This document discusses peripheral neuropathy, including:
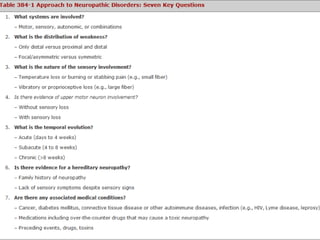
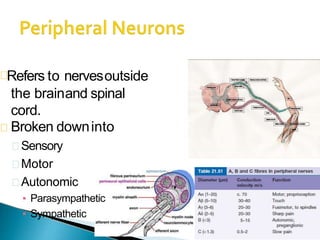
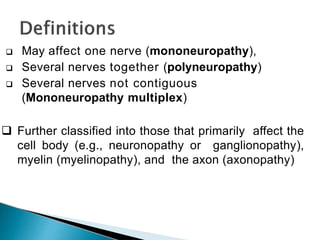
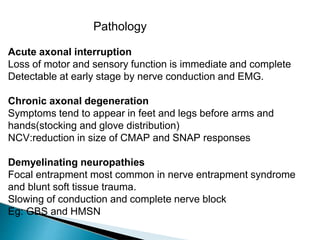
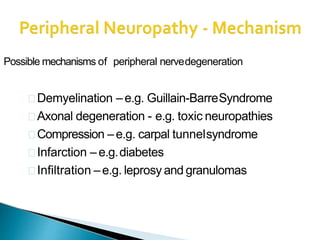
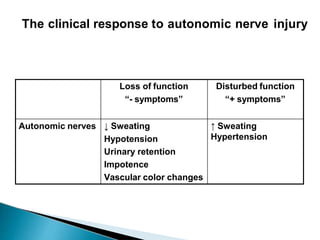
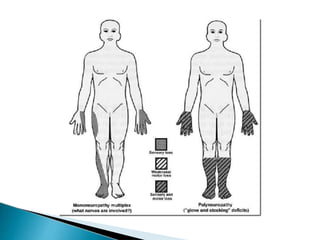
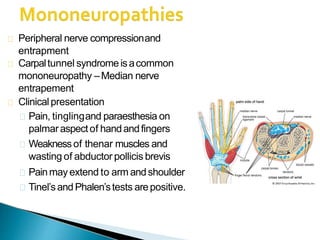
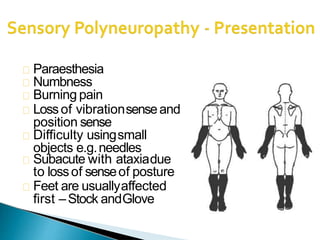
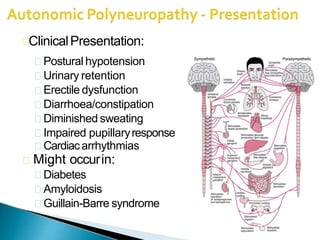
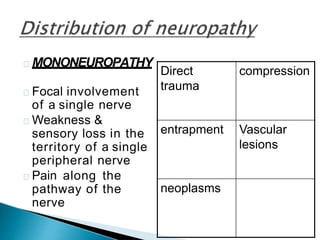
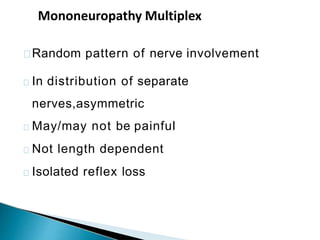
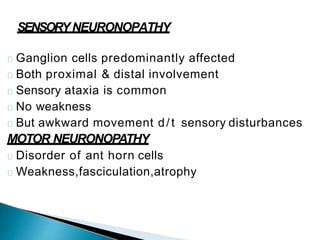
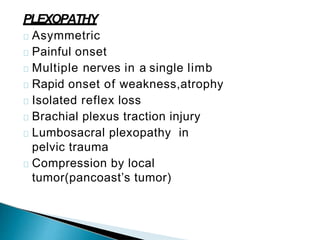
1. It defines peripheral neuropathy and describes the different types that can affect motor, sensory, or autonomic nerves.
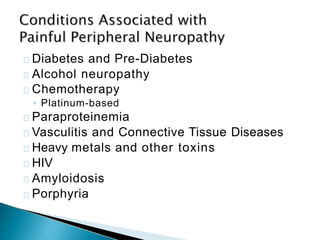
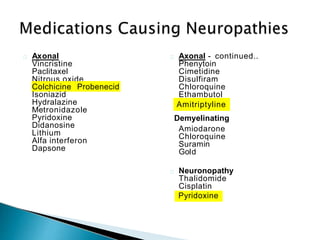
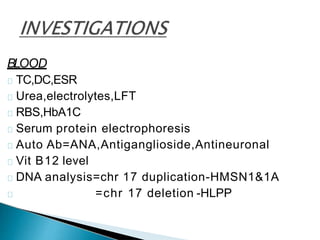
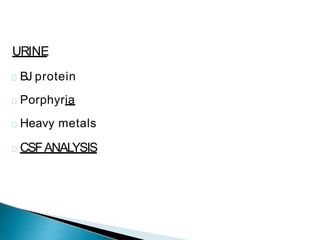
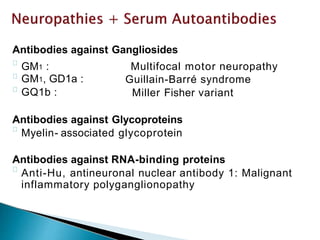
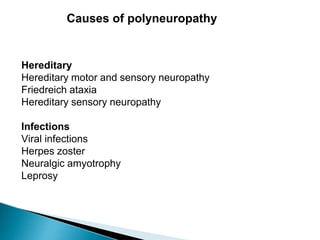
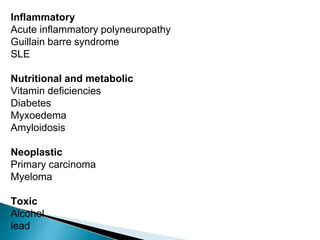
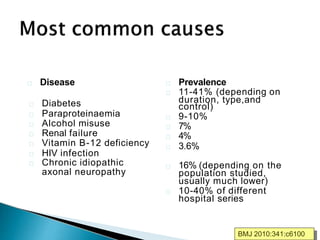
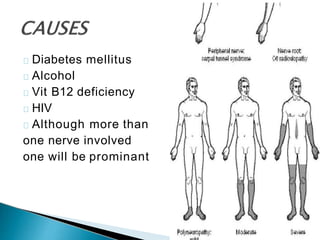
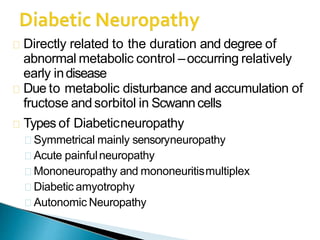
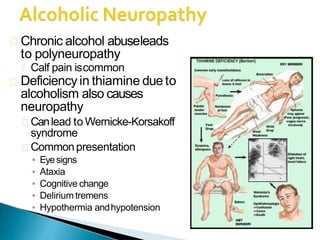
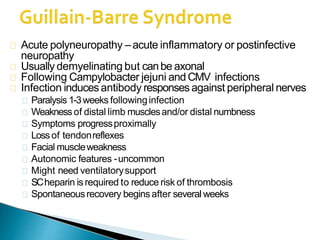
2. It outlines various causes of peripheral neuropathies including hereditary, infectious, inflammatory, metabolic, toxic, and more.
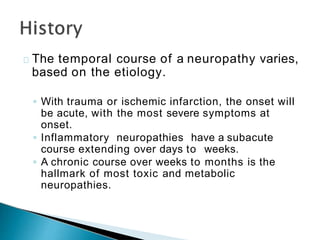
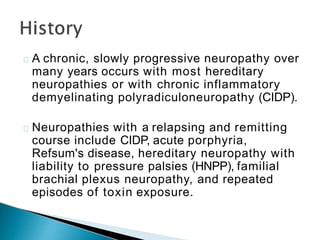
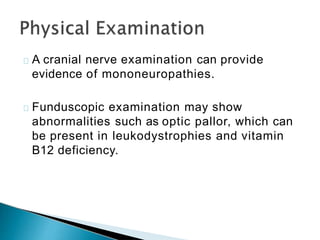
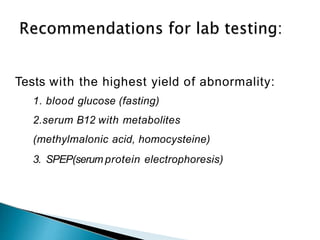
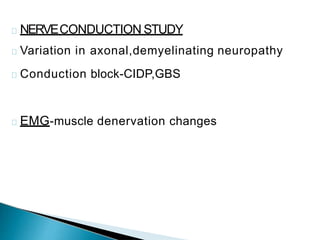
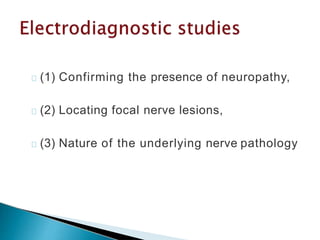
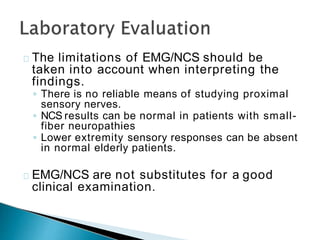
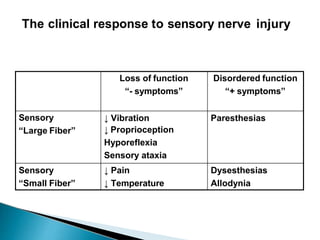
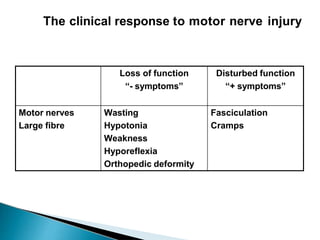
3. It describes the clinical presentations of different types of peripheral neuropathies based on the affected nerves and provides examples.
![DM
hypothyroidism
chronic renal failure
liver disease
intestinal
malabsorption
malignancy
connective tissue
diseases
[HIV]
drug use
Vitamin B6 toxicity
alcohol and dietary
habits
• Weight loss, malaise, and anorexia.](https://image.slidesharecdn.com/peripheralneuropathy-210206174907/85/Peripheral-neuropathy-29-320.jpg)