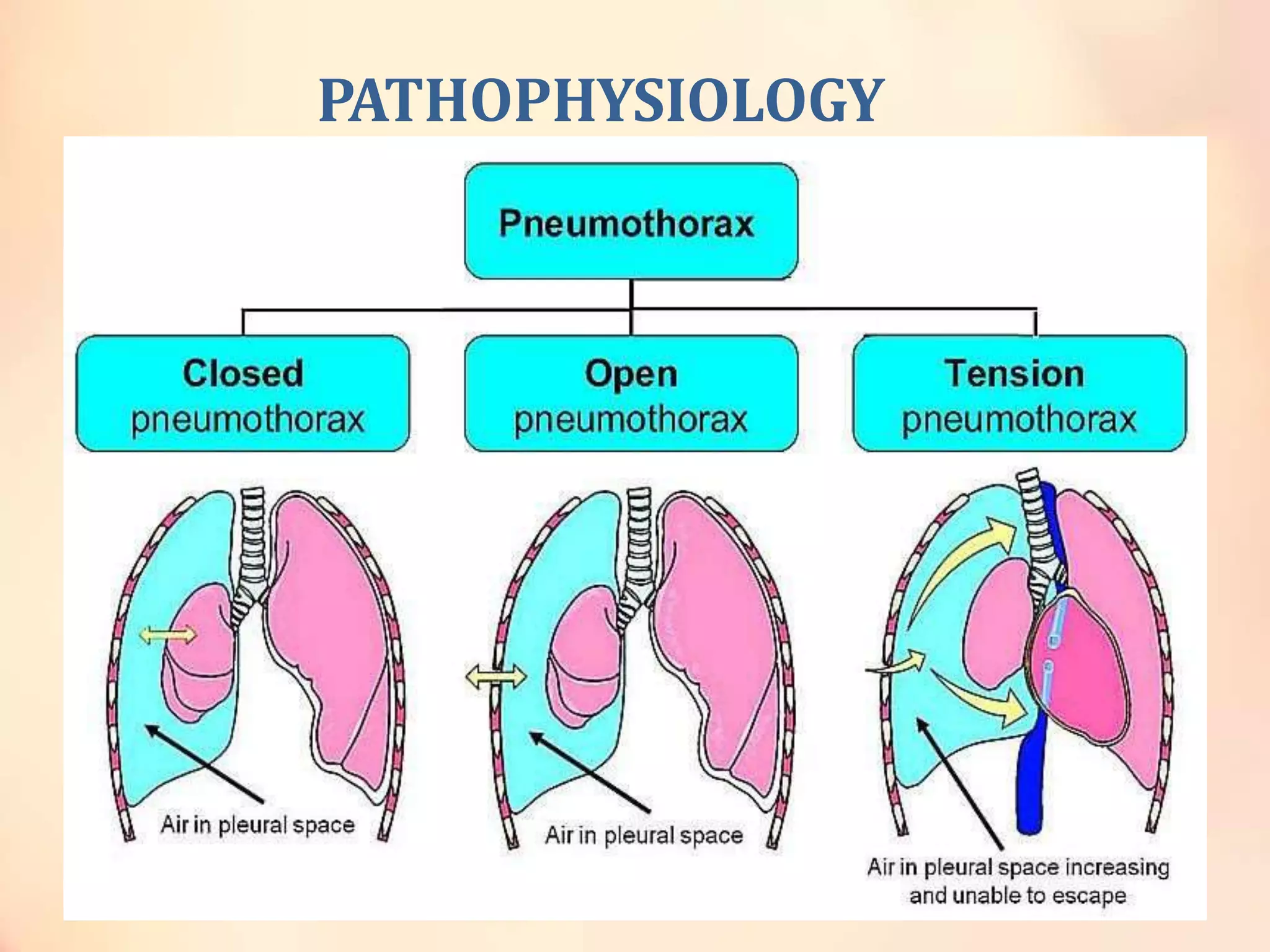
Pneumothorax is the presence of air in the pleural space causing lung collapse. The document defines and classifies pneumothorax, describing the pathophysiology, clinical features, diagnosis and management strategies for primary spontaneous pneumothorax and secondary spontaneous pneumothorax, including tube thoracostomy and pleurodesis. Special types of pneumothorax seen in conditions like AIDS, cystic fibrosis and tuberculosis are also discussed.