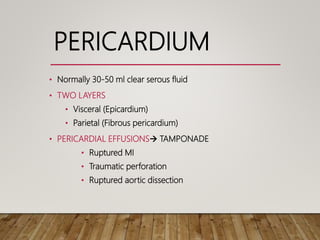
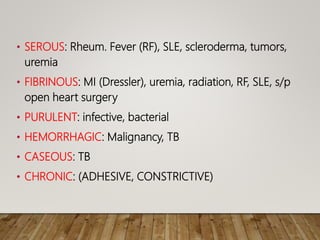
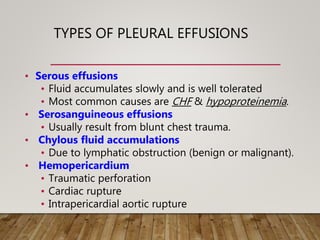
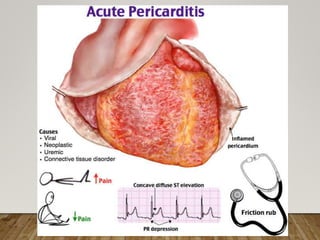
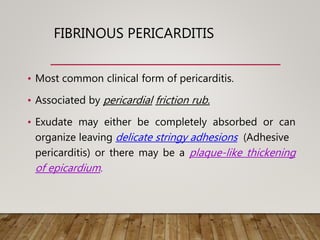
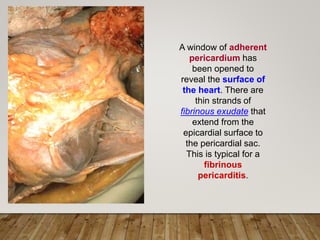
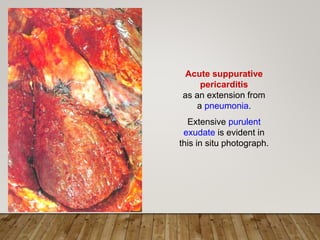
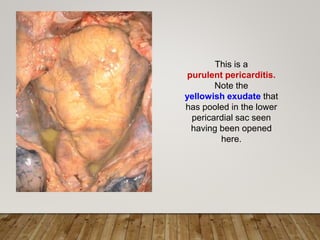
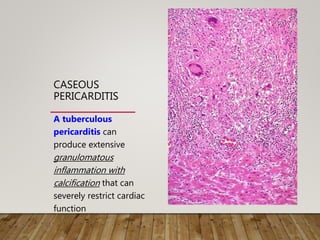
The pericardium normally contains a small amount of fluid to reduce friction on the heart. Pericardial effusions occur when too much fluid accumulates and can cause cardiac tamponade. There are several types of pericardial effusions including serous, fibrinous, purulent, hemorrhagic, and caseous. Serous effusions are most common in congestive heart failure and hypoproteinemia. Fibrinous pericarditis causes pericardial friction rub and can result in adhesions or thickening. Purulent pericarditis from infection contains pus and causes high fever and rigors. Chronic or healed pericarditis can resolve completely or cause fibrosis