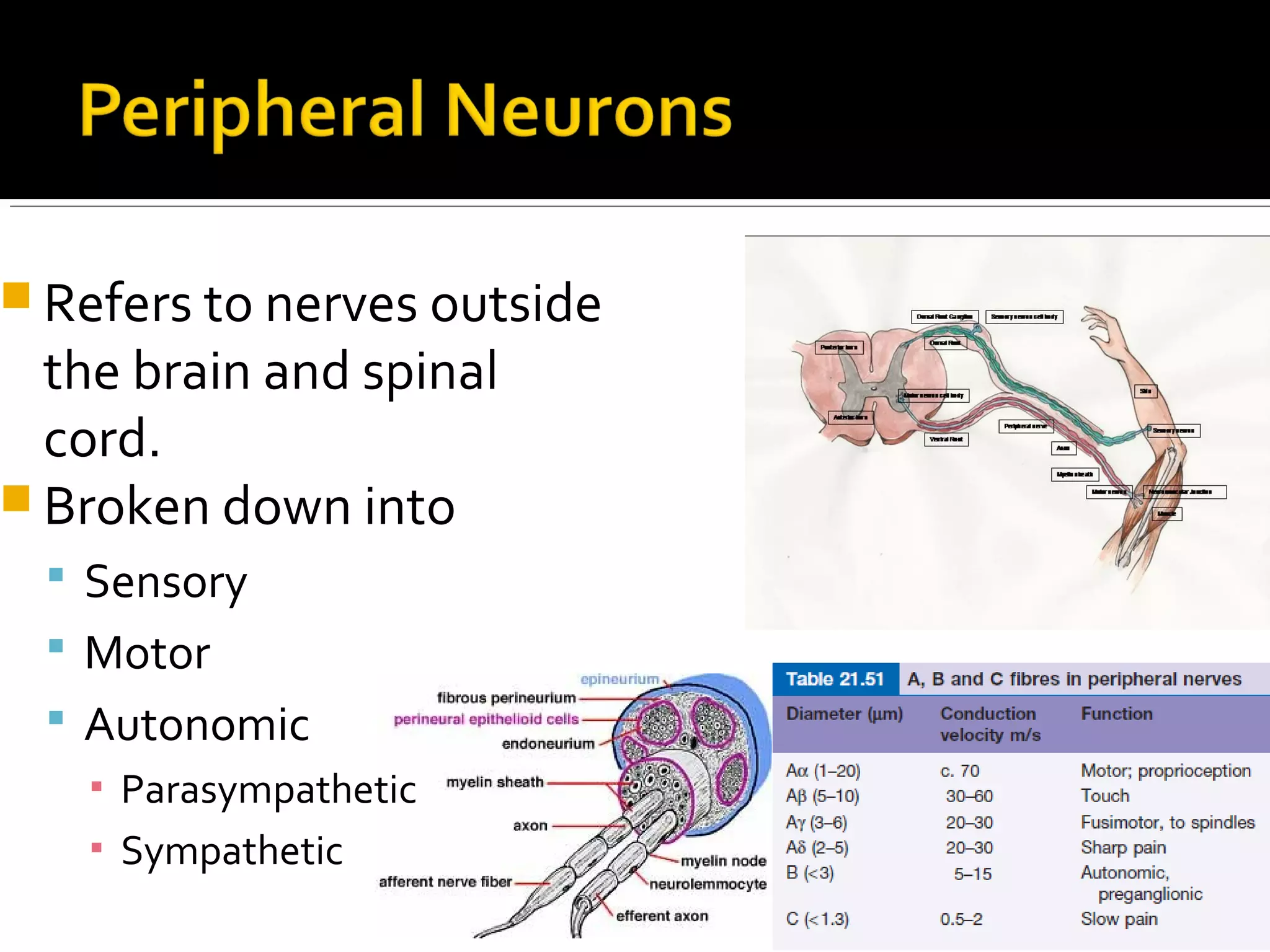
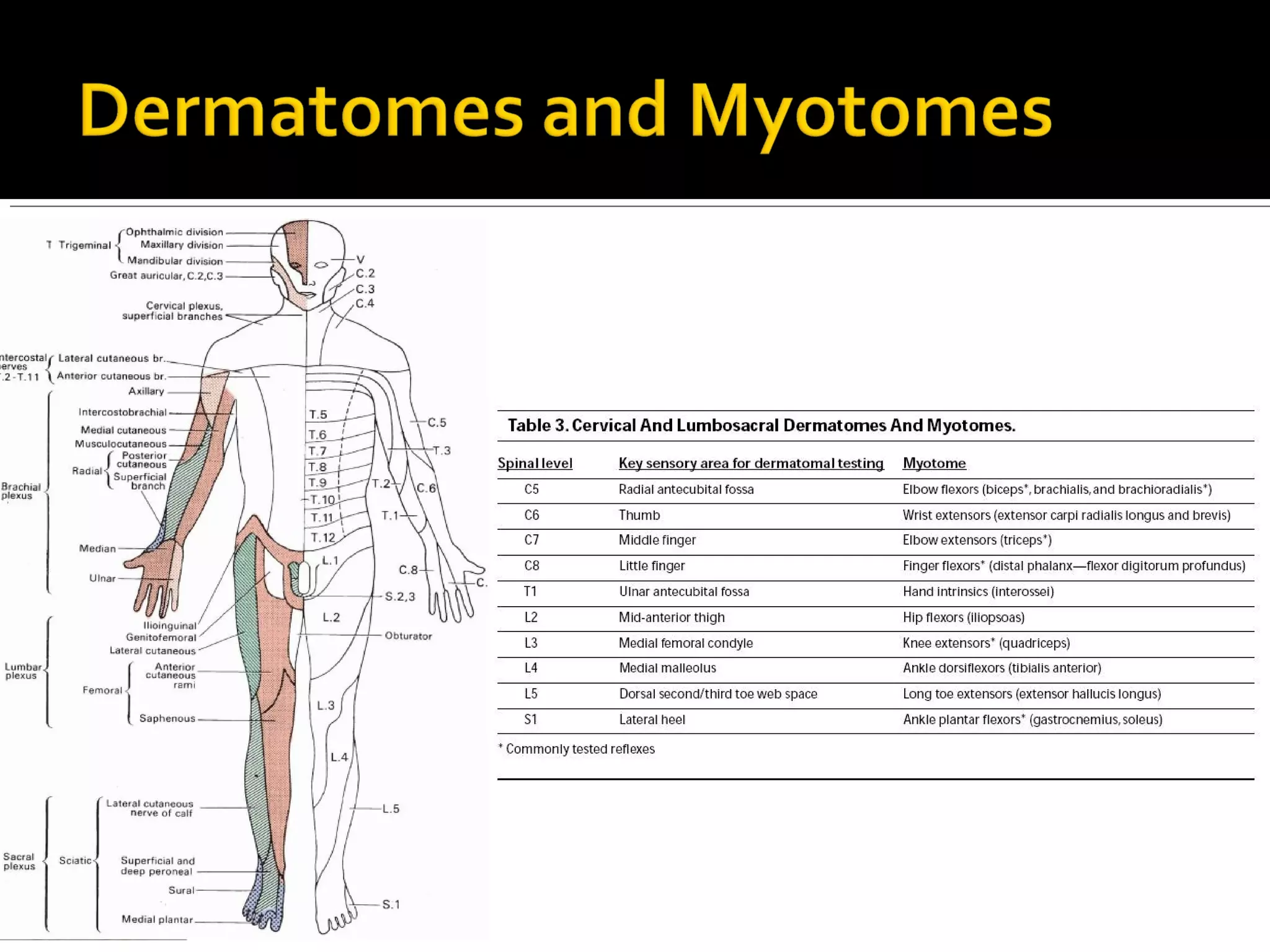
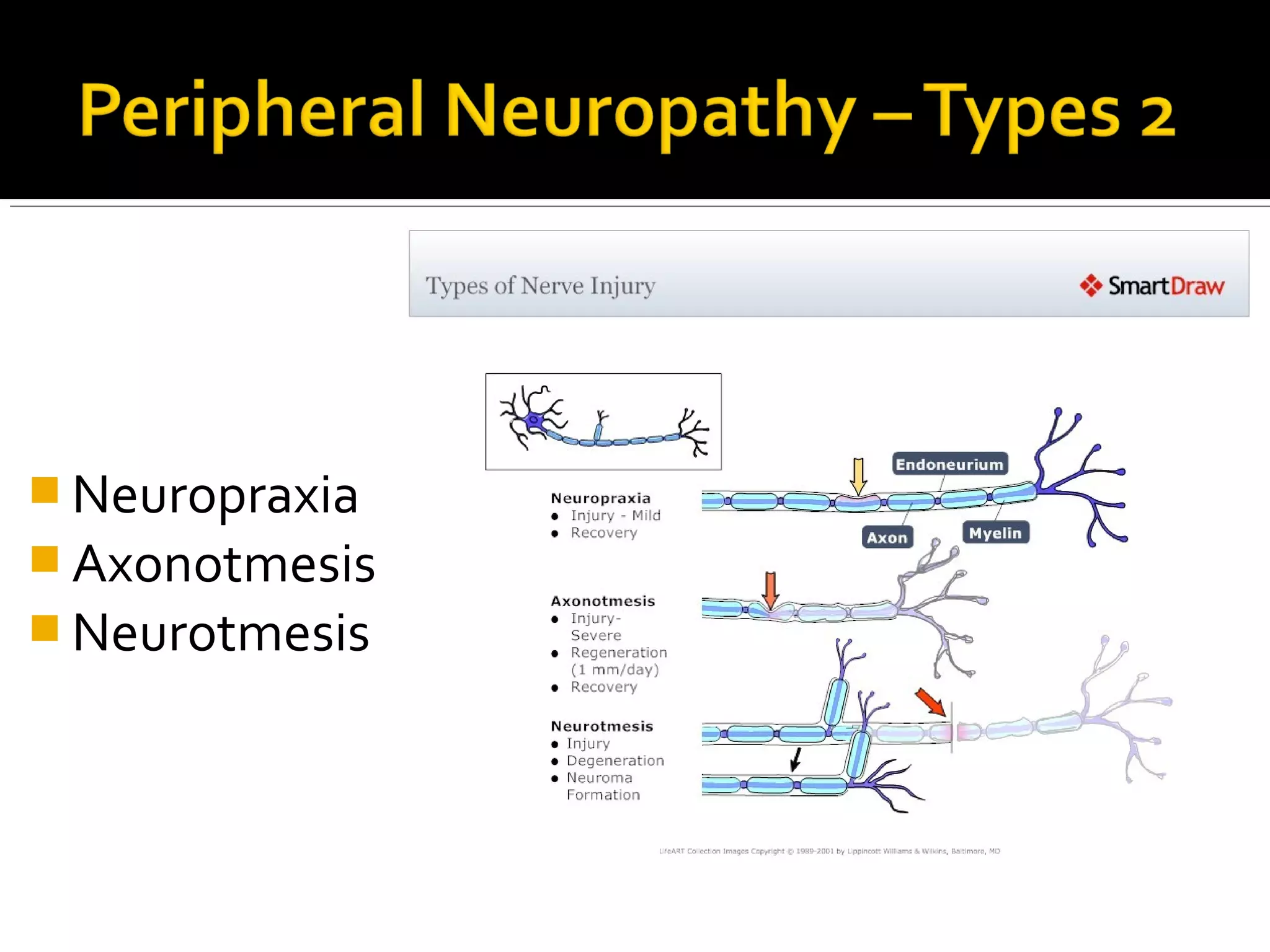
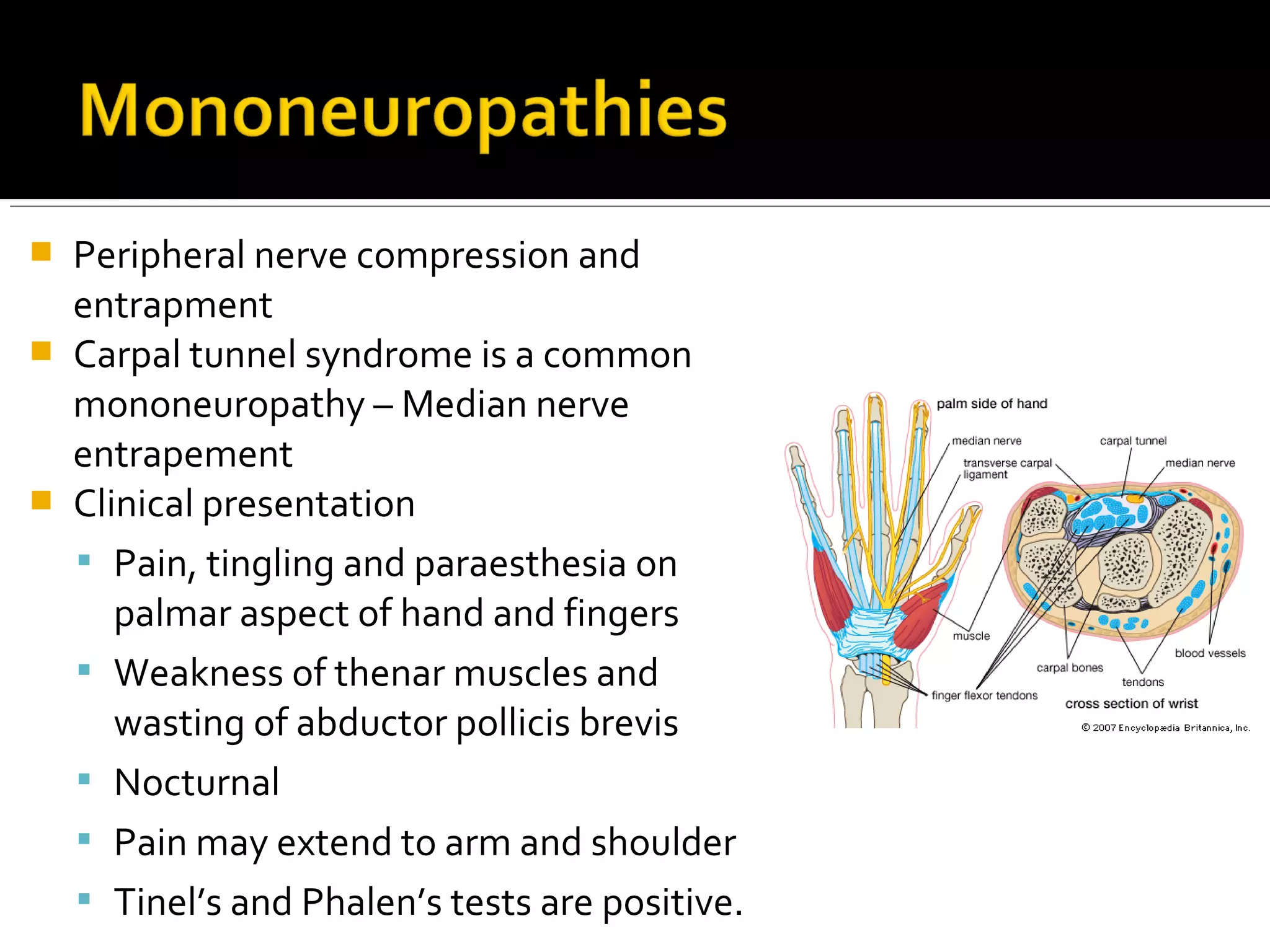
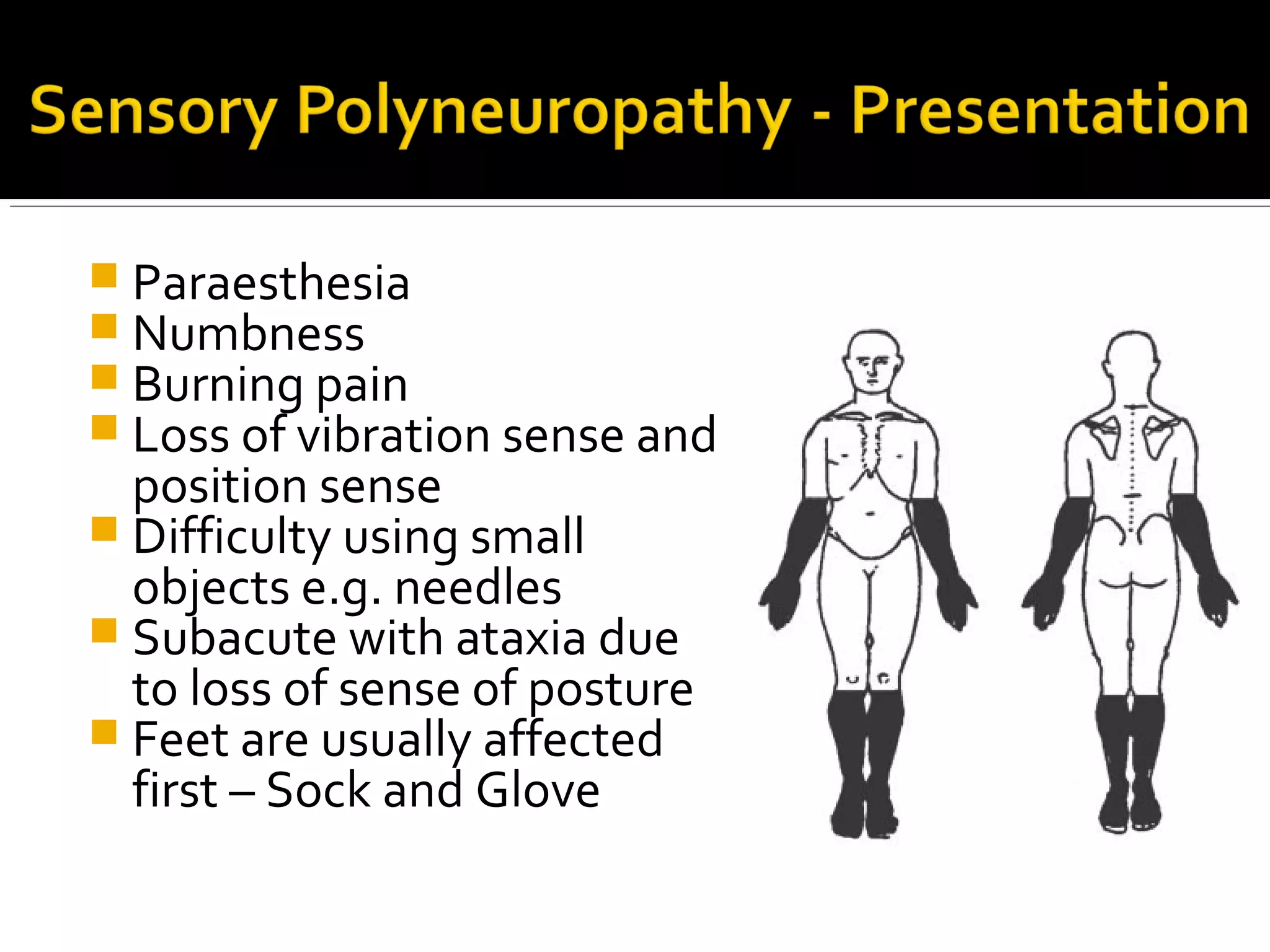
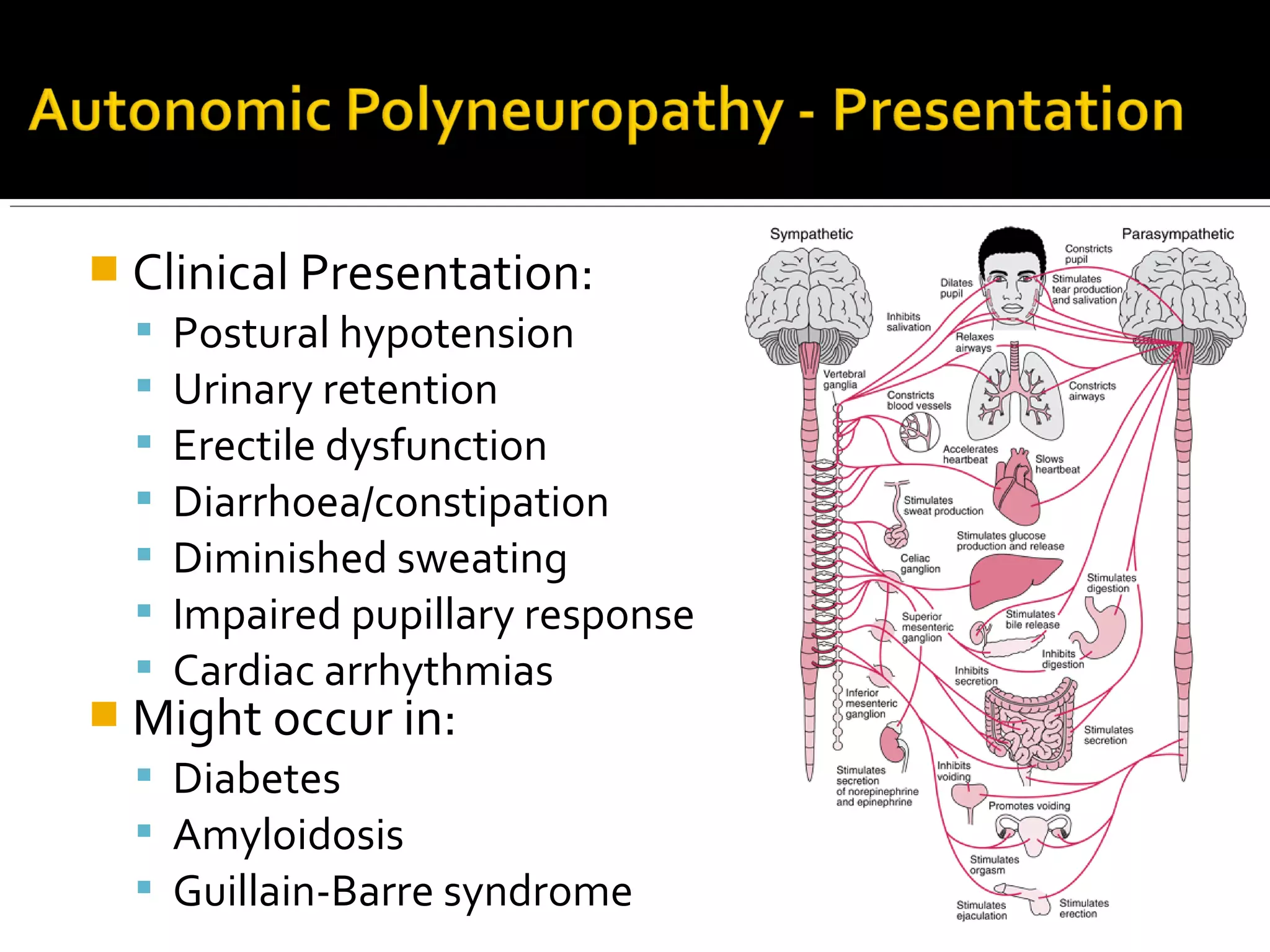
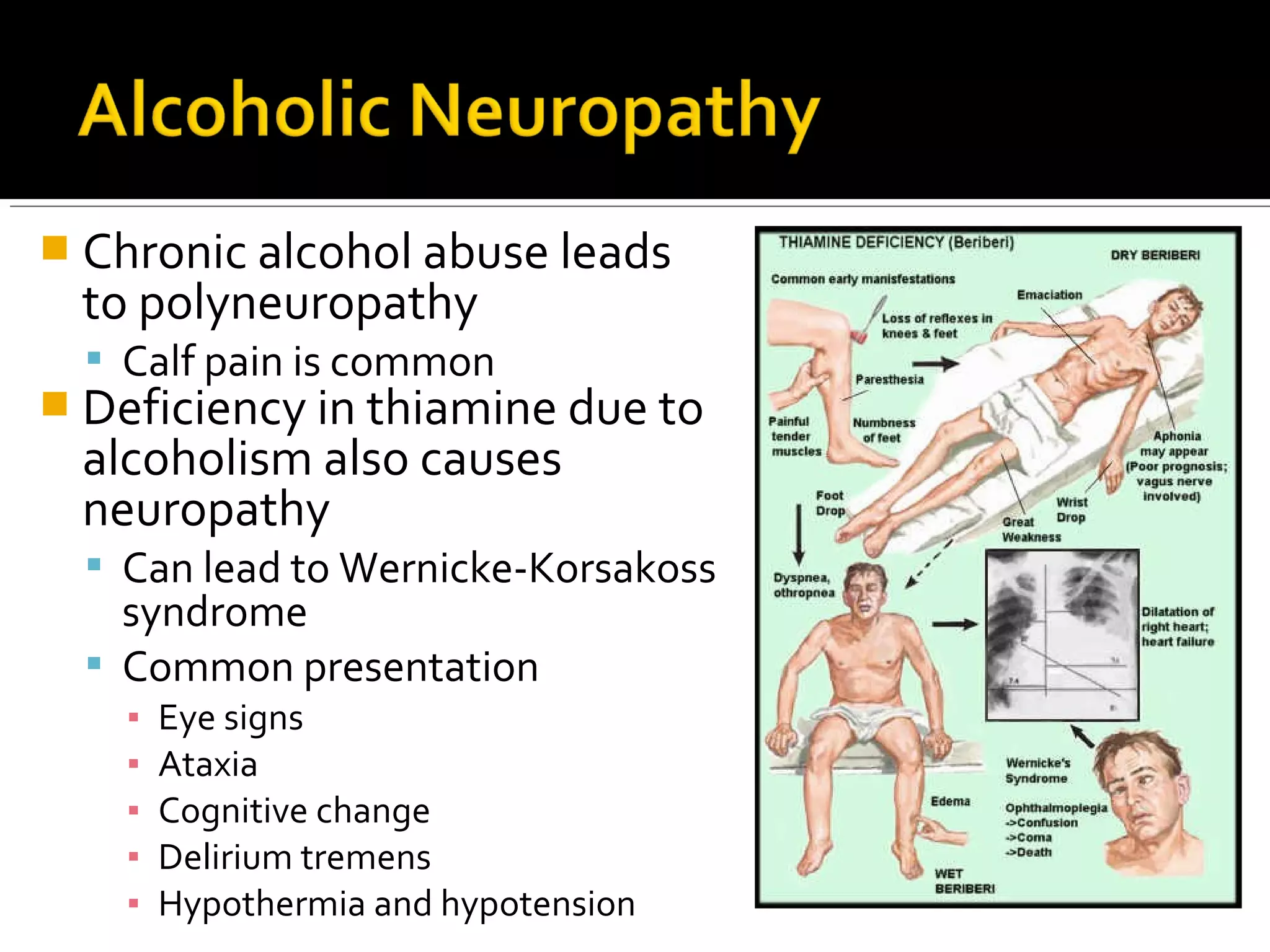
This document discusses peripheral neuropathy, which refers to diseases that affect nerves outside the brain and spinal cord. It covers the types of peripheral nerves and classifications of neuropathies. Some key causes of peripheral neuropathy discussed include diabetes, nutritional deficiencies like B1/B12 deficiency, alcoholism, infections like HIV and leprosy, and certain drugs. Symptoms, clinical presentations, investigations, and treatment approaches for different types of peripheral neuropathies are also summarized.