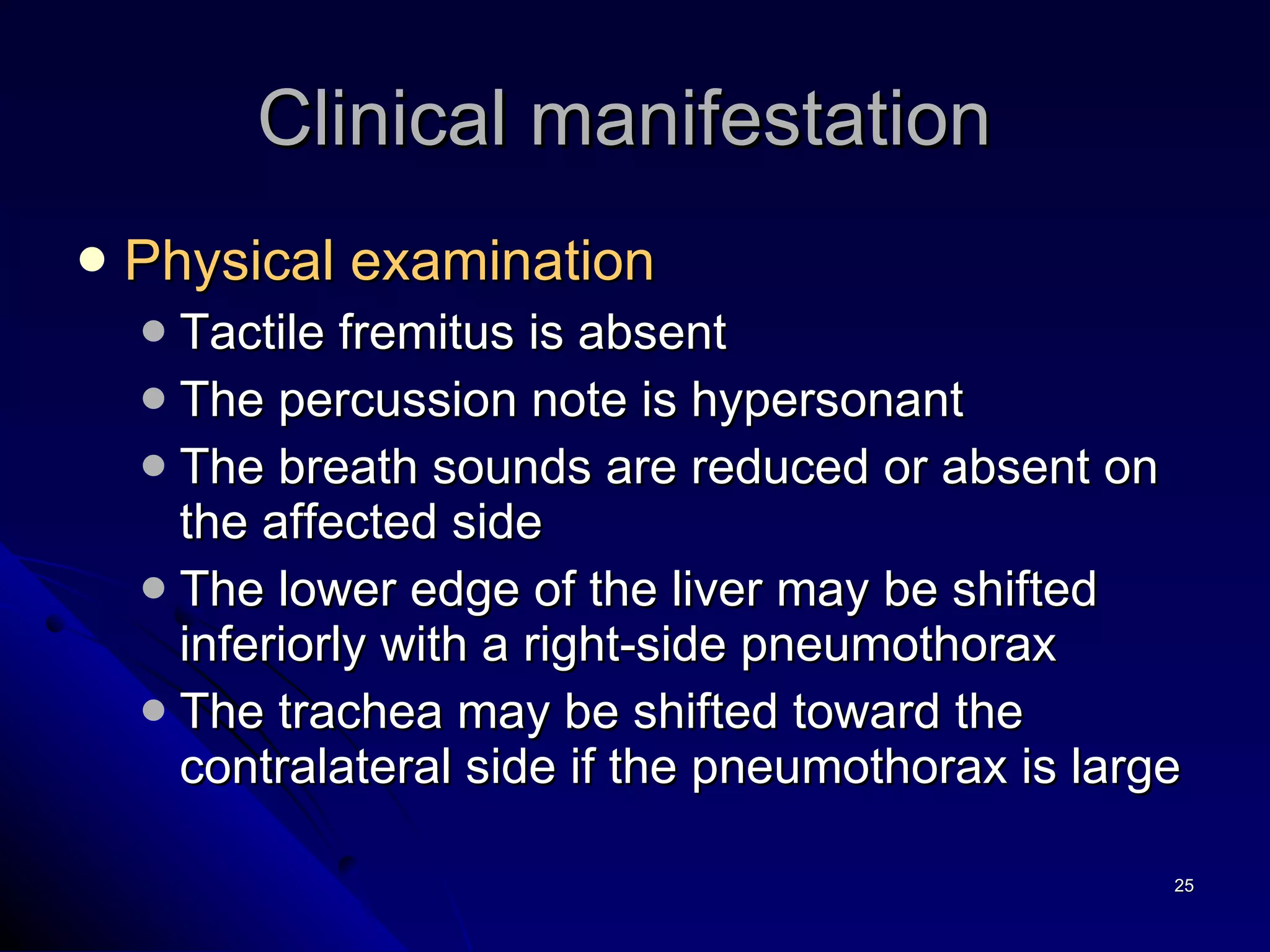
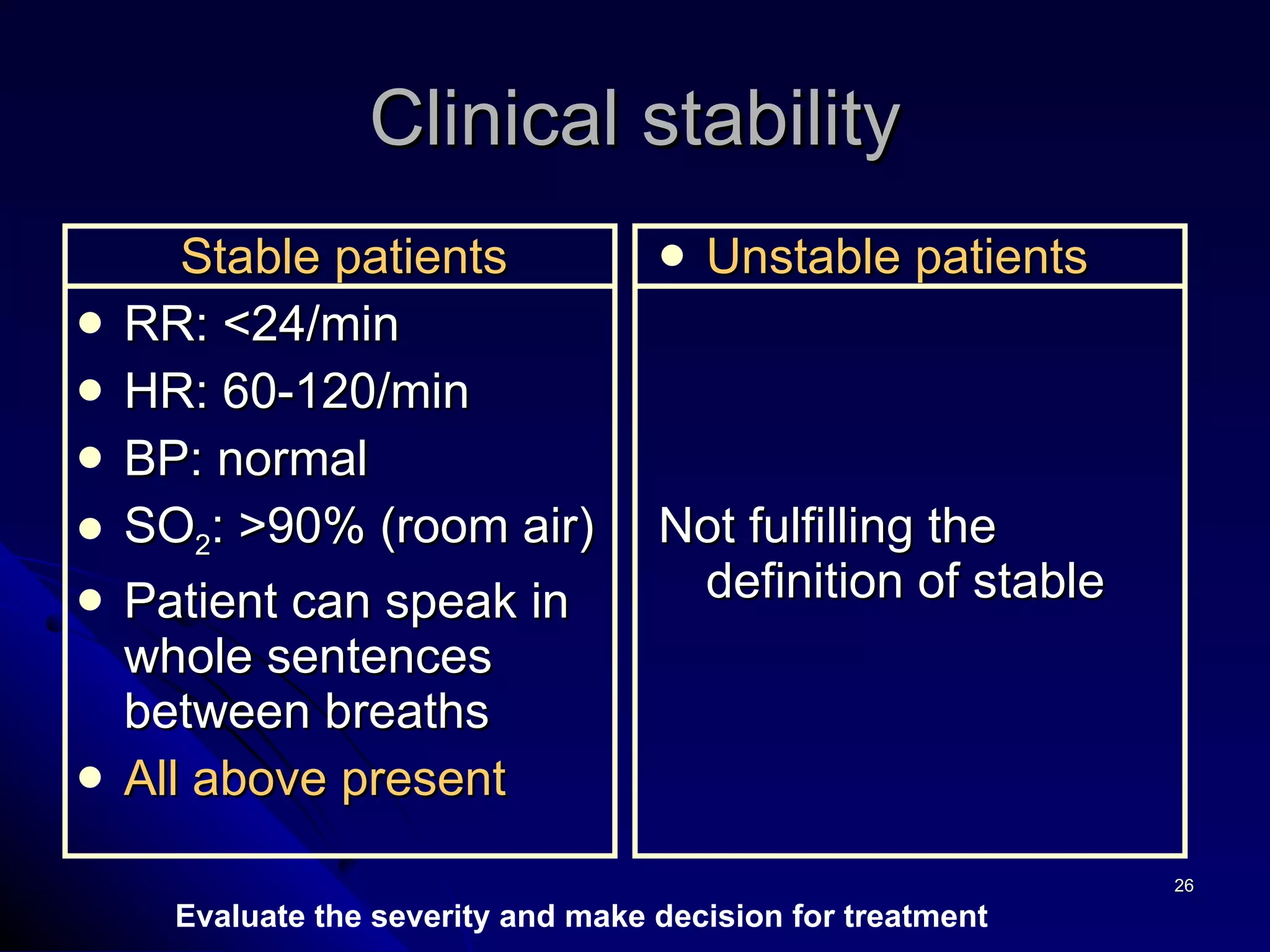
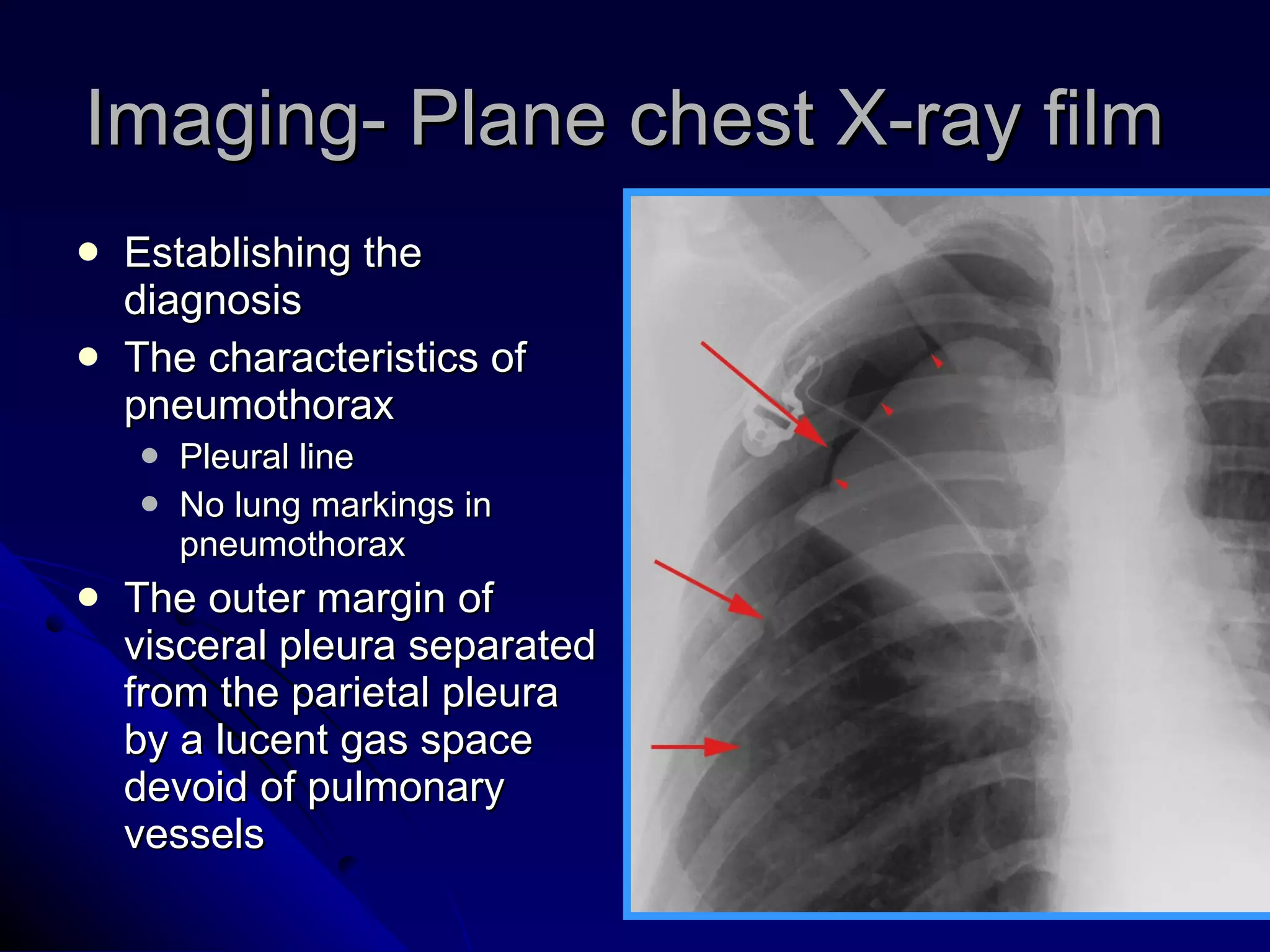
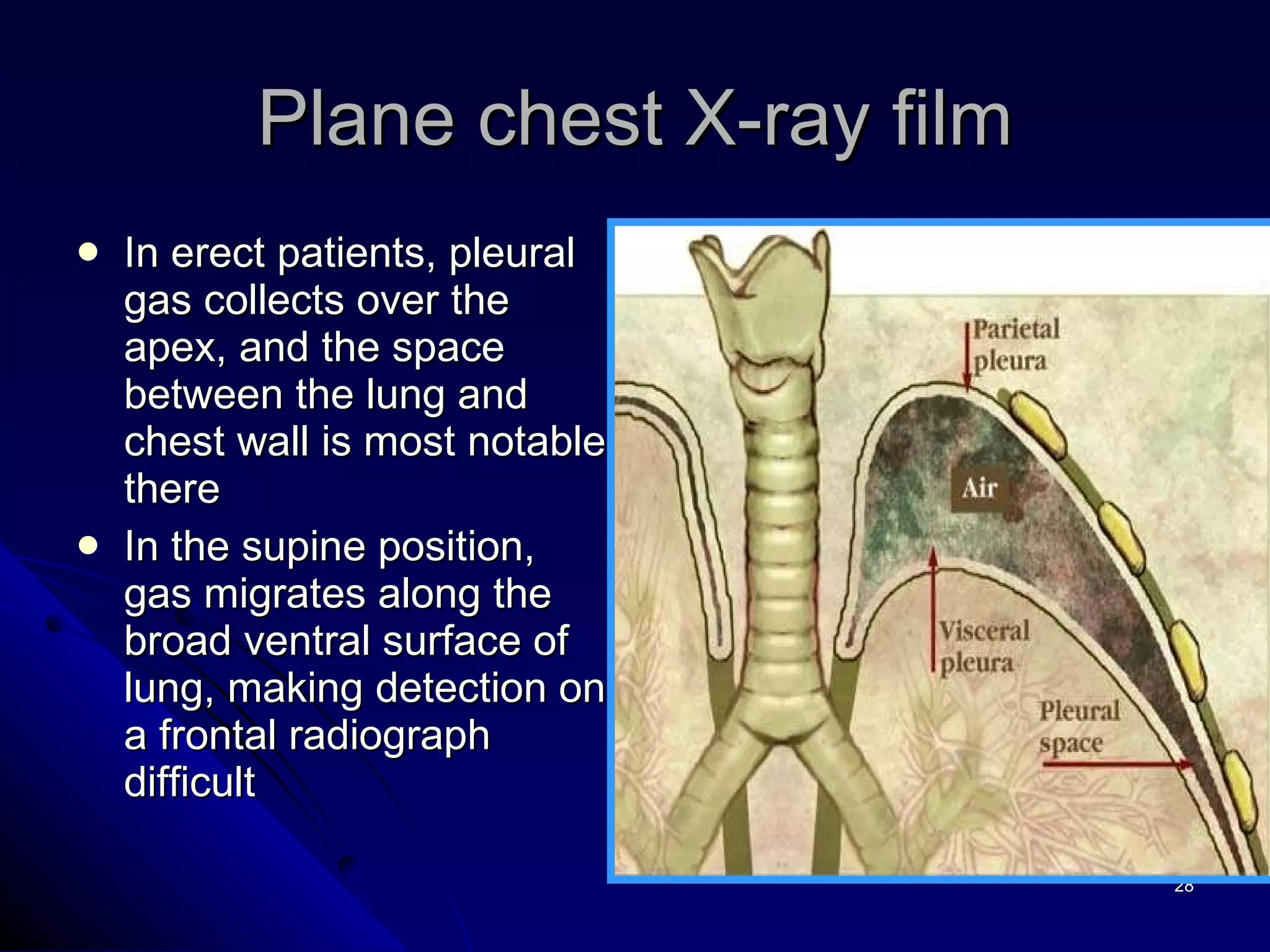
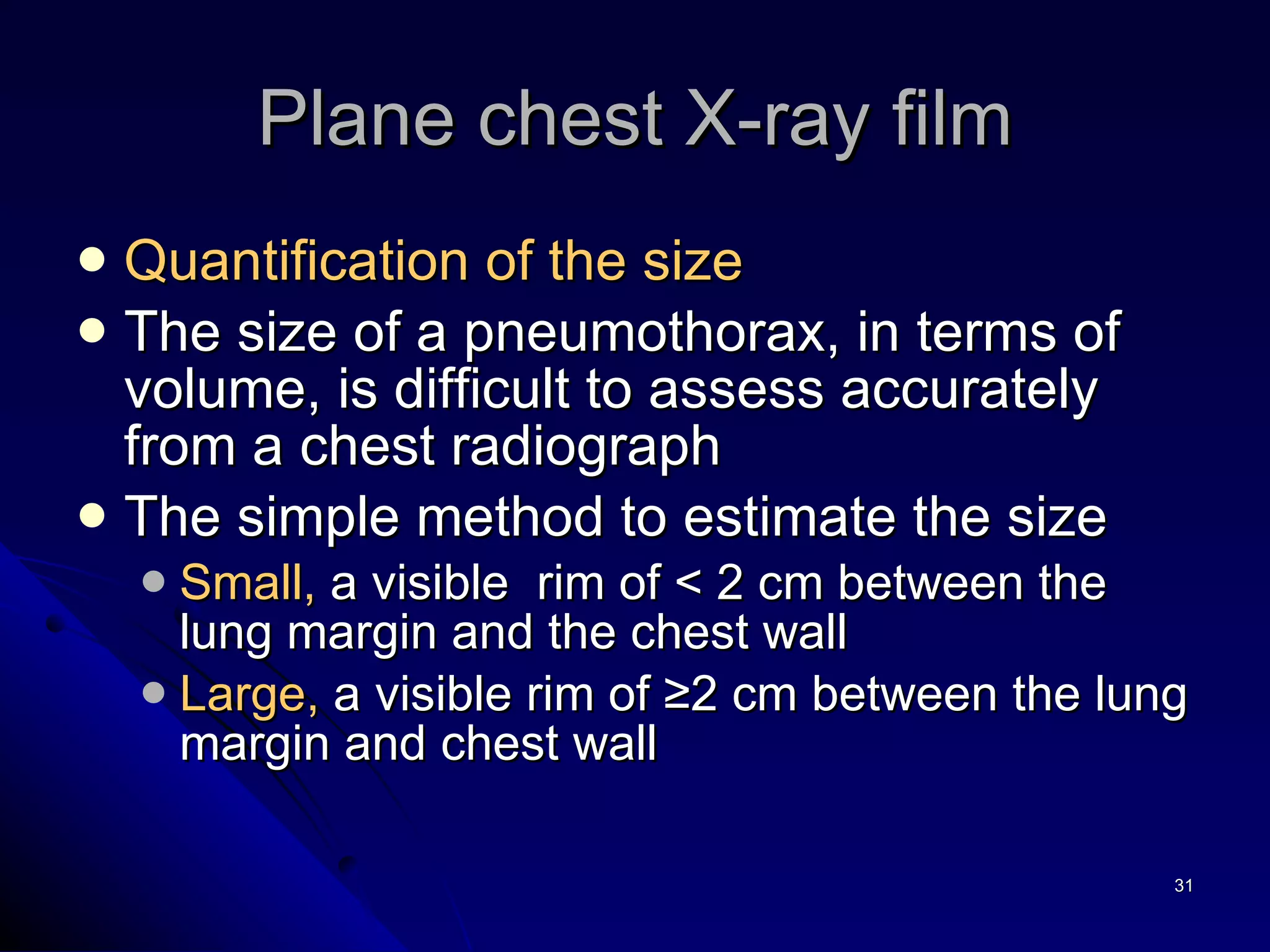
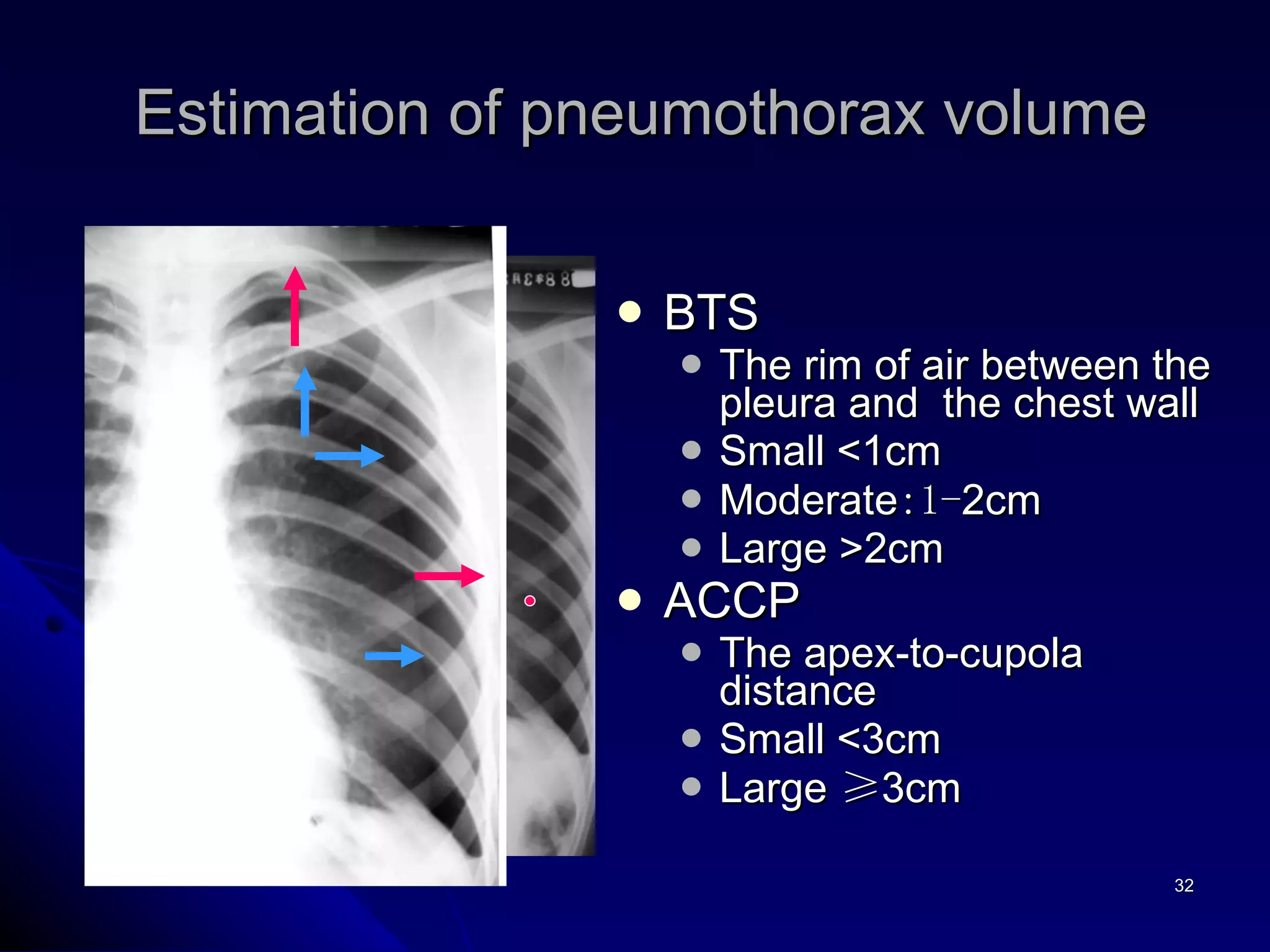
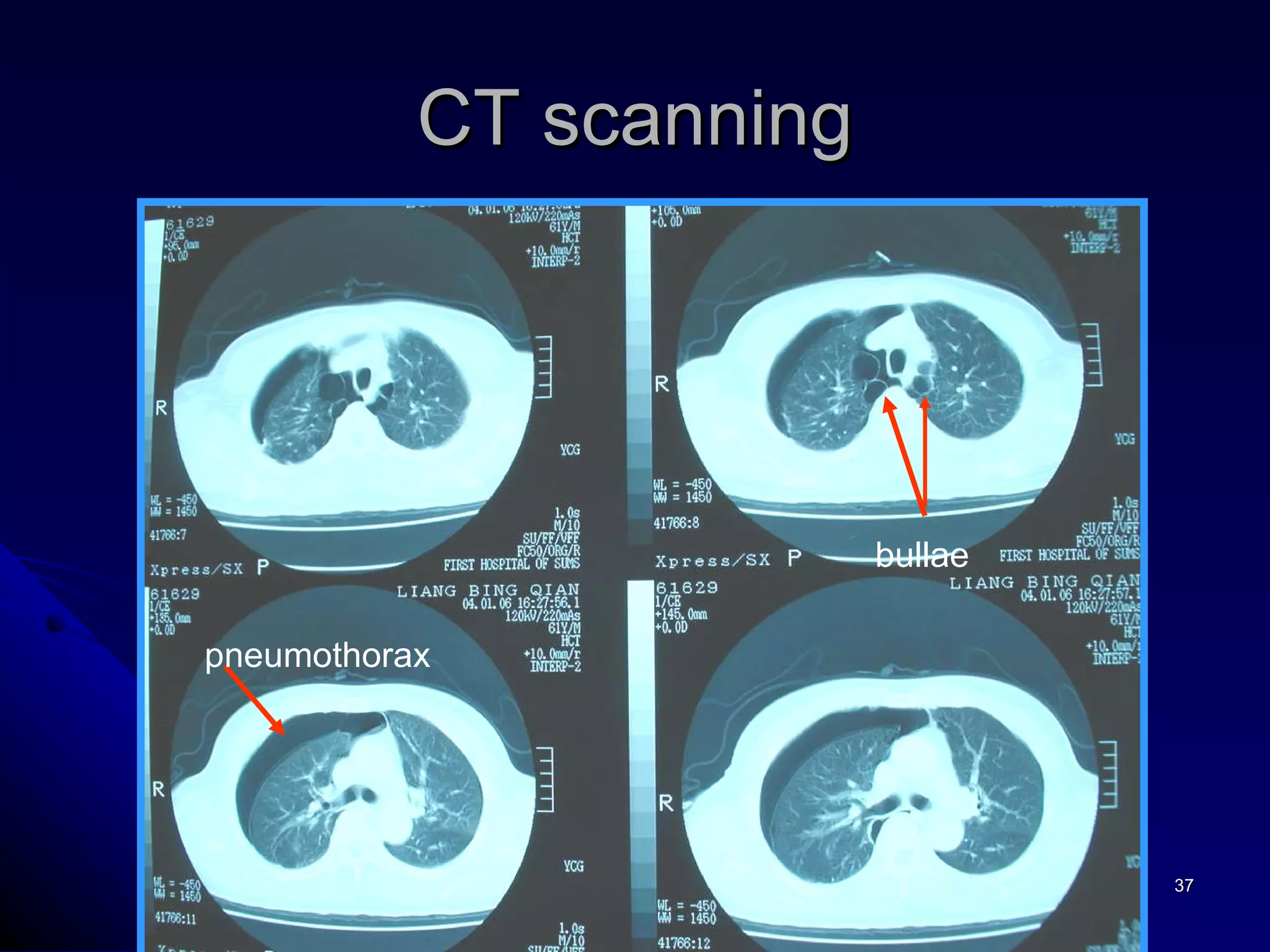
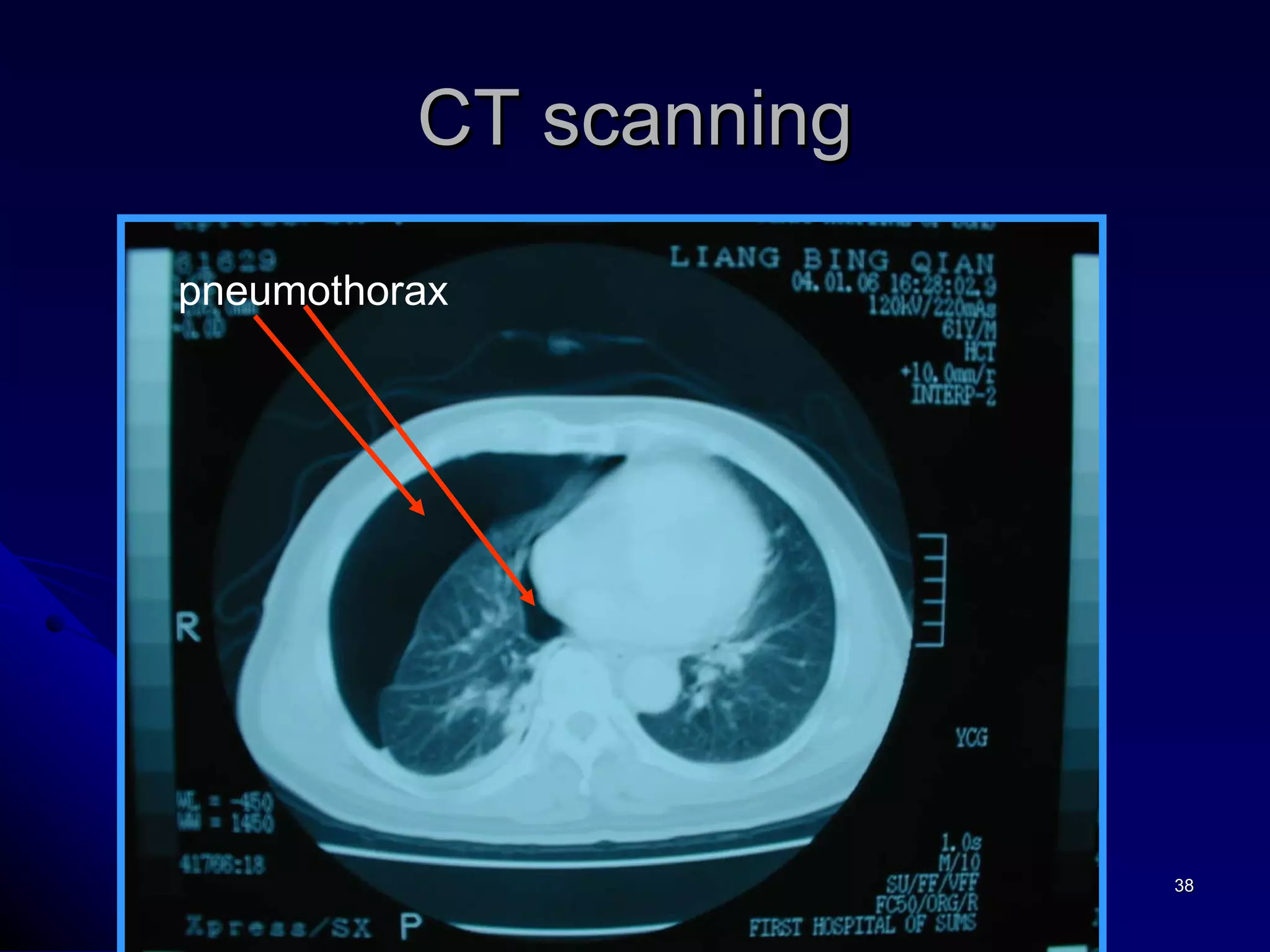
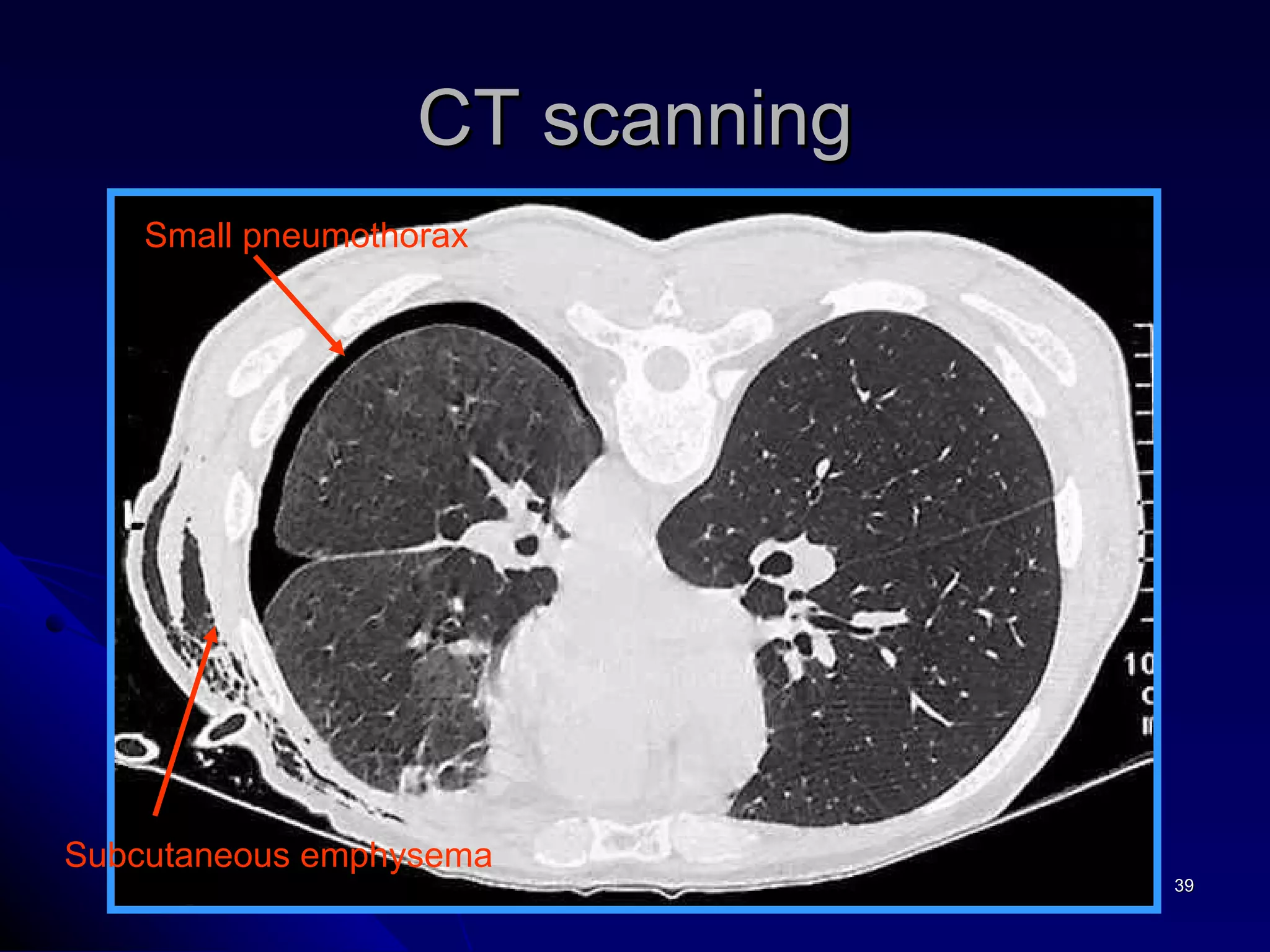
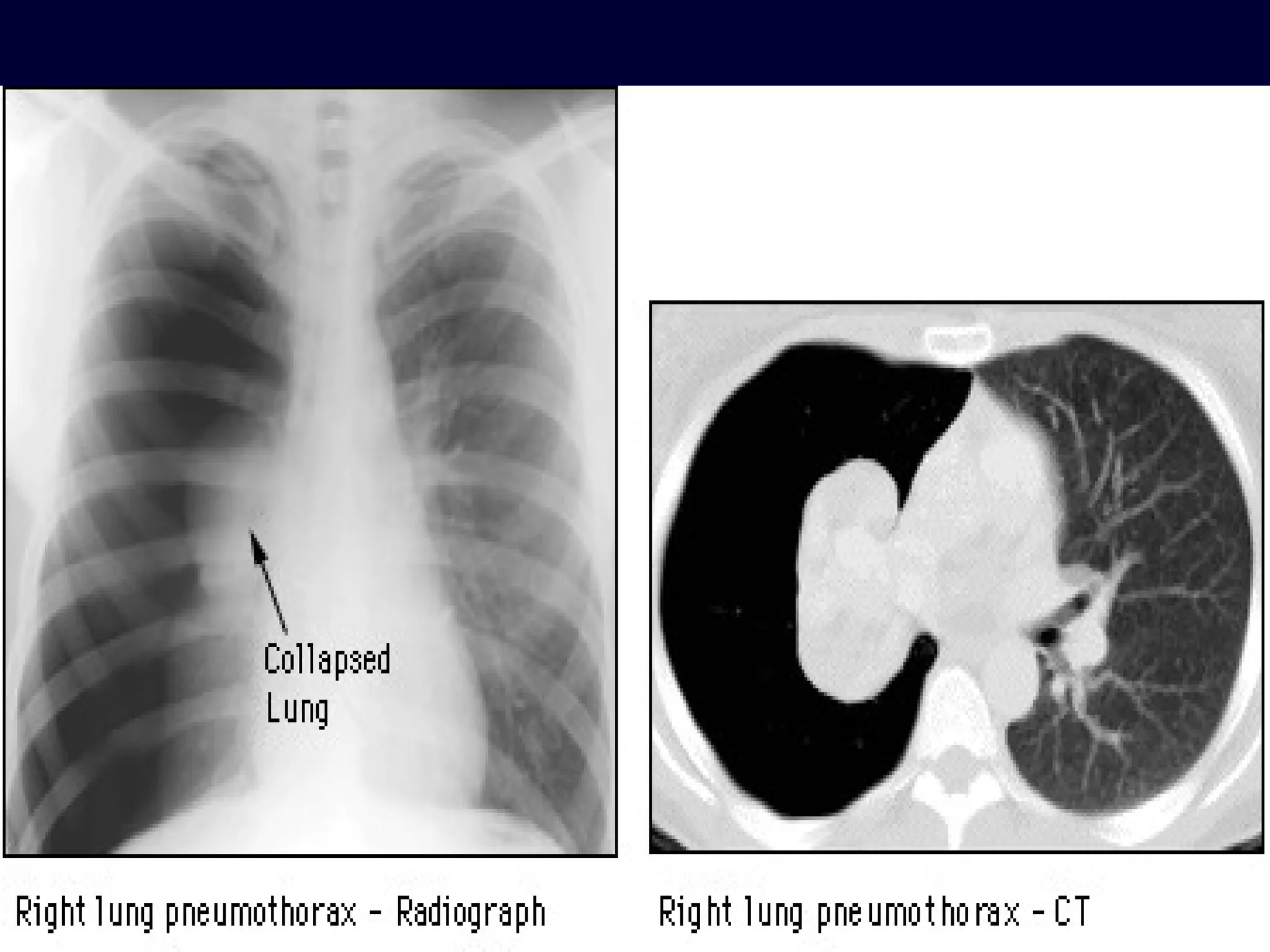
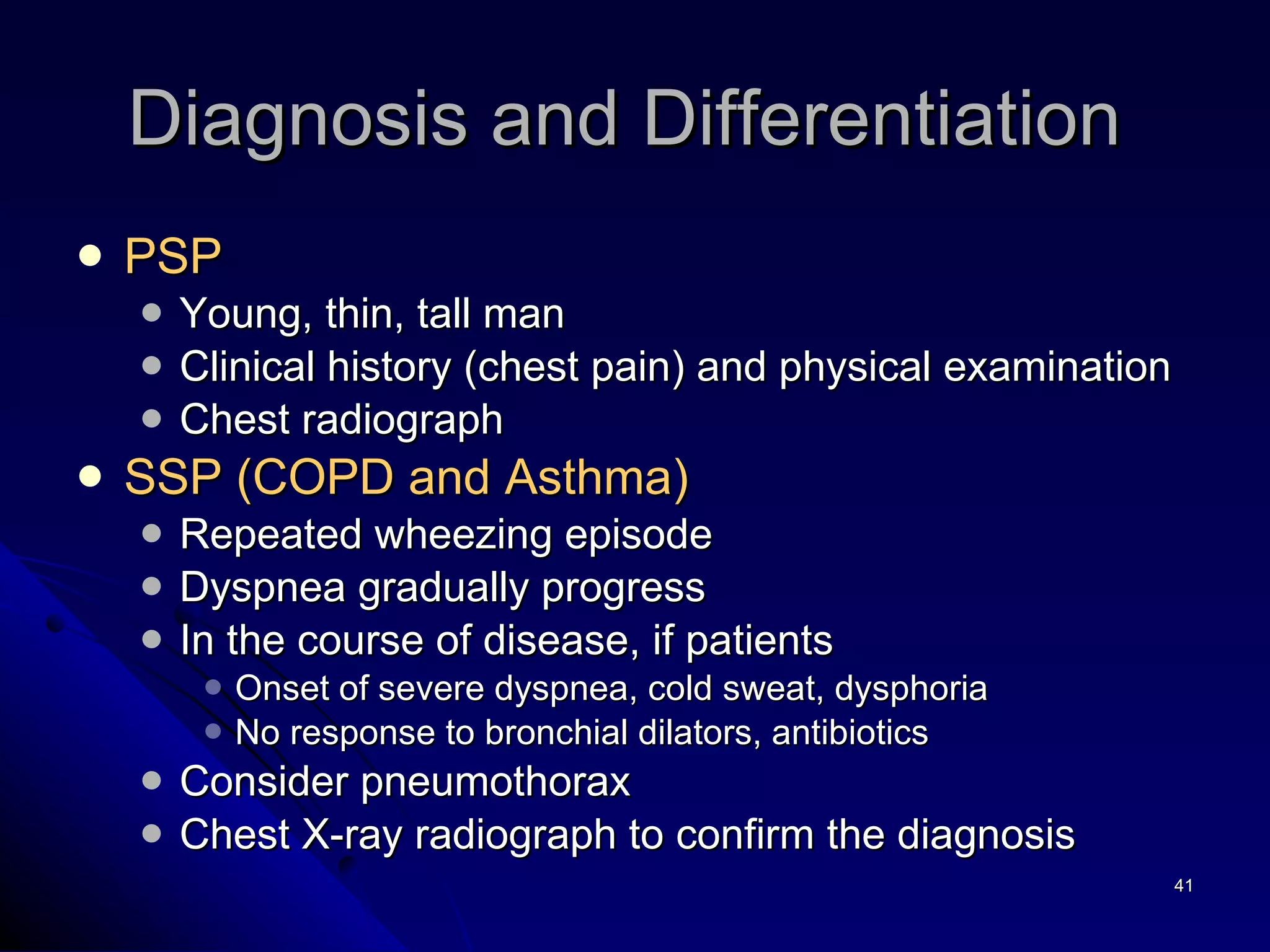
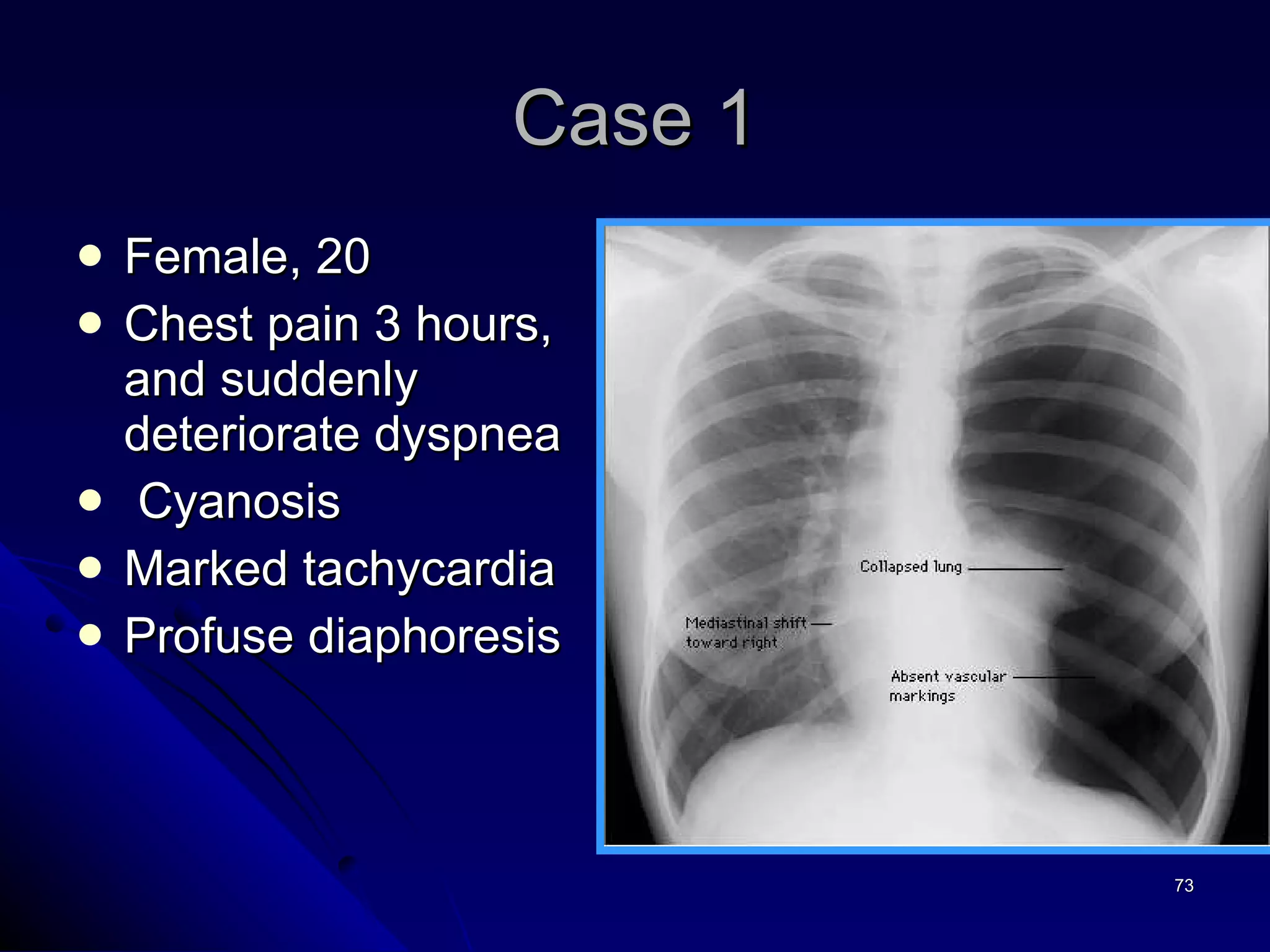
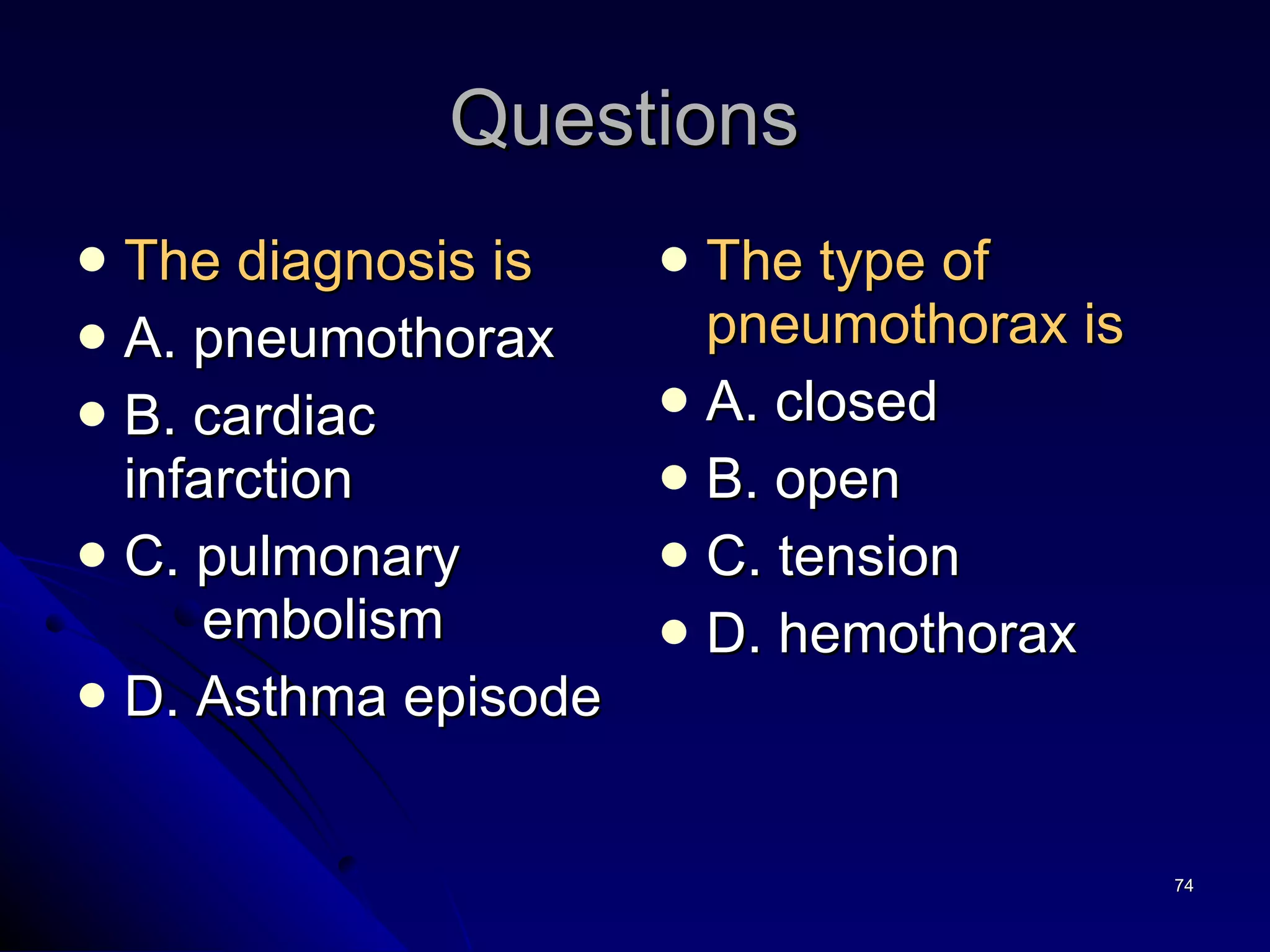
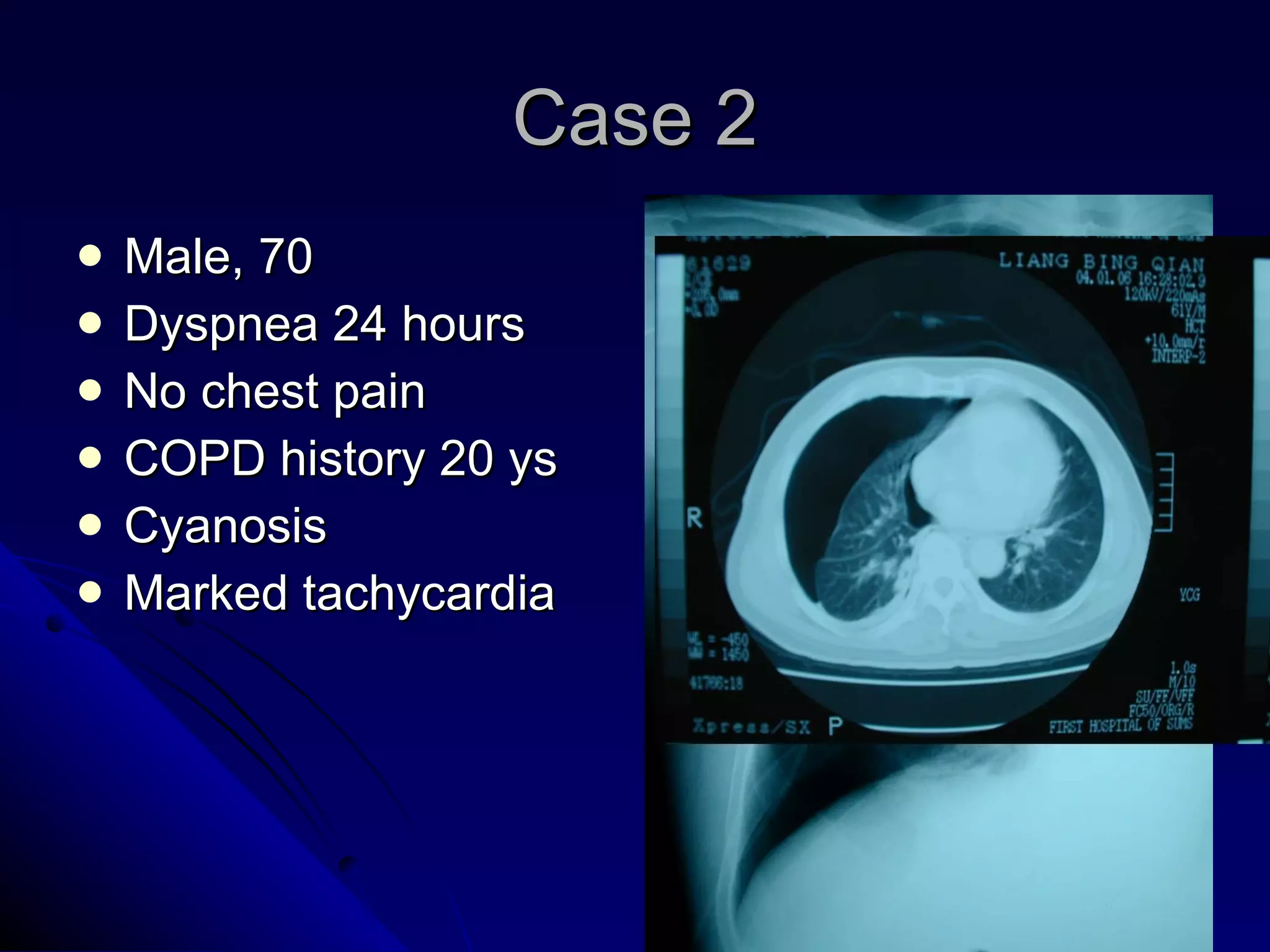
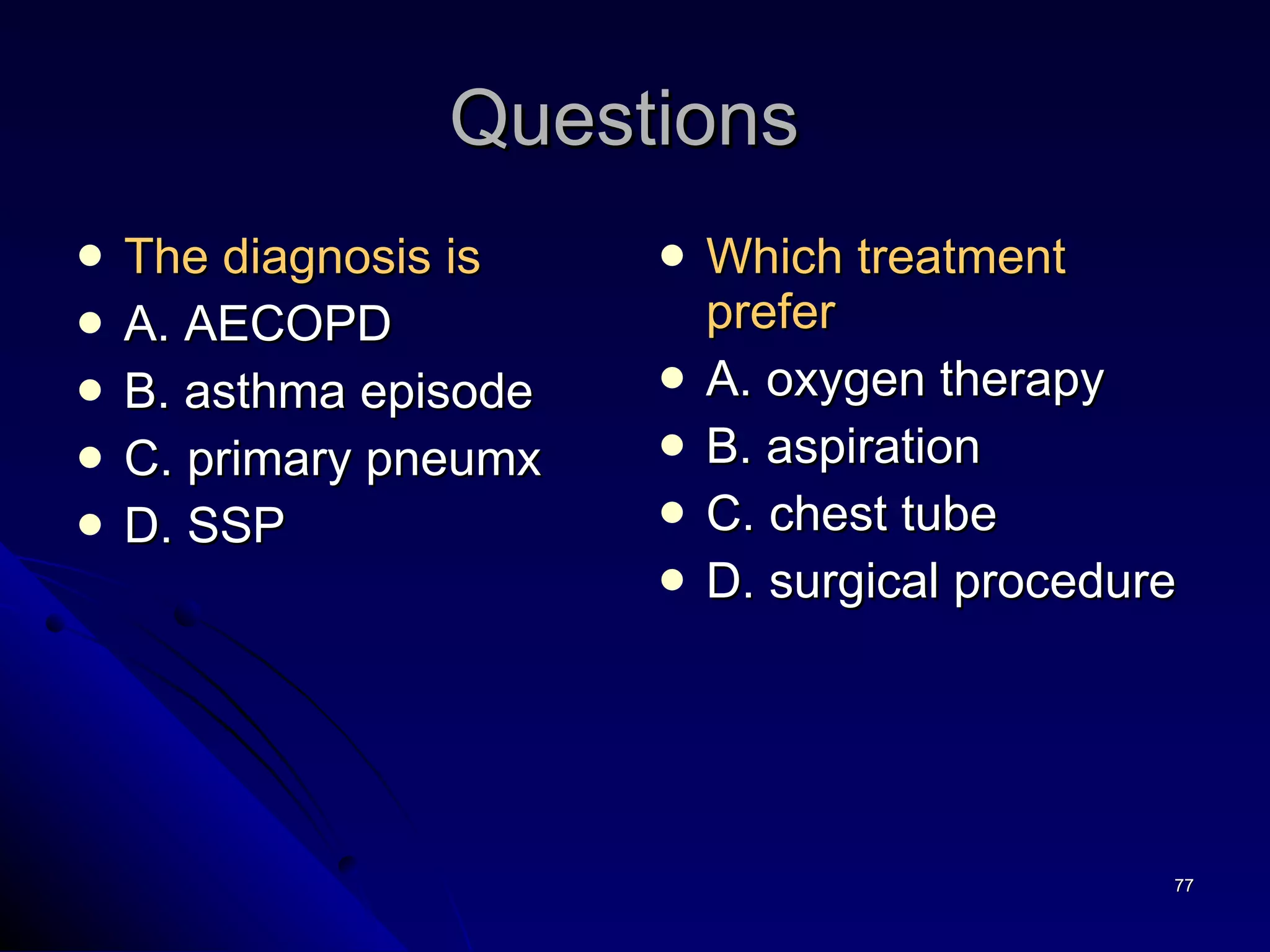
- The document discusses pneumothorax, describing its classification, pathogenesis, clinical presentation, diagnosis, and treatment options.
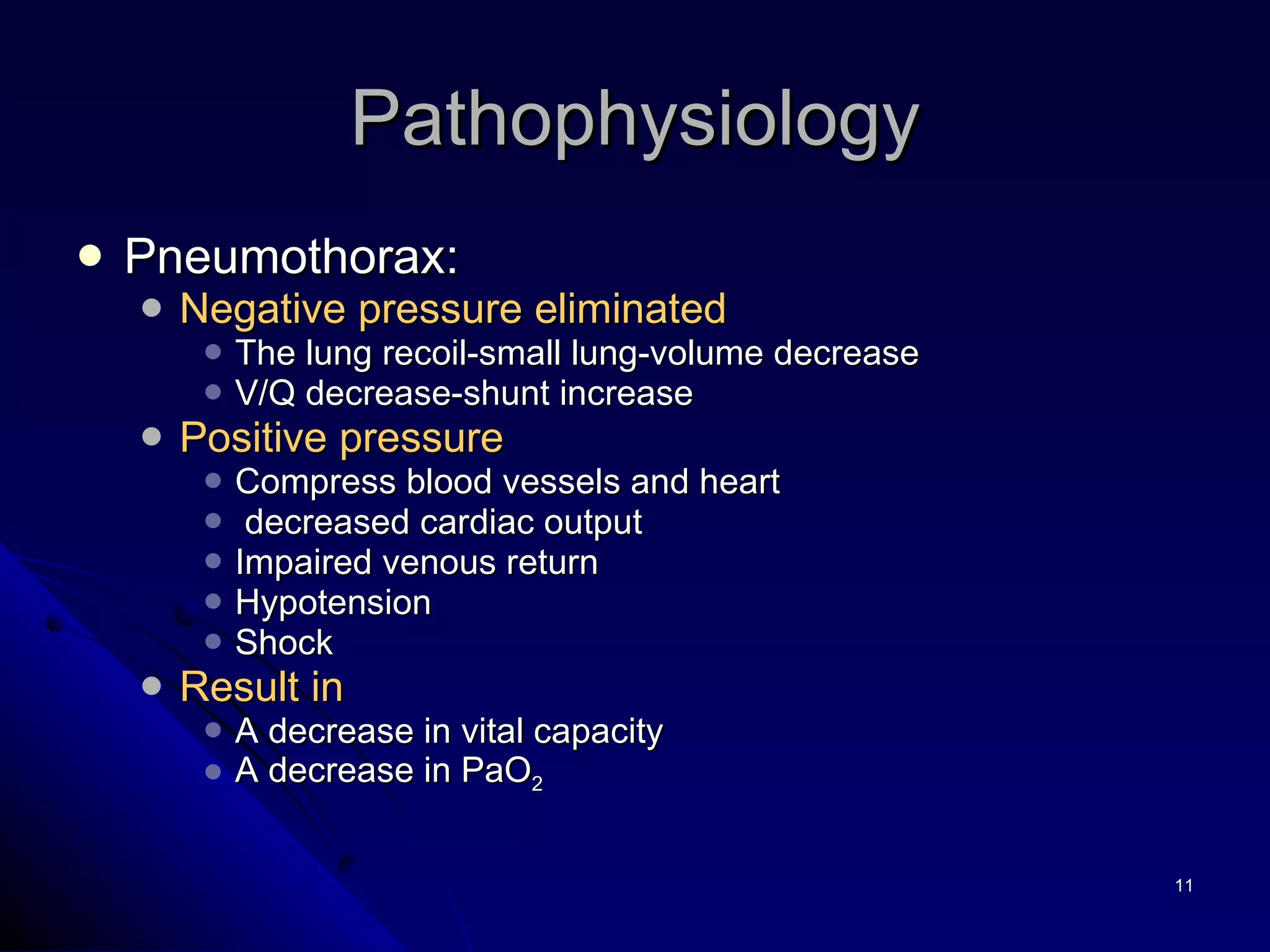
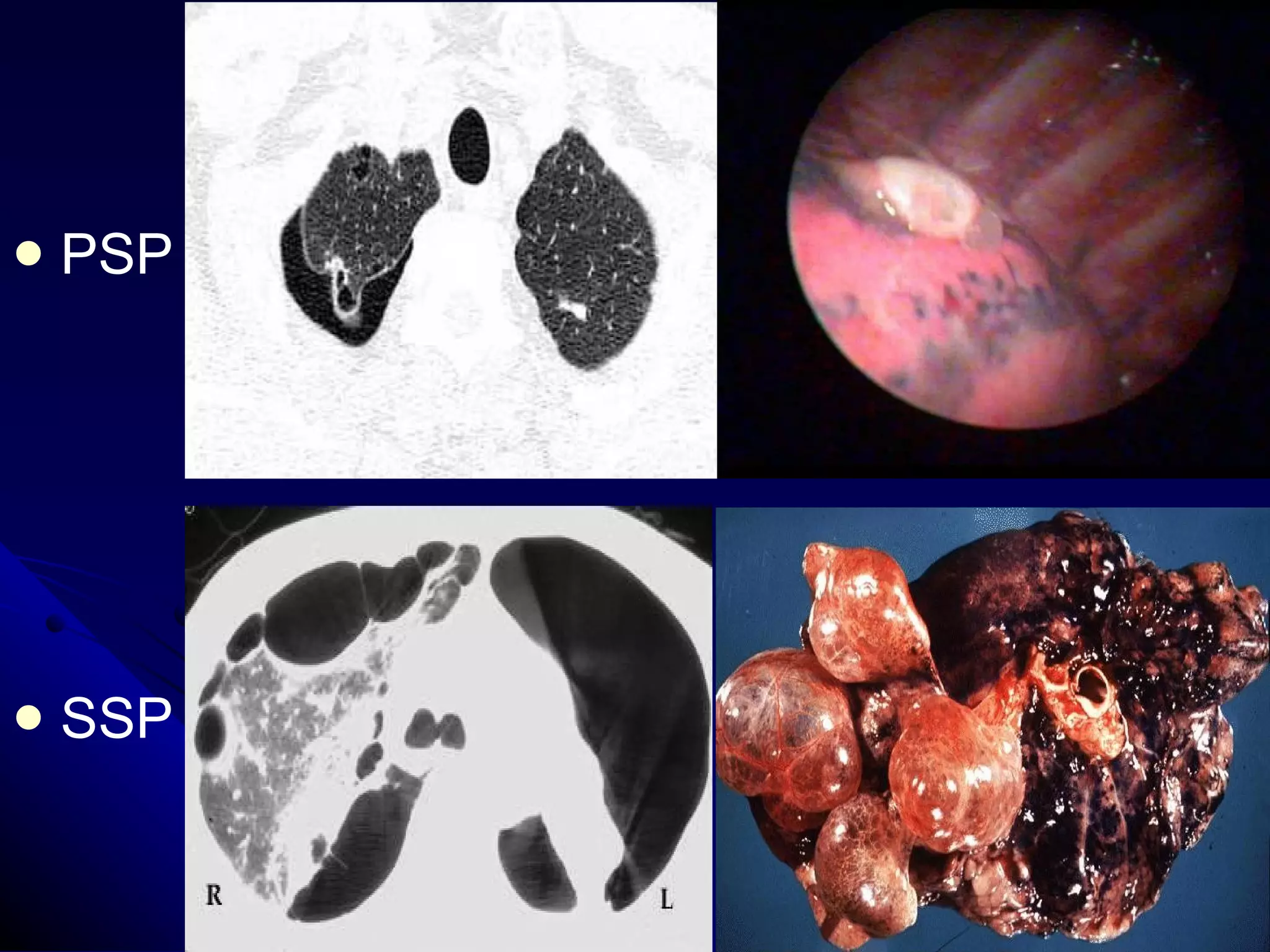
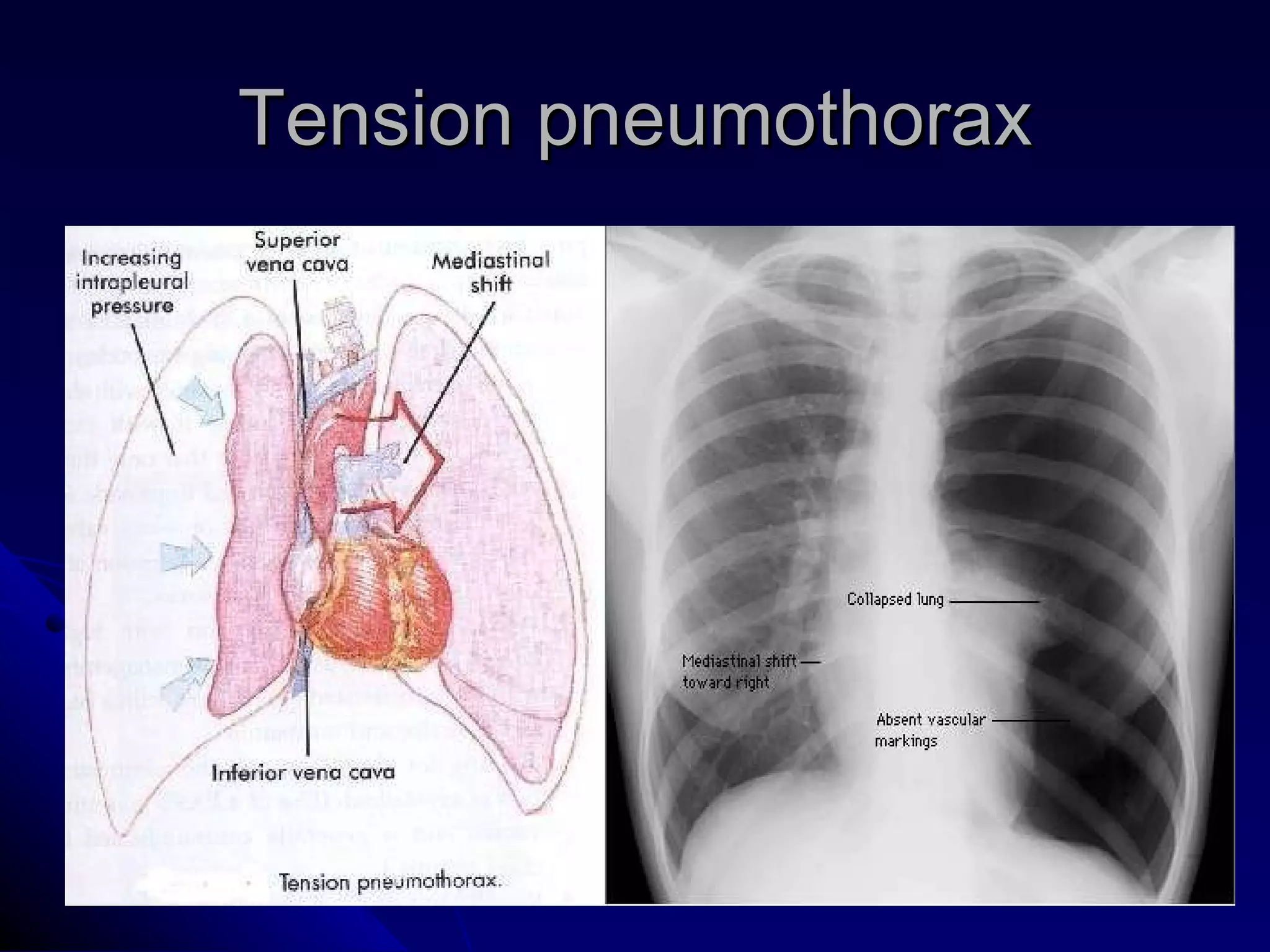
- Key points include that tension pneumothorax can cause rapid deterioration and requires immediate treatment, while spontaneous pneumothorax is classified as primary or secondary depending on underlying lung health.
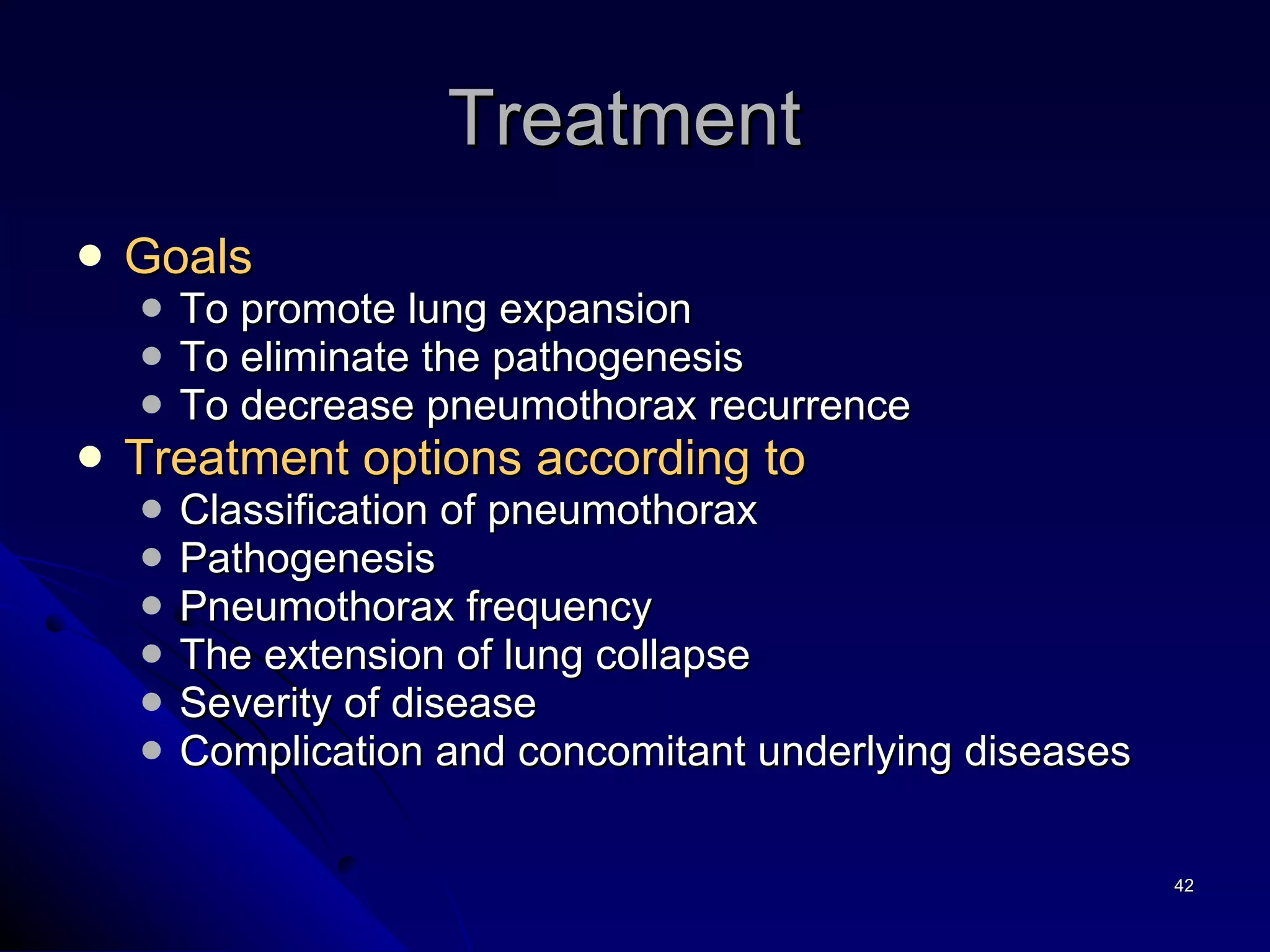
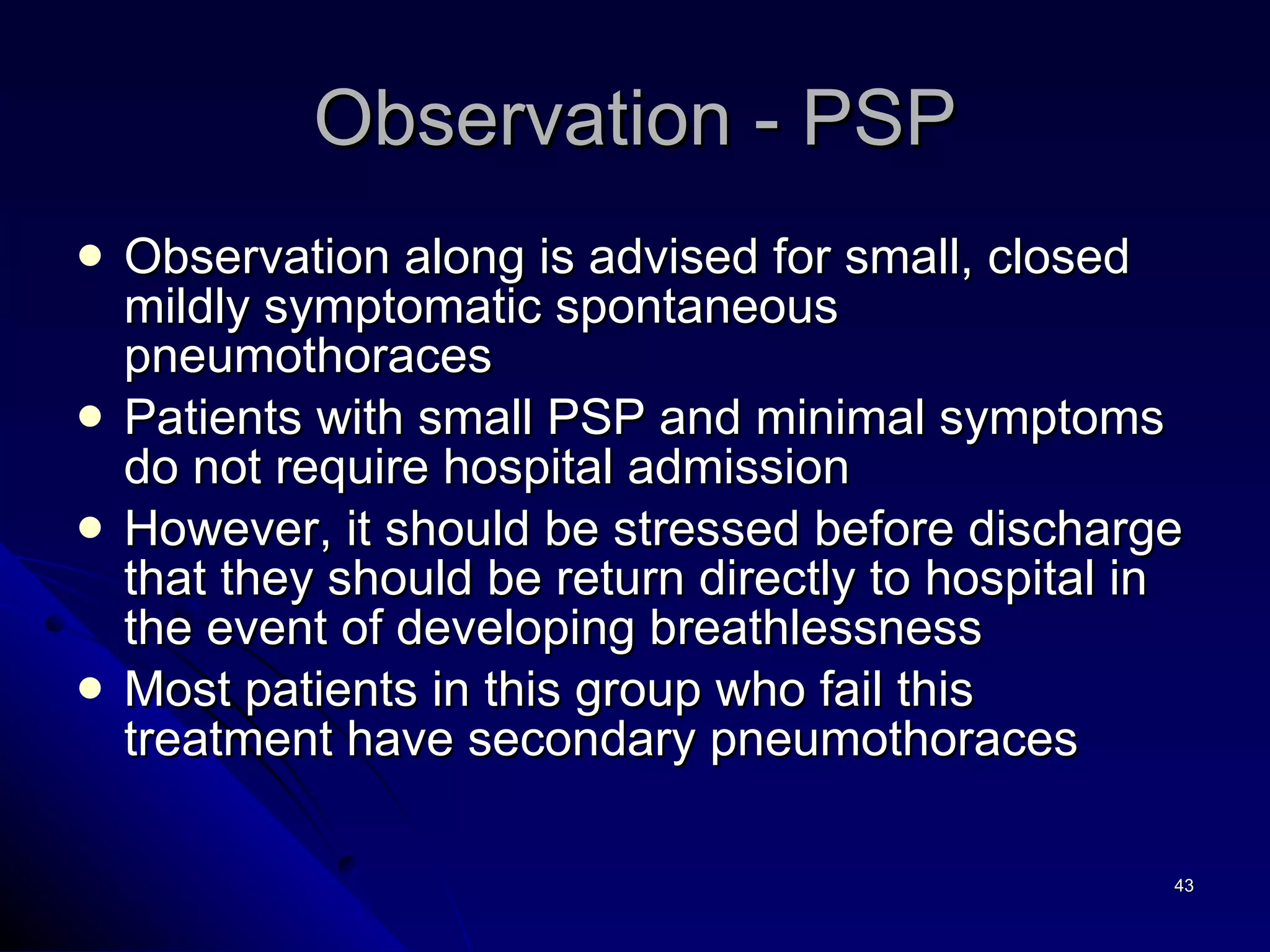
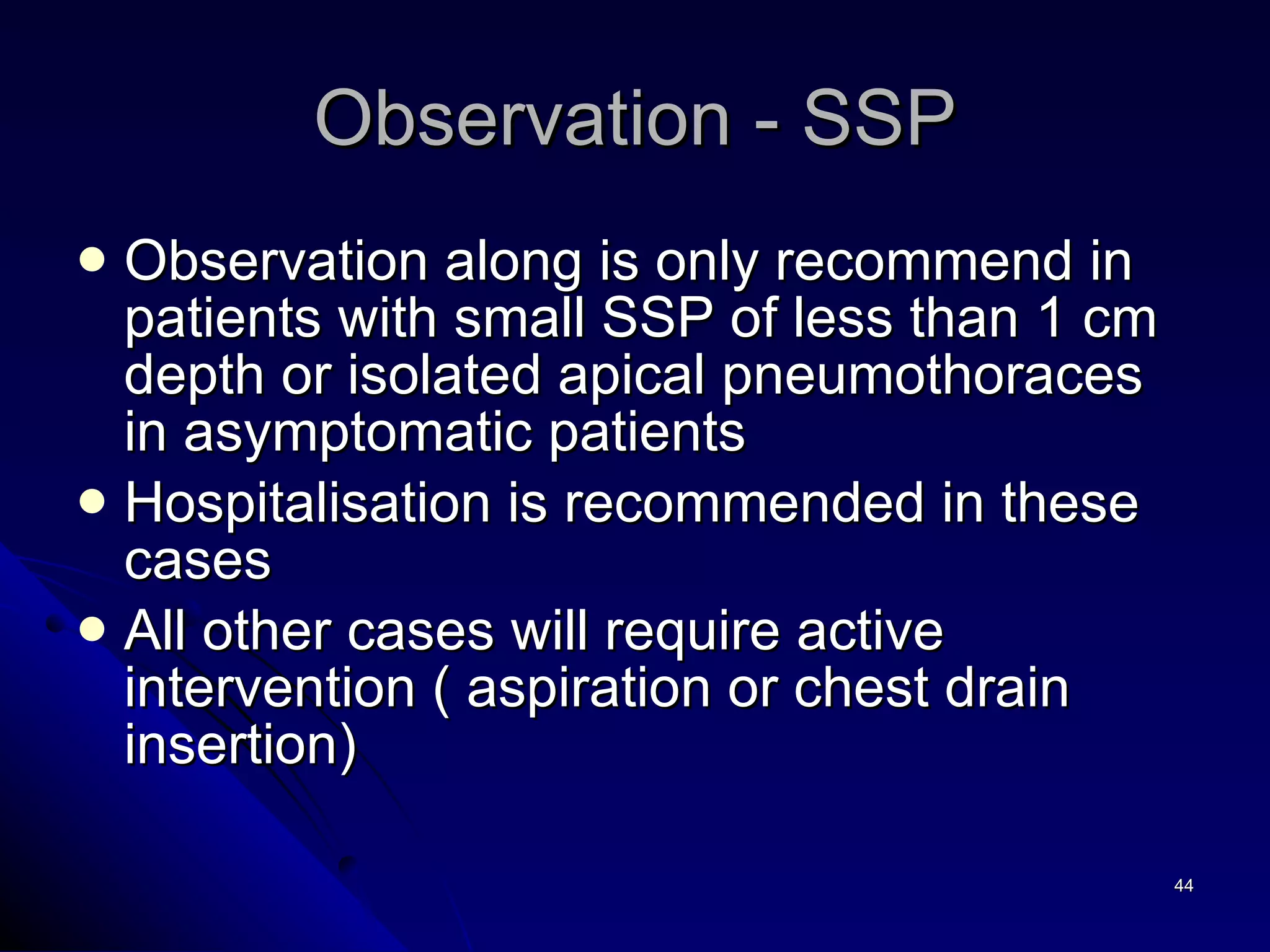
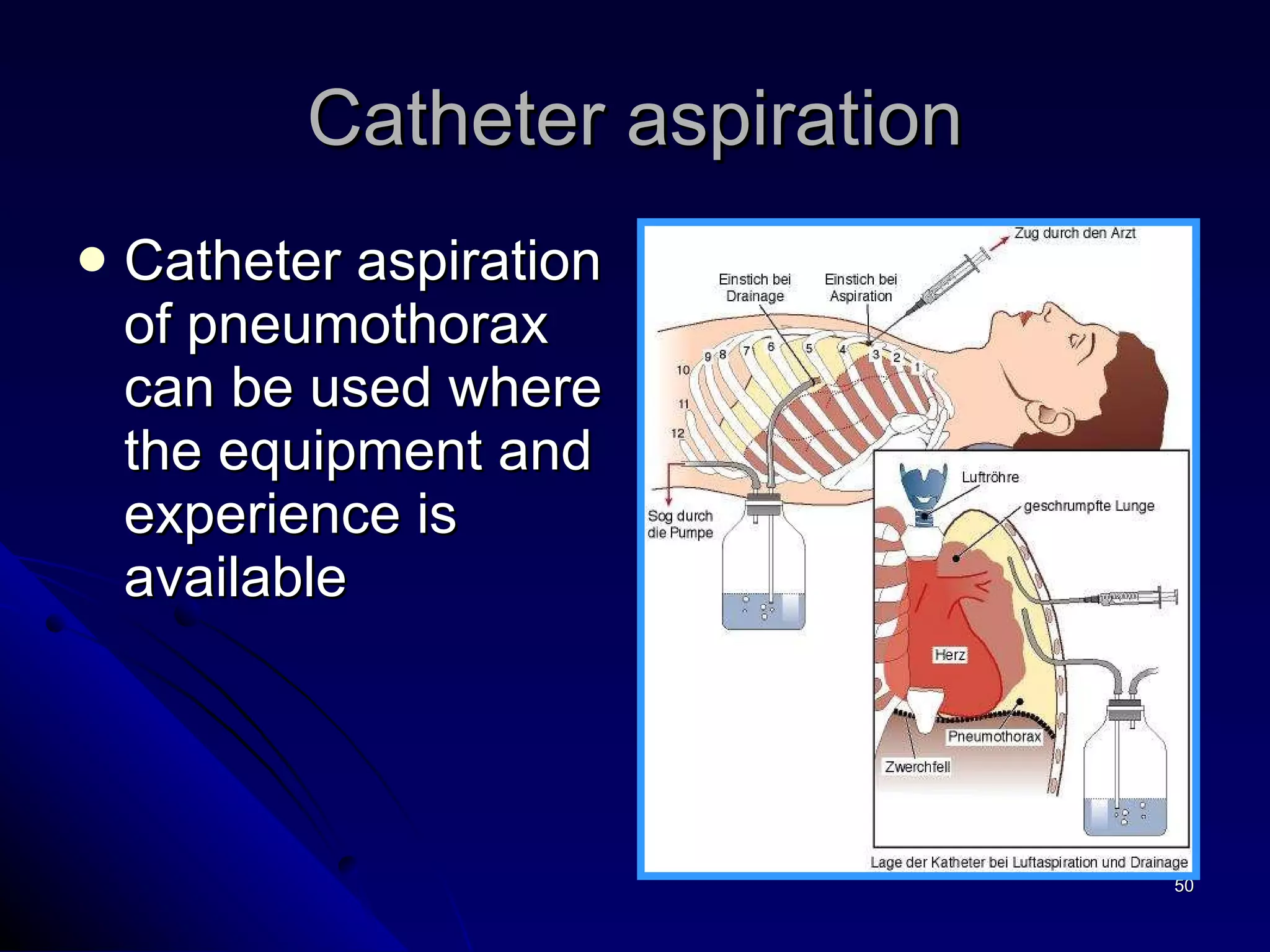
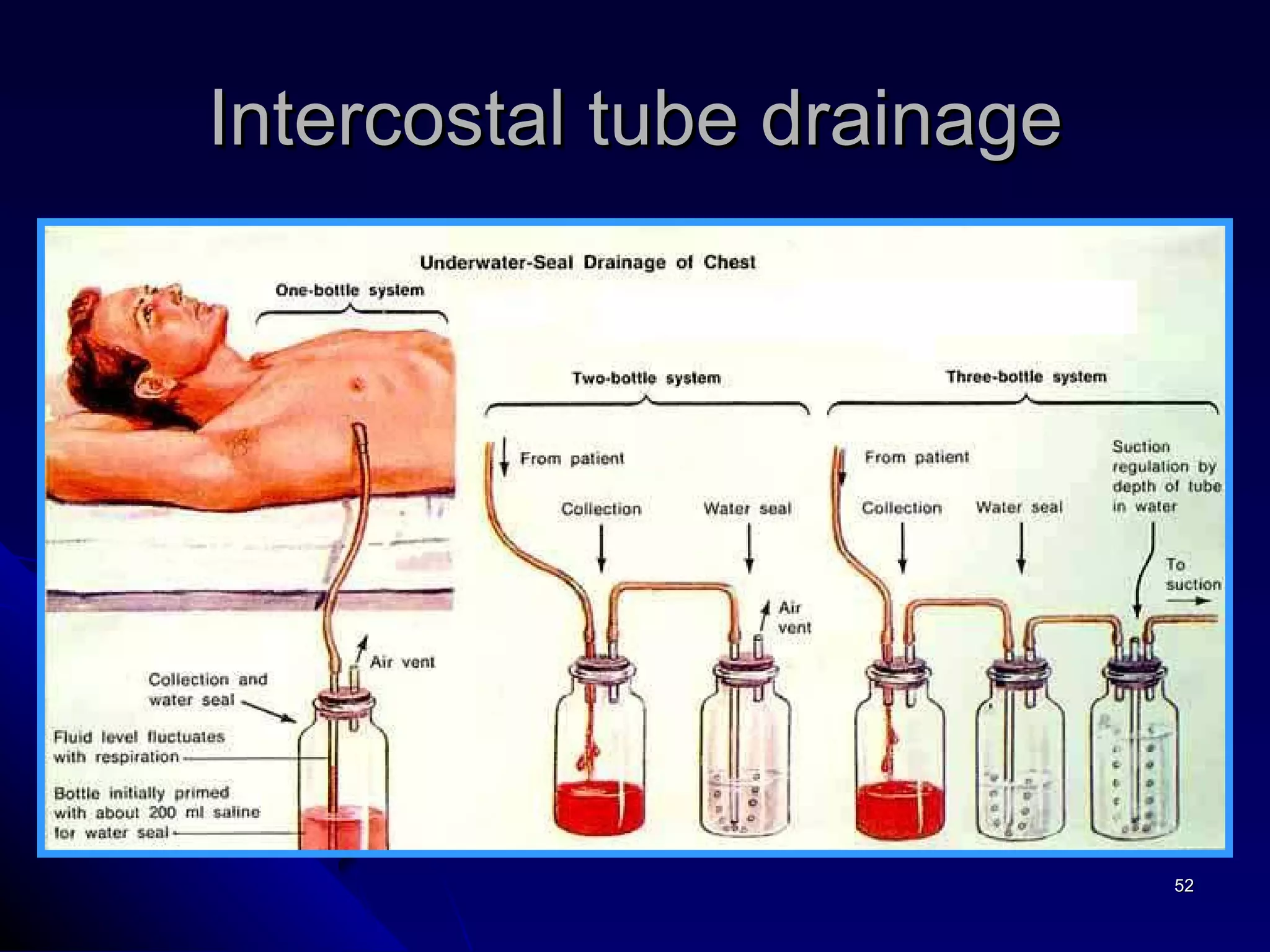
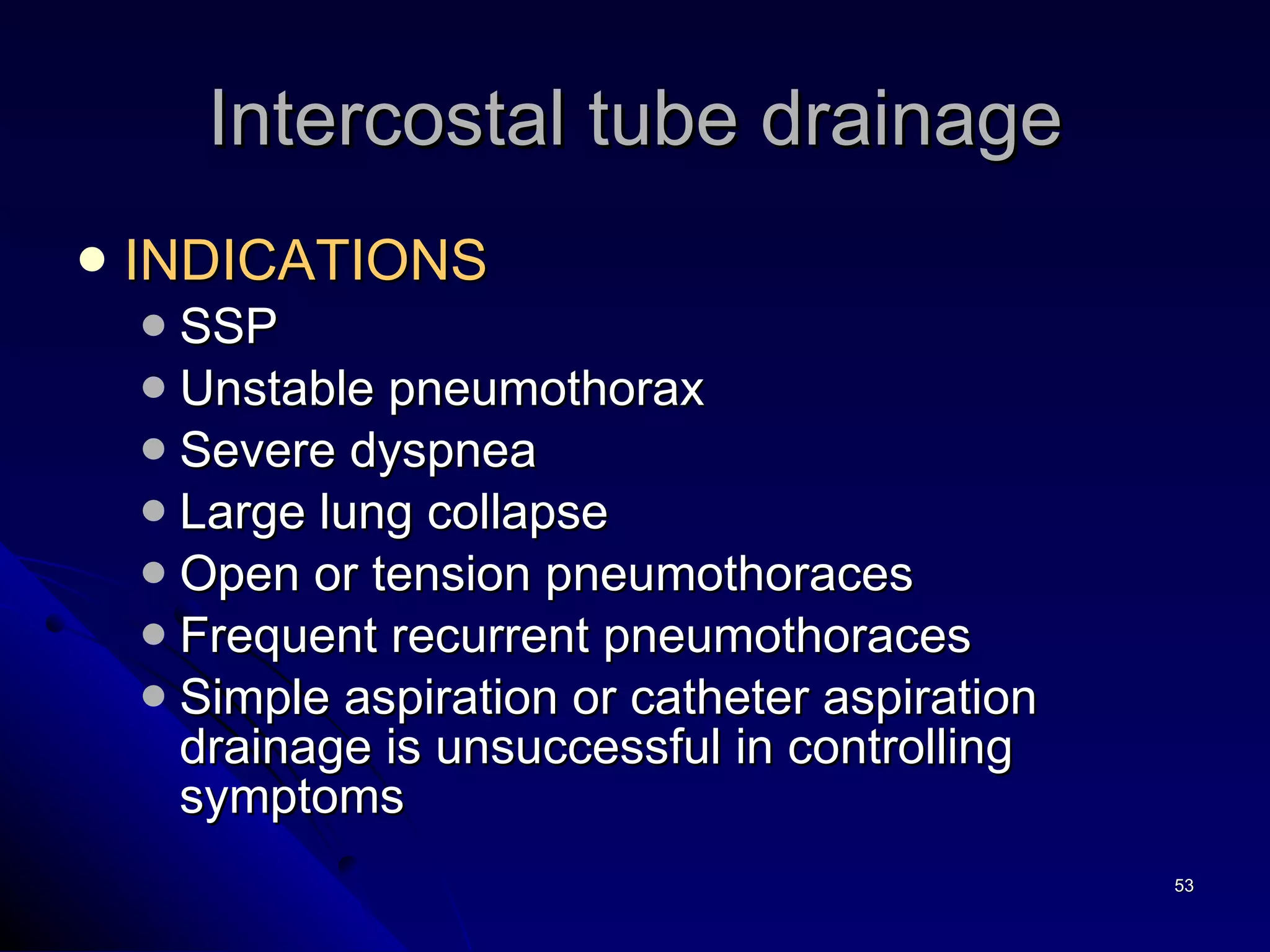
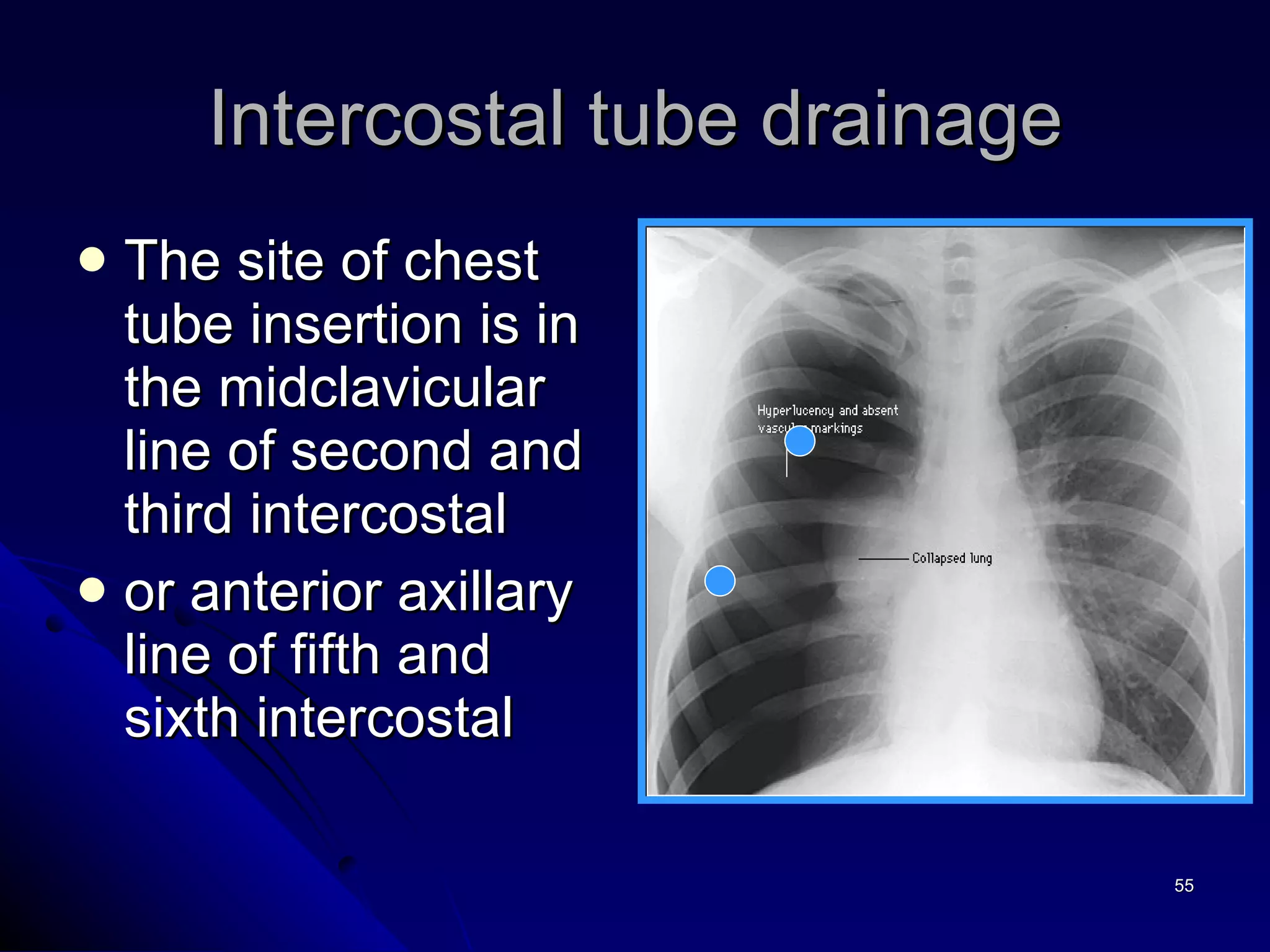
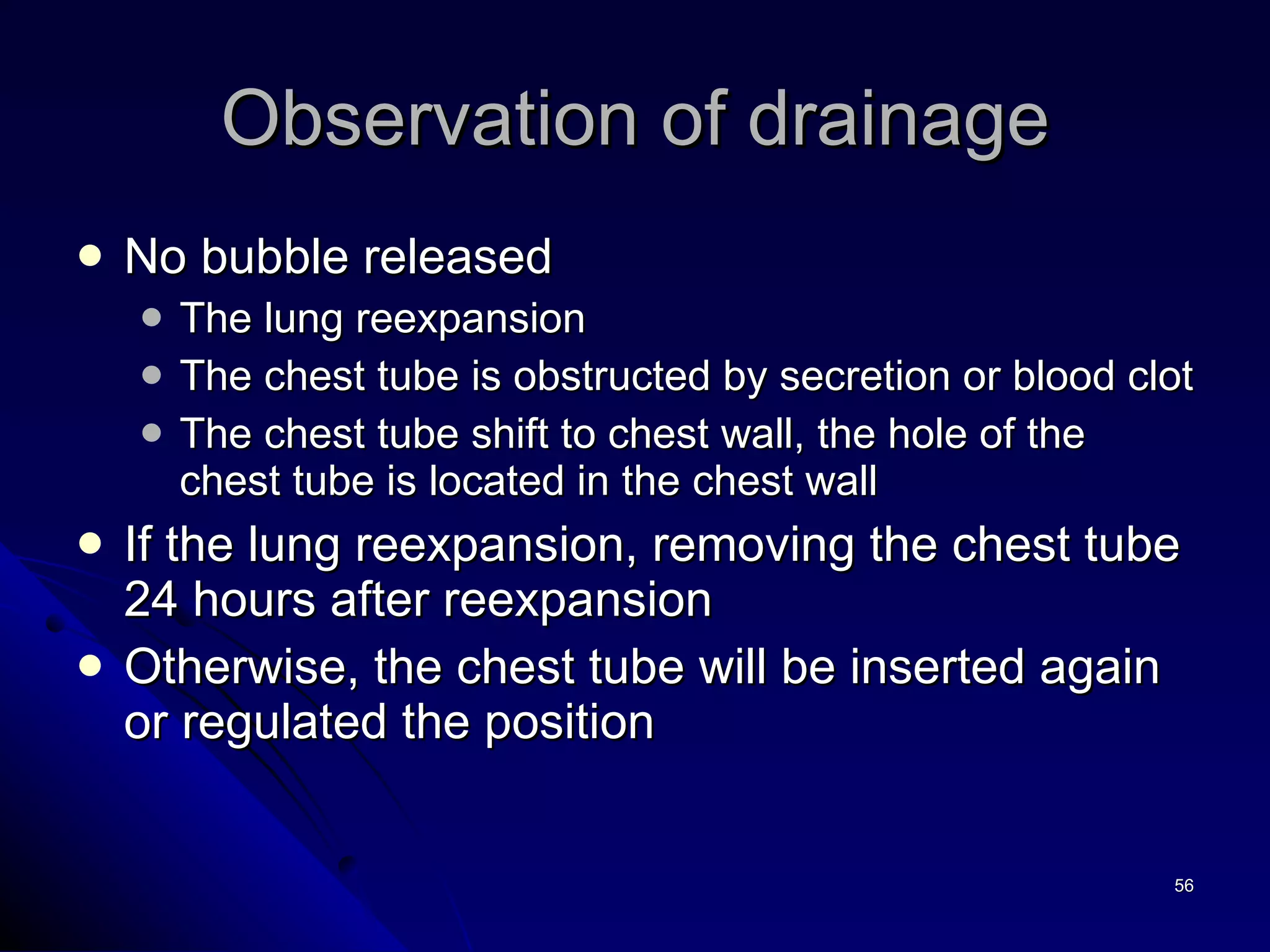
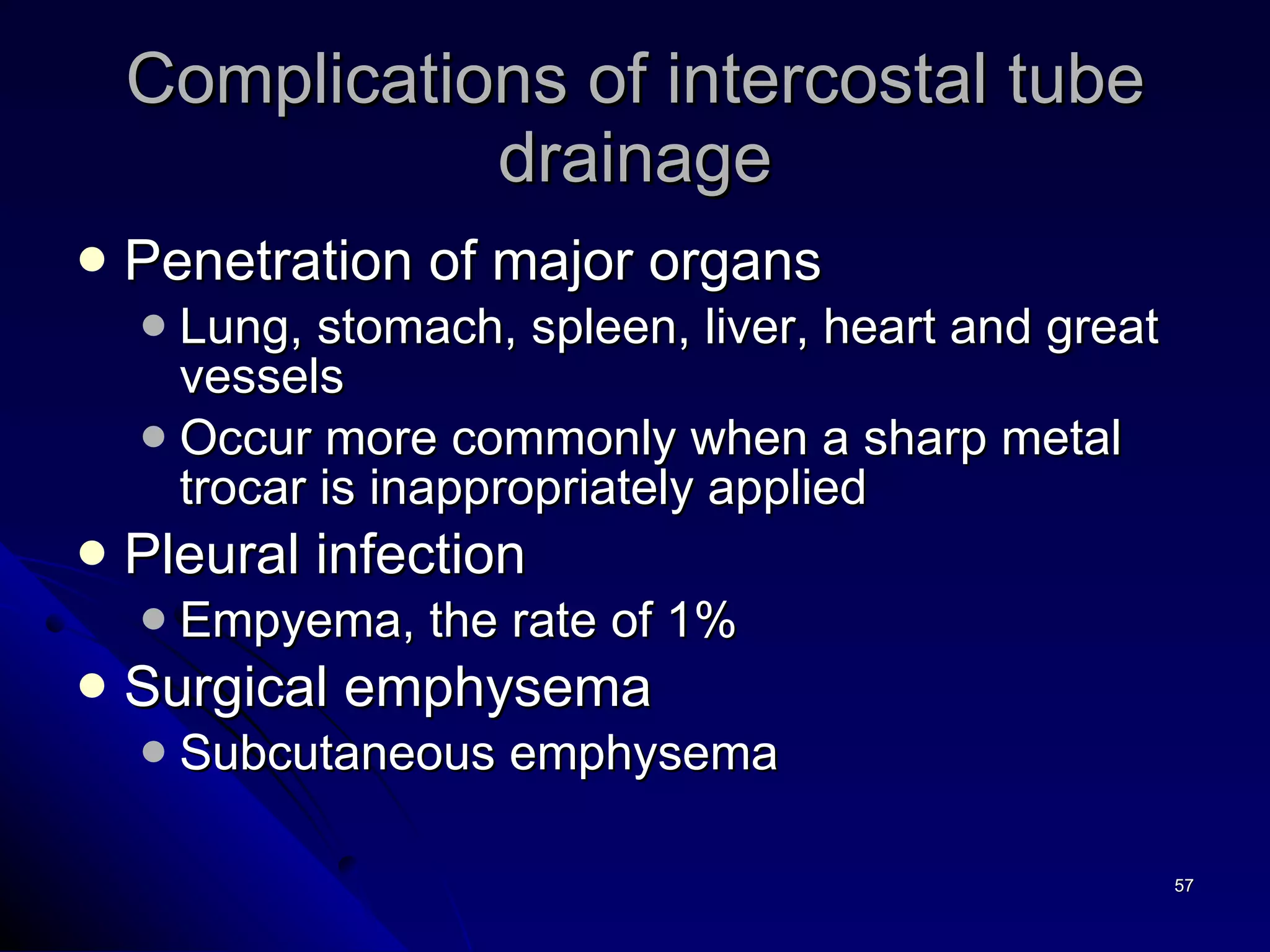
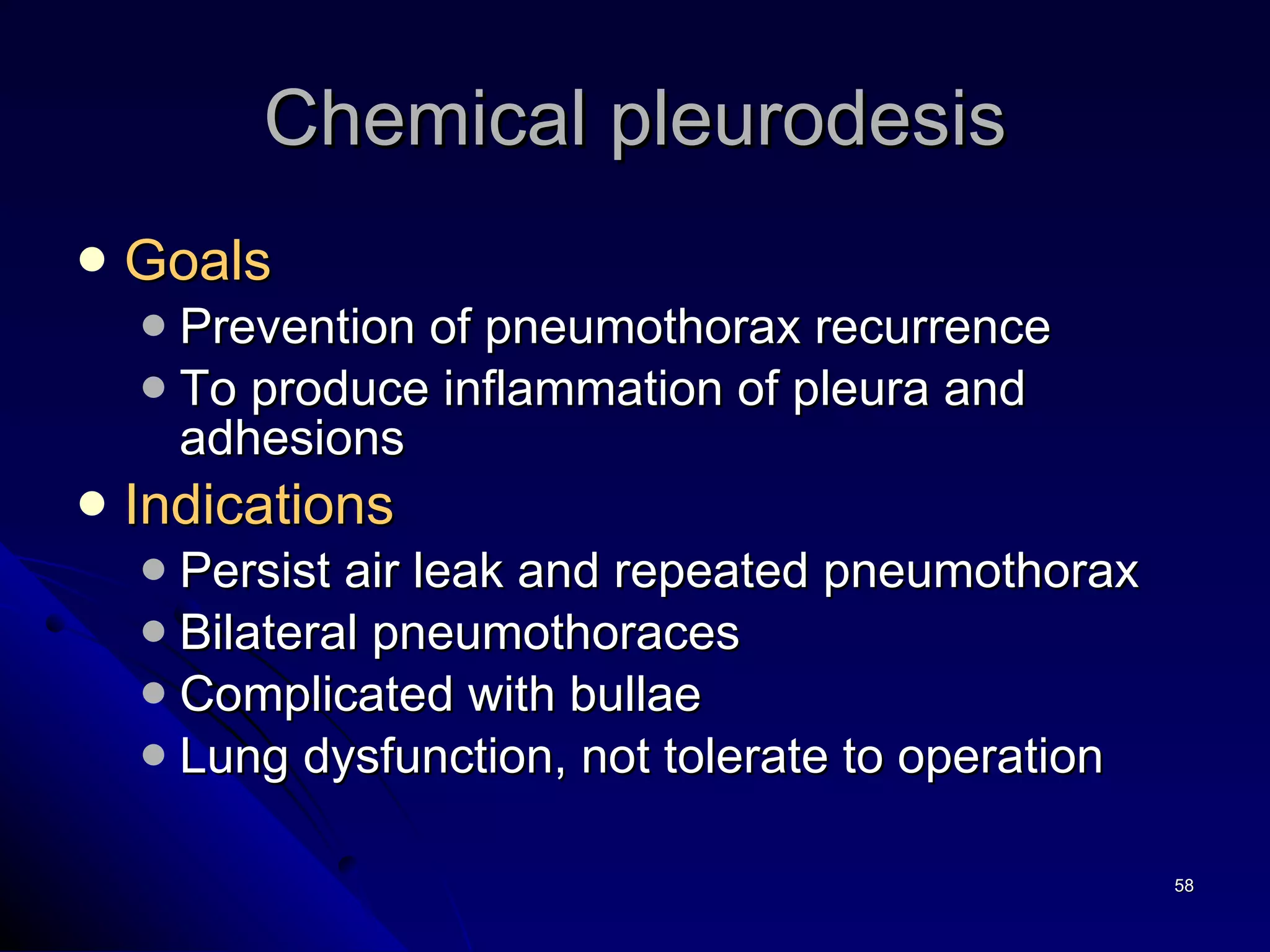
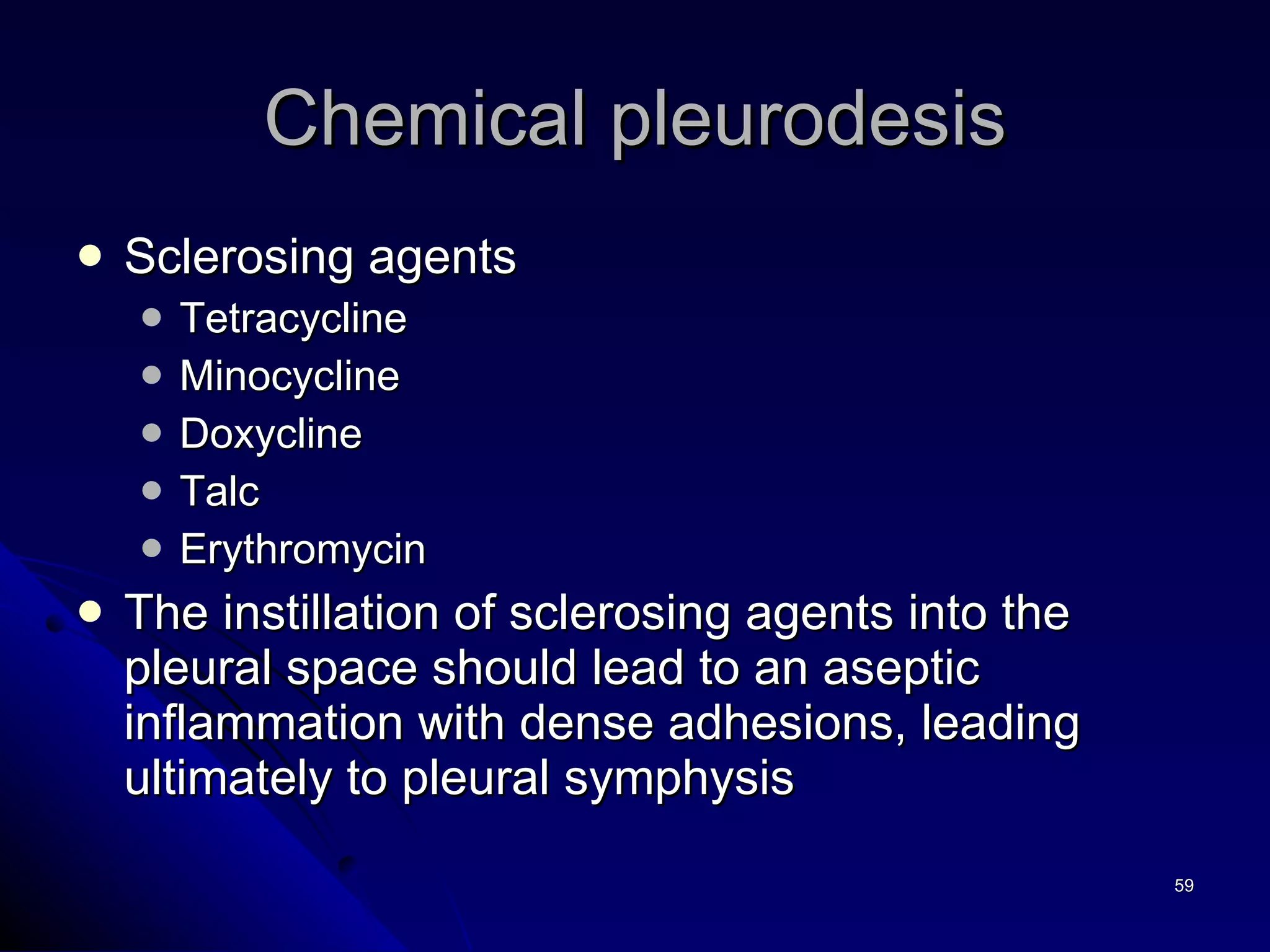
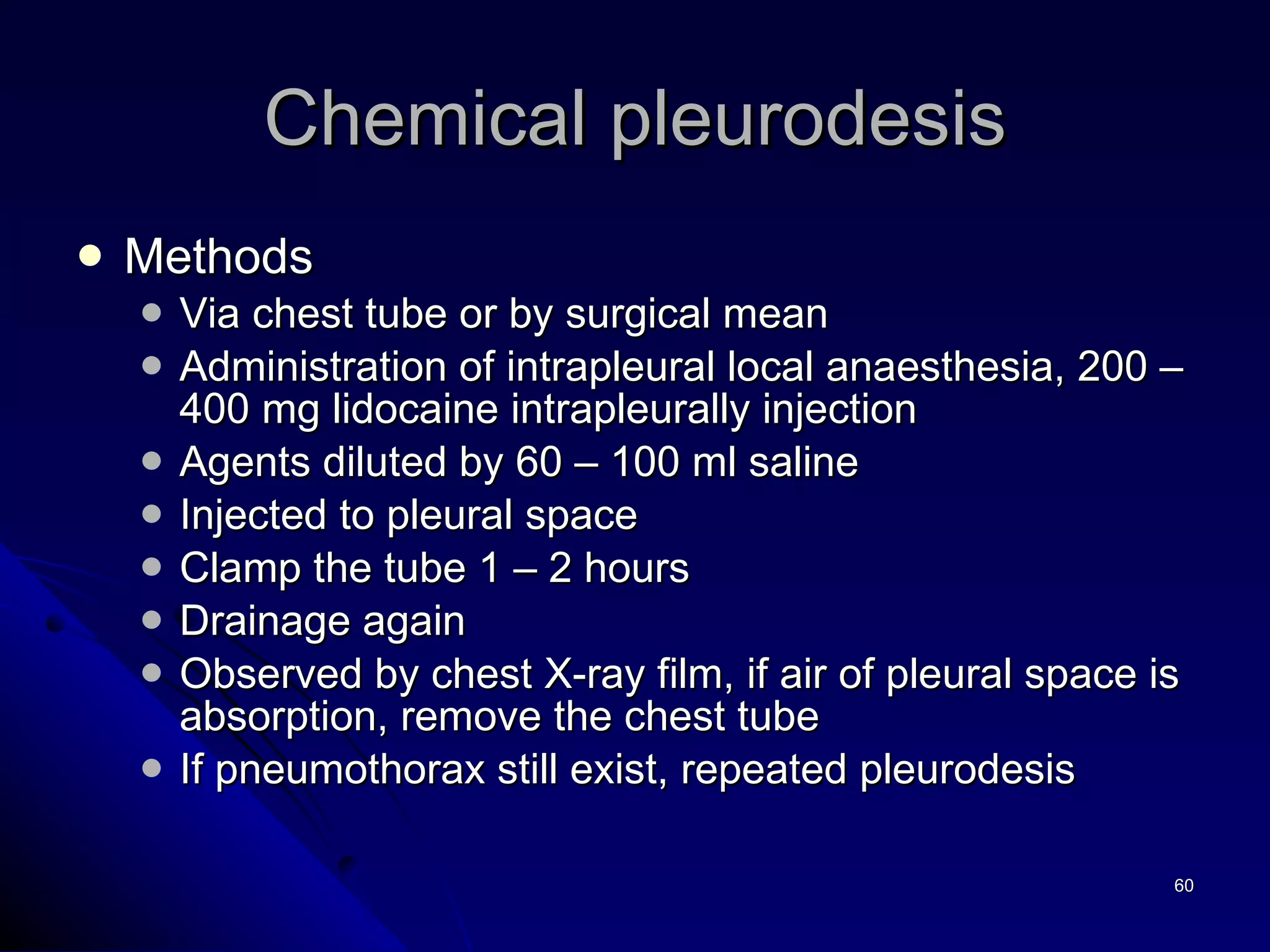
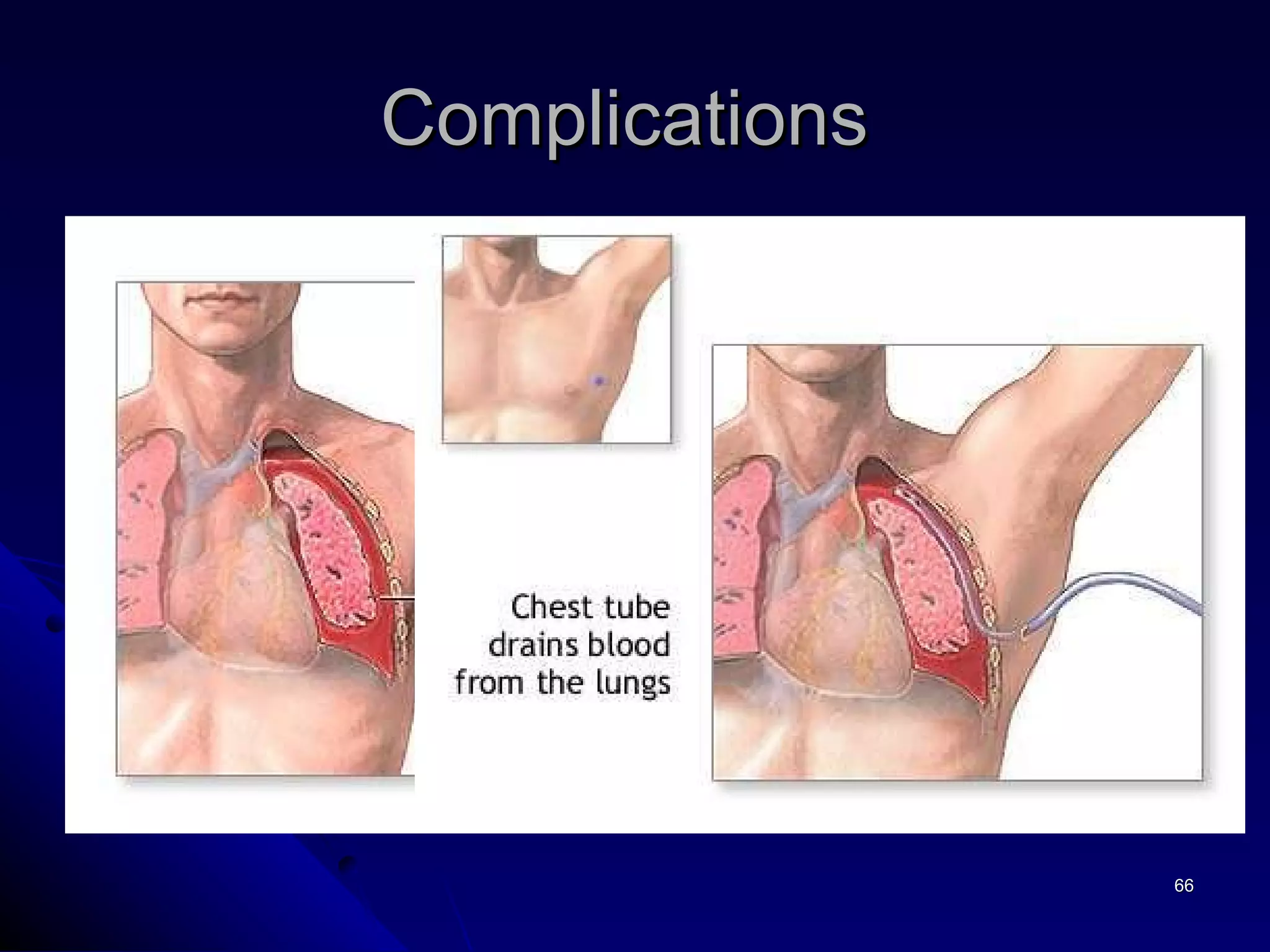
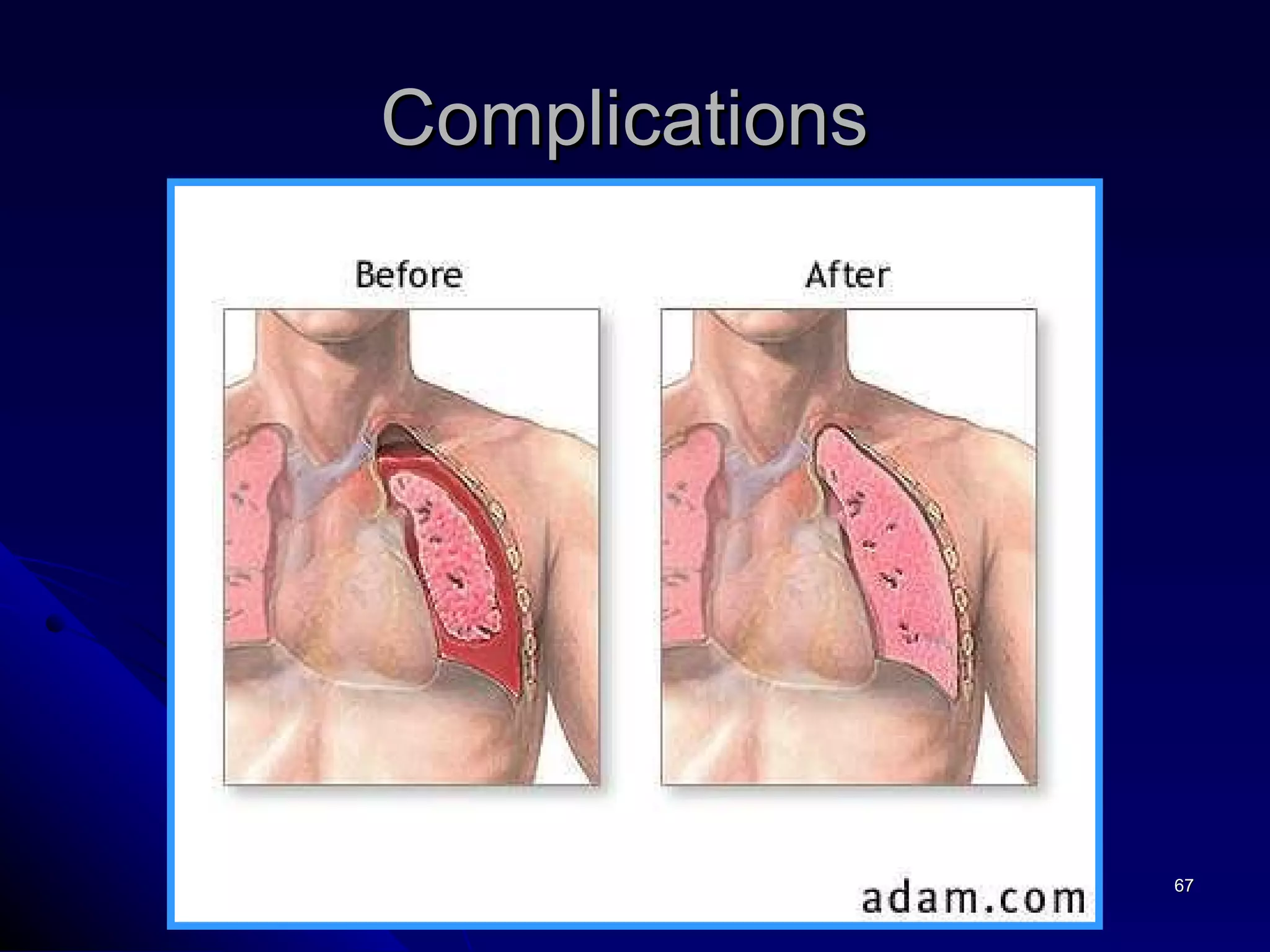
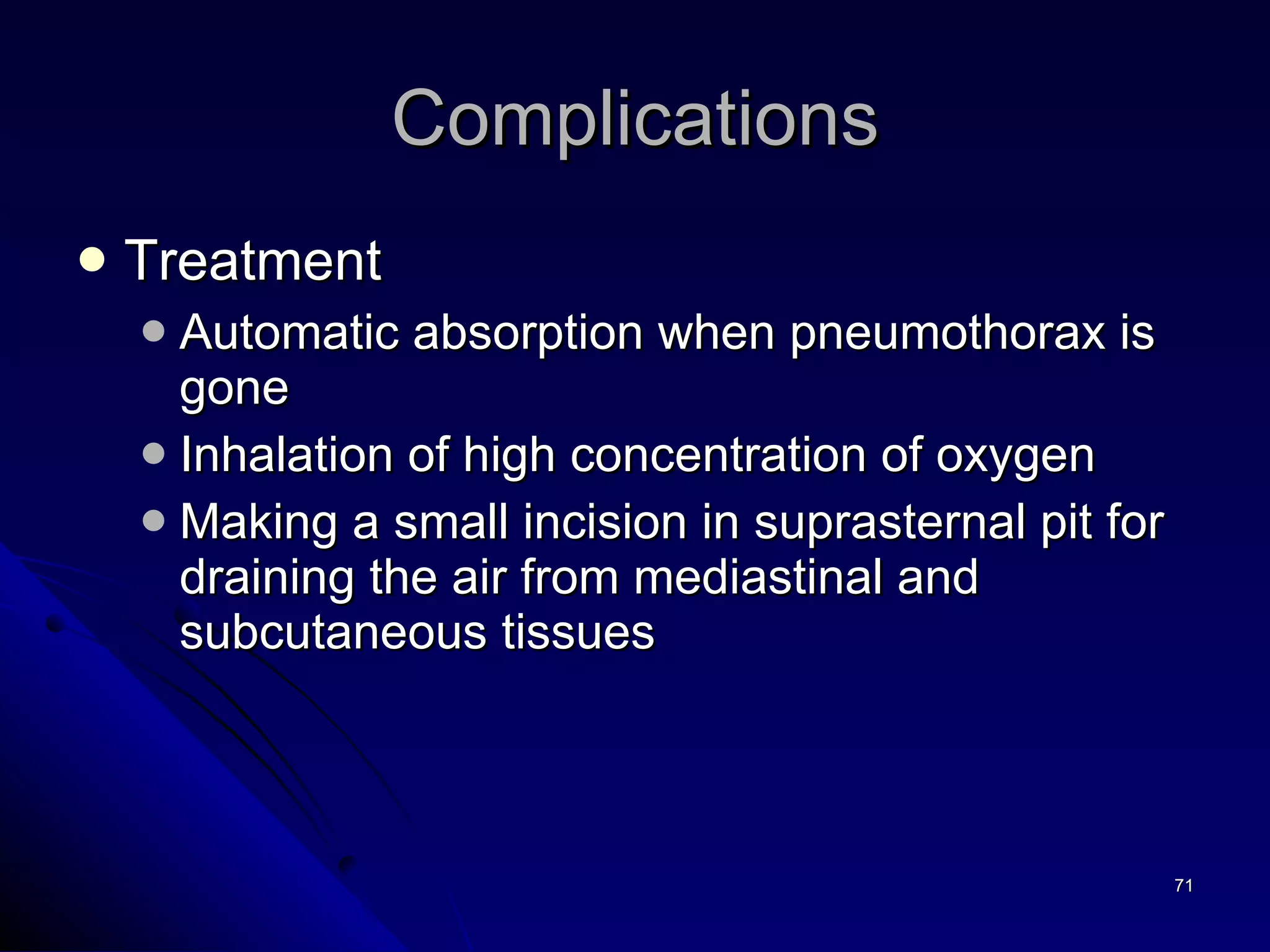
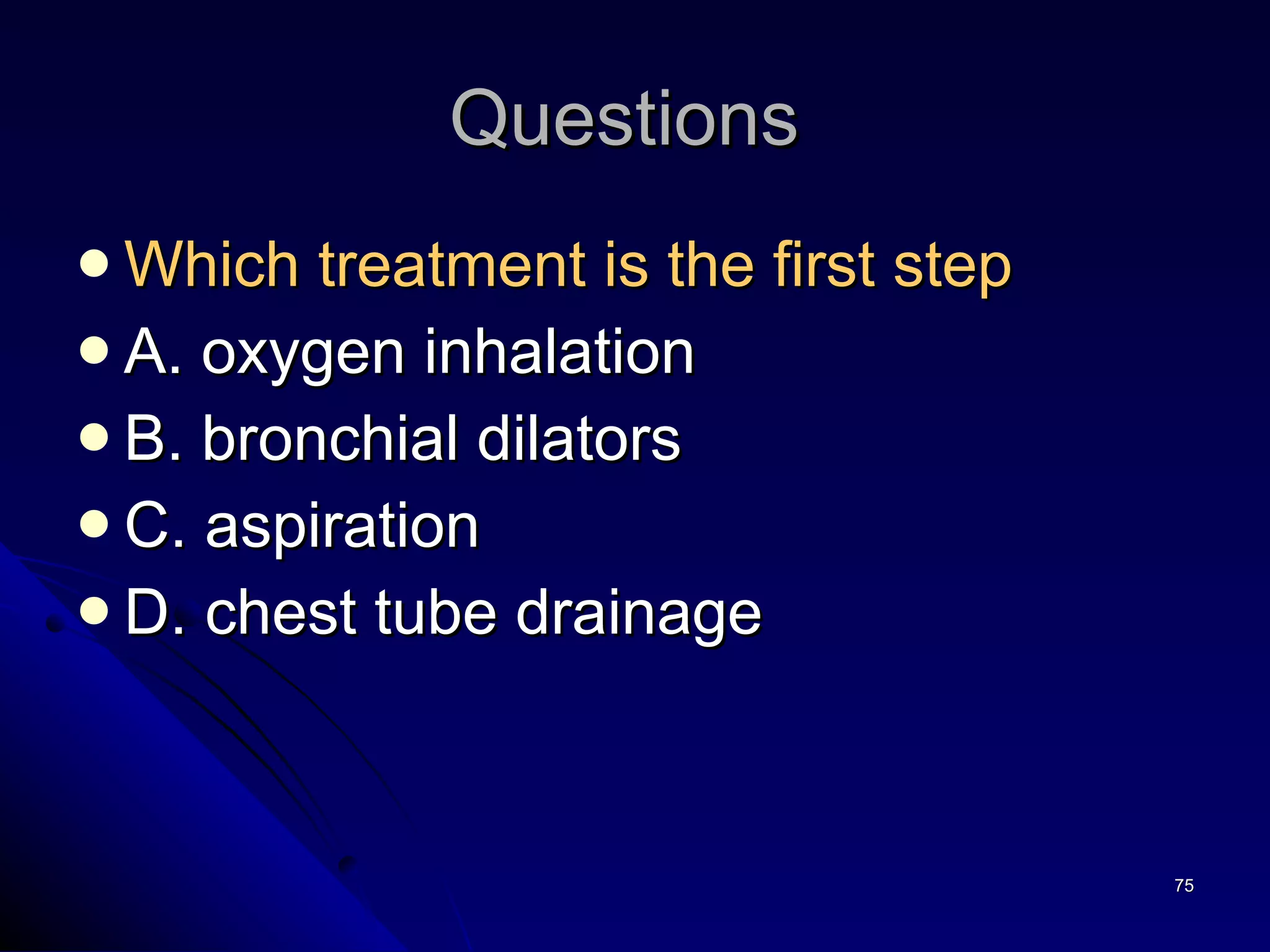
- Treatment involves observation for small primary pneumothoraces or procedures like aspiration, chest tube placement, or surgery depending on the size and symptoms.