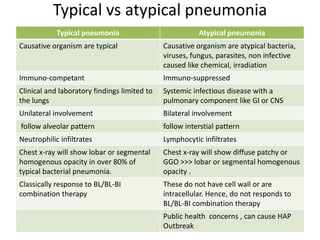
1. Atypical pneumonia is characterized by gradual onset of symptoms associated with an unusual radiographic pattern of infection. It involves both upper and lower respiratory tracts and can have a protracted clinical course.
2. It is caused by atypical bacteria, viruses, or other pathogens. Common causes include Mycoplasma pneumoniae, Legionella pneumophila, and Chlamydophila pneumoniae.
3. Diagnosis involves lab tests like culture, antigen detection by ELISA or PCR from respiratory samples, as well as antibody detection from serum samples. Chest imaging often shows diffuse bilateral opacities rather than lobar consolidation.