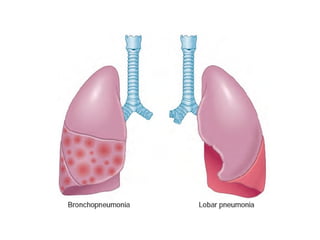
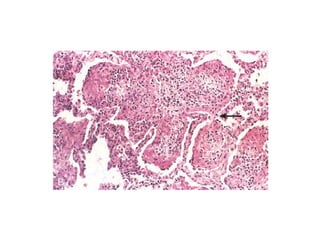
This document provides an overview of different types of pneumonia, including classifications, typical causative organisms, and key characteristics. Community-acquired pneumonias are most commonly caused by bacteria such as Streptococcus pneumoniae, while hospital-acquired pneumonias often involve drug-resistant organisms. Viral pneumonias tend to involve the interstitium rather than alveoli. Immunocompromised individuals are at risk for opportunistic fungal and viral pathogens. Granulomatous pneumonias like tuberculosis can appear chronic.











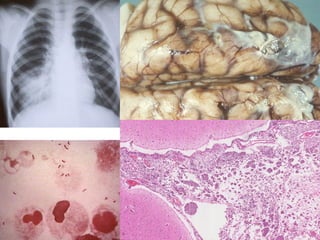




































![COMPROMISED HOSTS
• Defenses are suppressed by
– Disease
– Immunosuppressive therapy for organ or
hematopoietic stem cell transplants
– Chemotherapy for tumors
– Irradiation.
• Infectious agents
– Bacteria (P. aeruginosa, Mycobacterium species, L.
pneumophila, and Listeria monocytogenes),
– Viruses (cytomegalovirus [CMV] and herpesvirus)
– Fungi (P. jiroveci, Candida species, Aspergillus
species, the Phycomycetes, and Cryptococcus
neoformans).](https://image.slidesharecdn.com/pneumonia-160414054127/85/Pneumonia-51-320.jpg)



