This document provides an overview of peripheral neuropathy including:
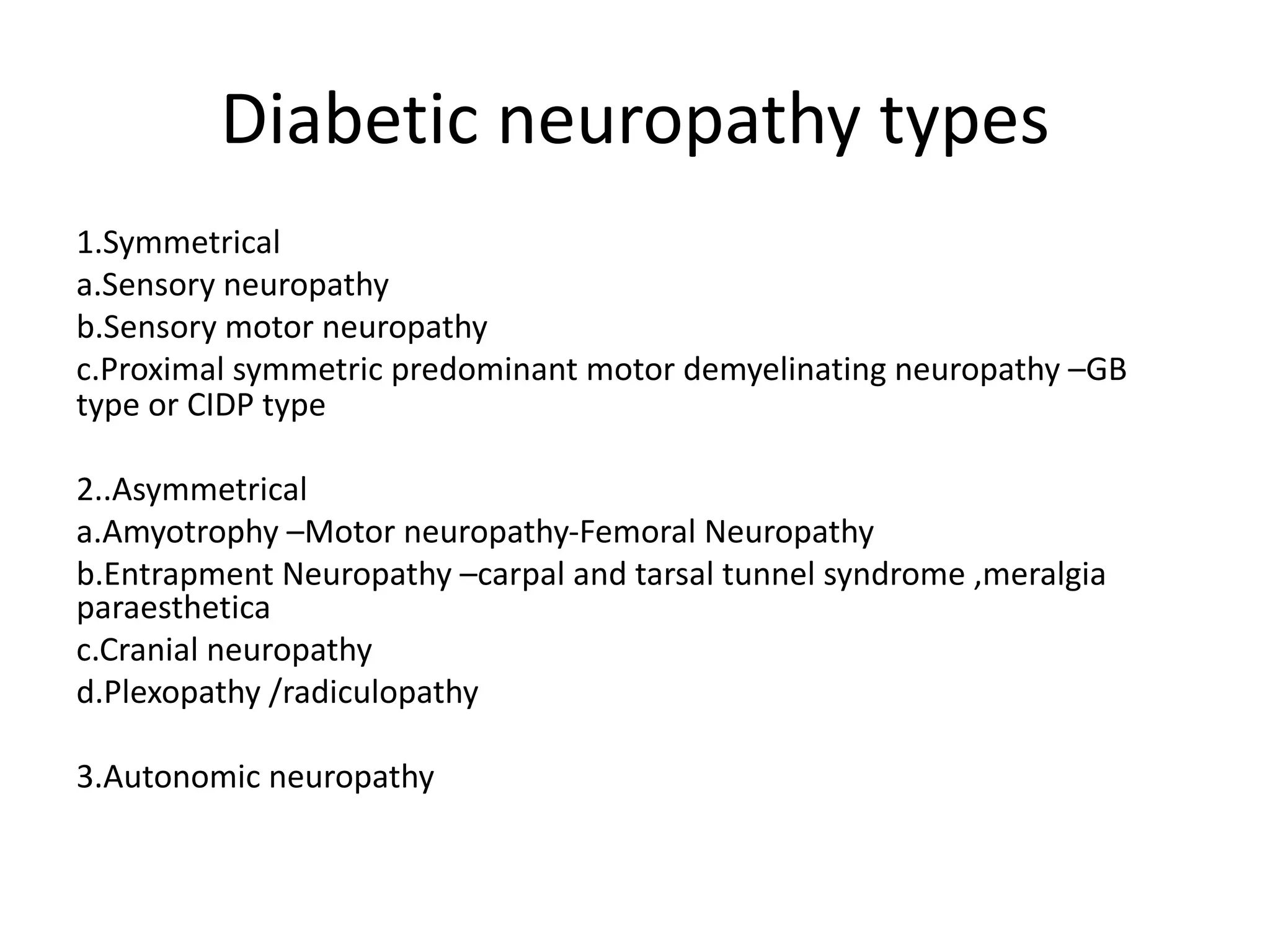
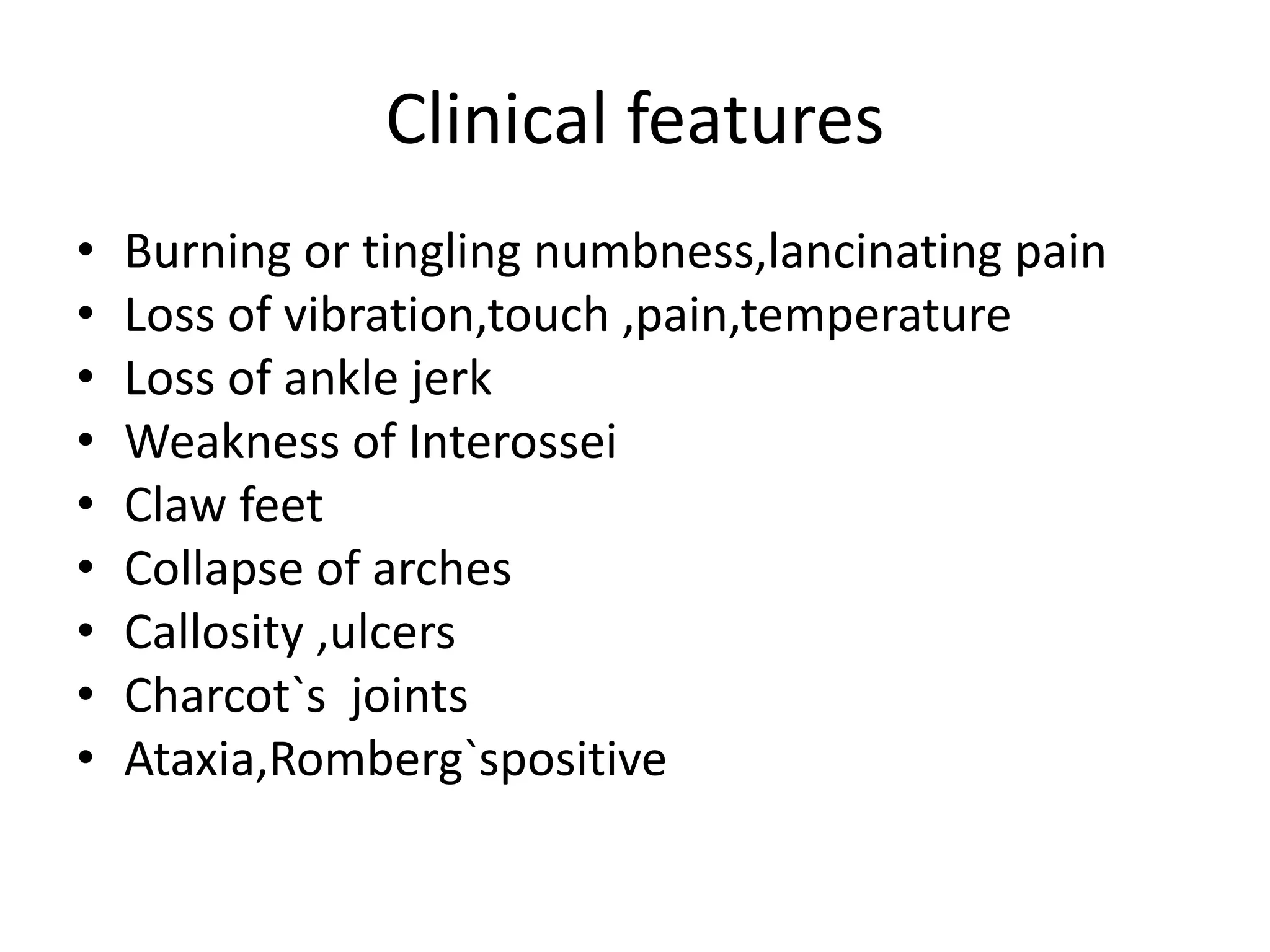
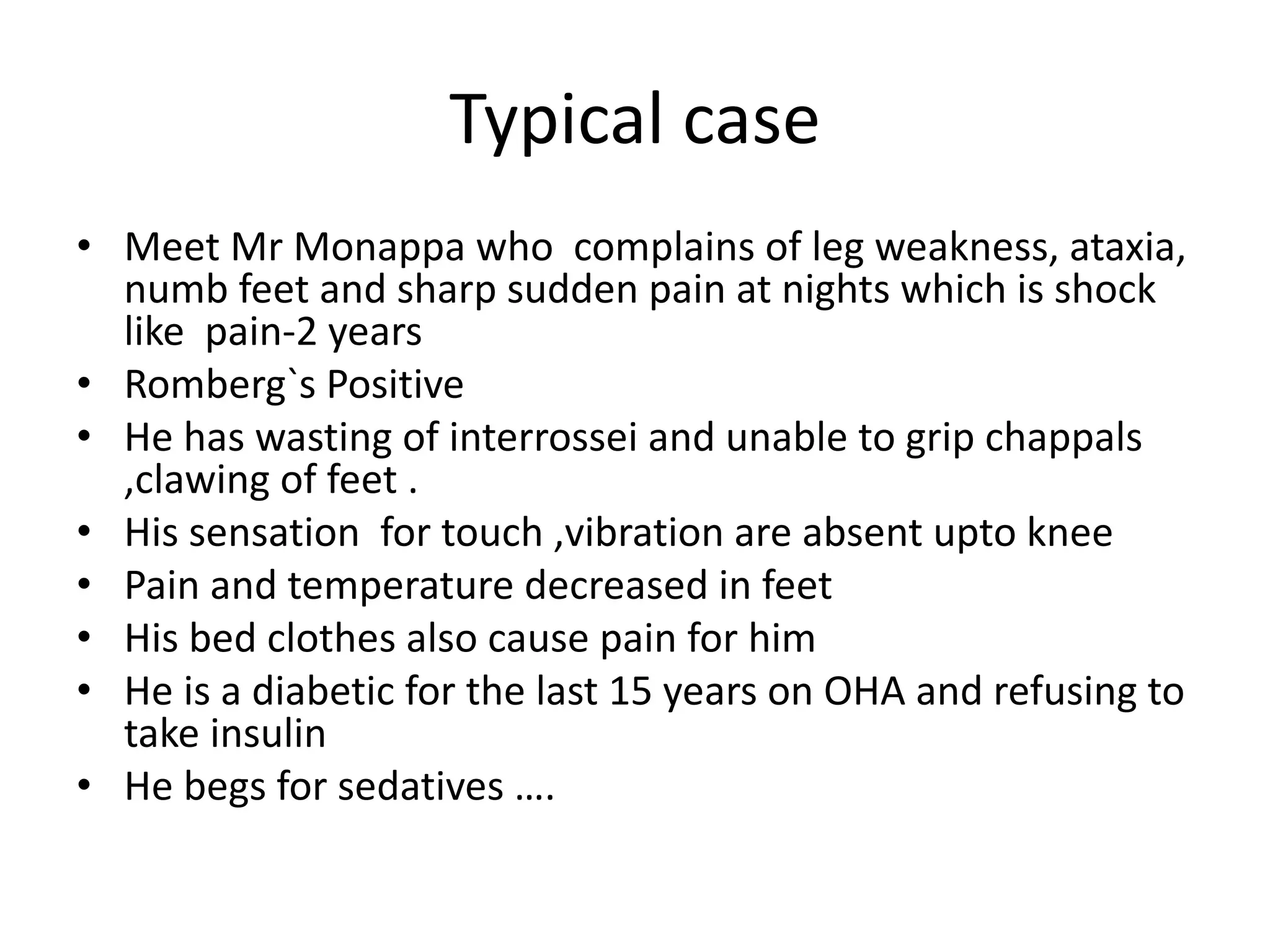
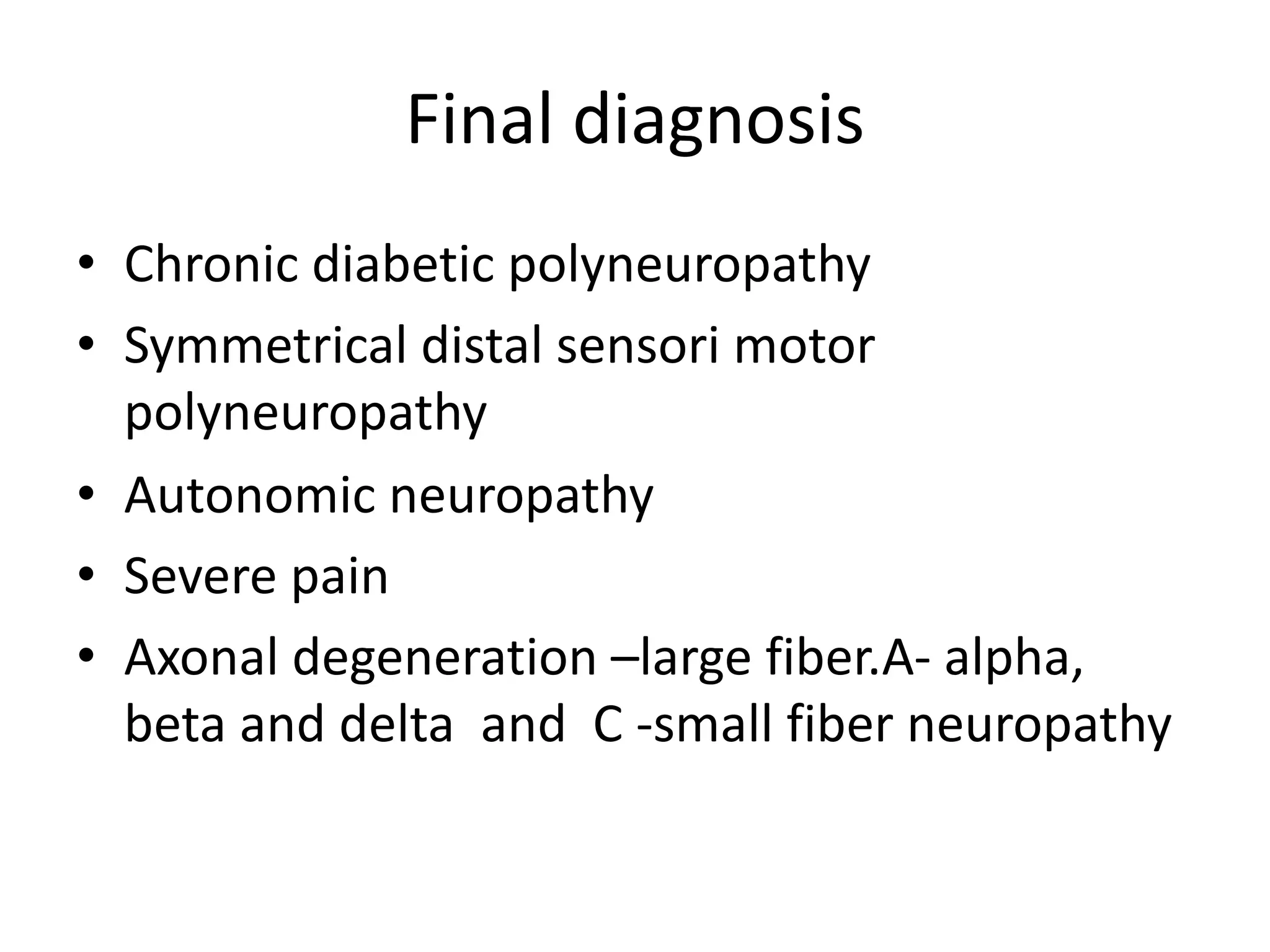
1. It describes a typical case of diabetic peripheral neuropathy presenting with leg weakness, numb feet, and pain.
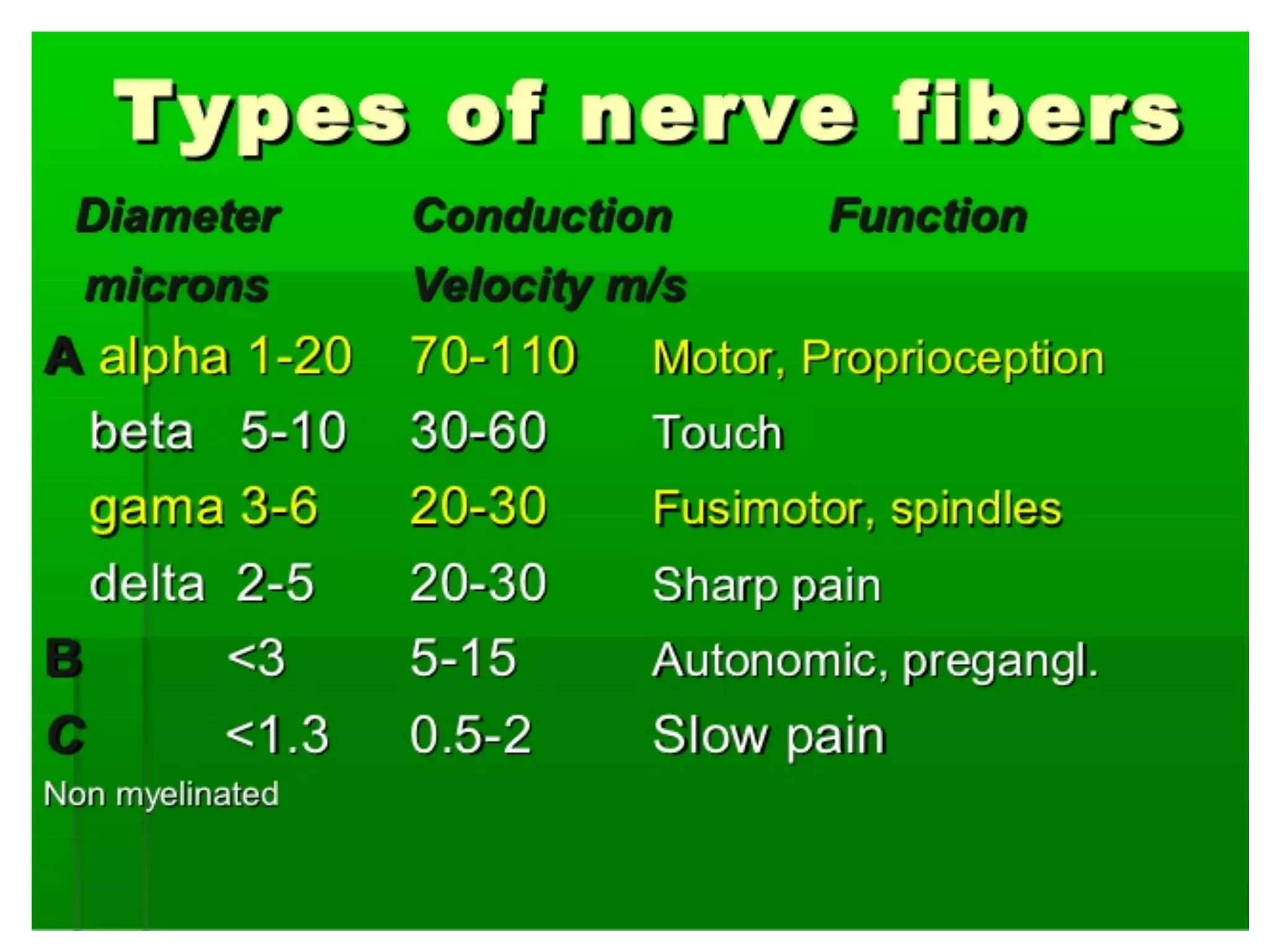
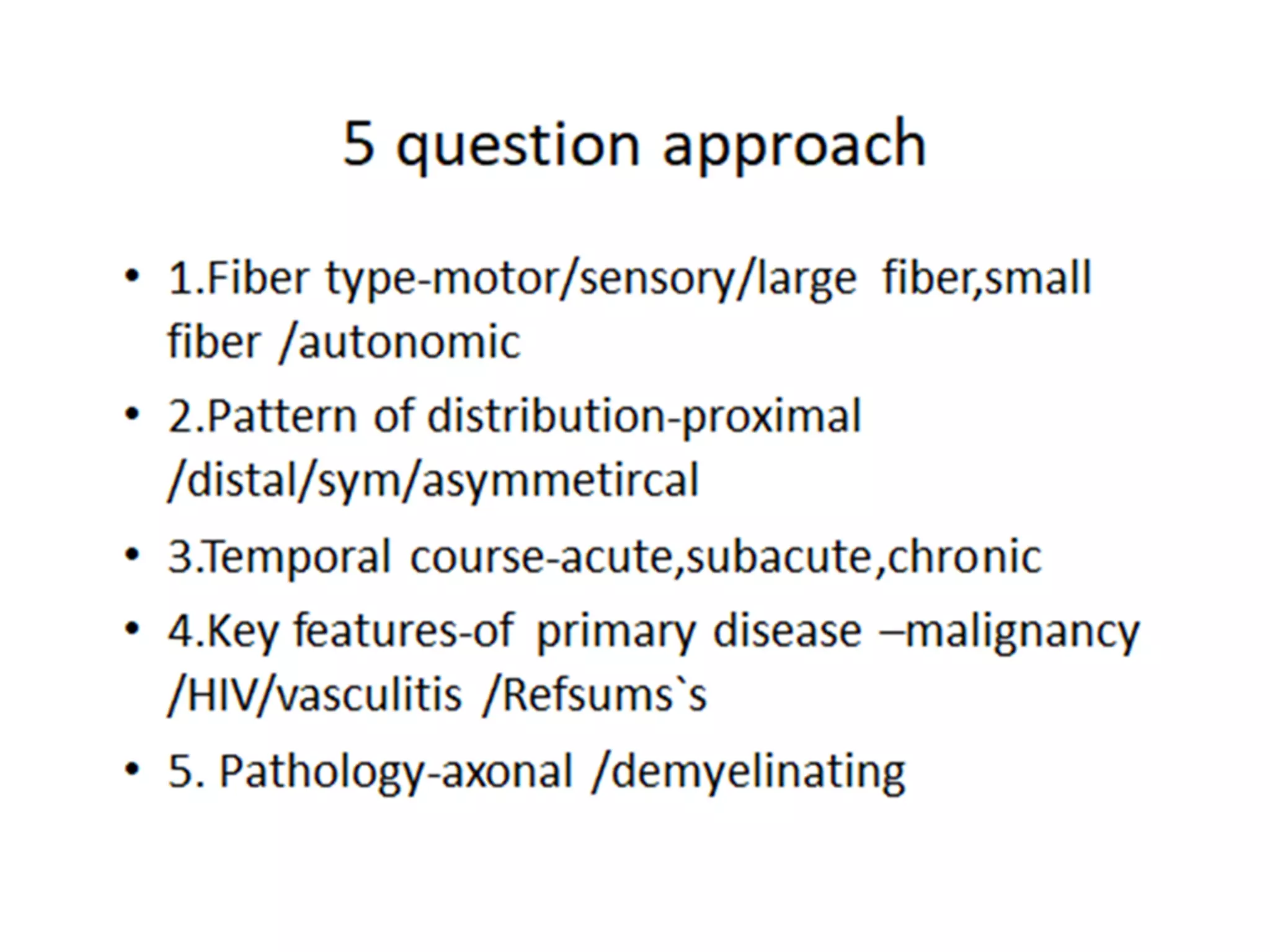
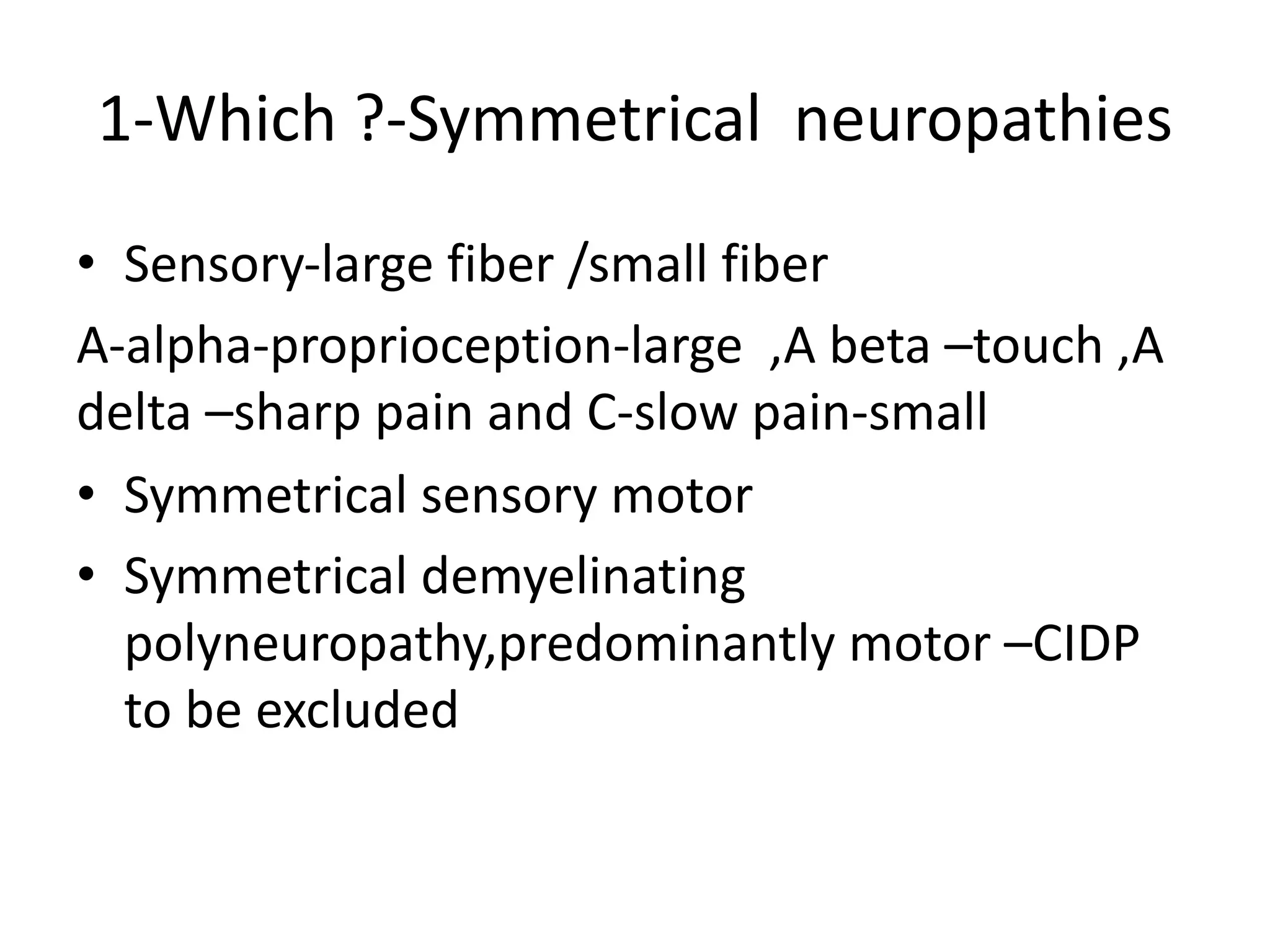
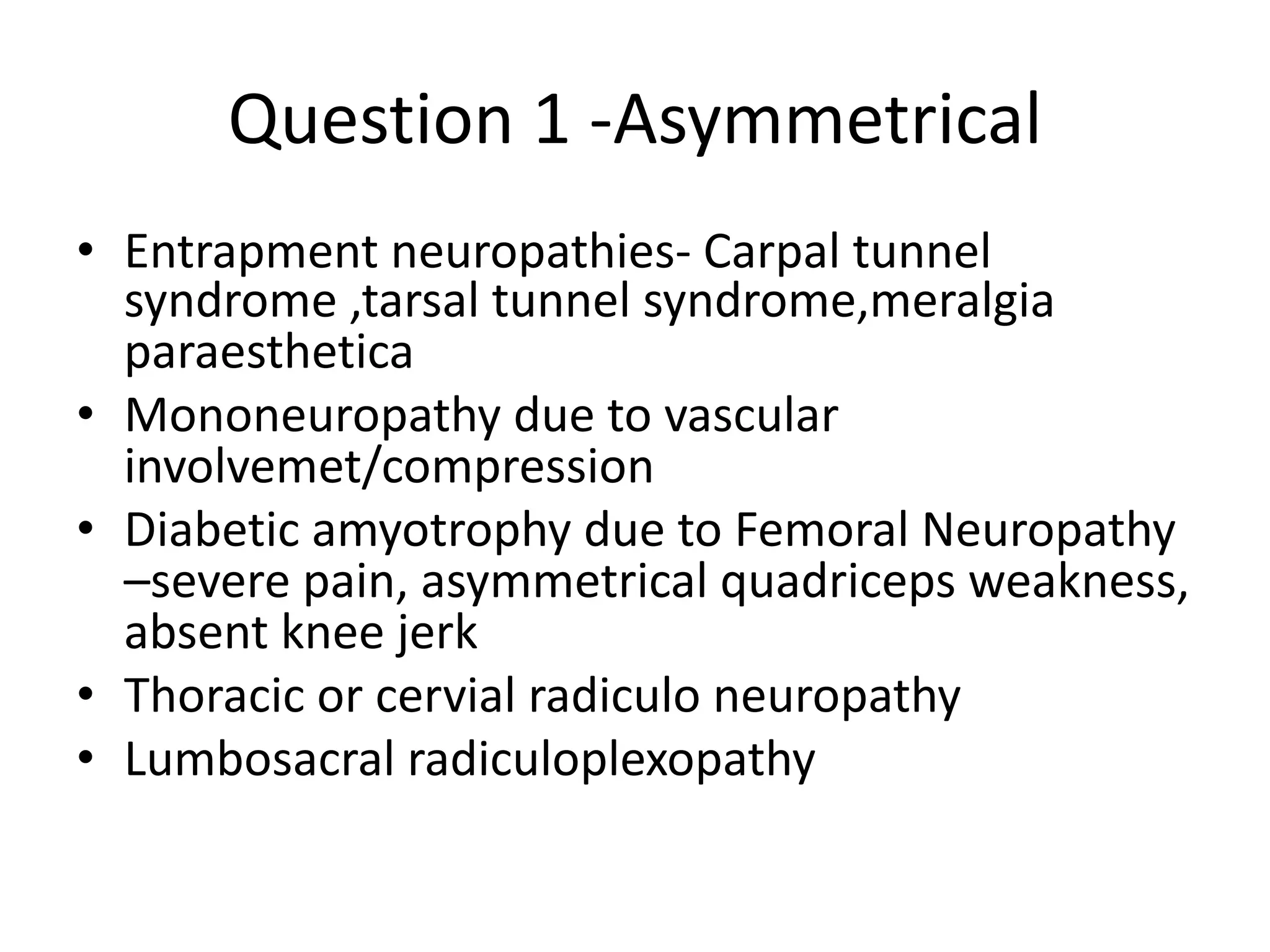
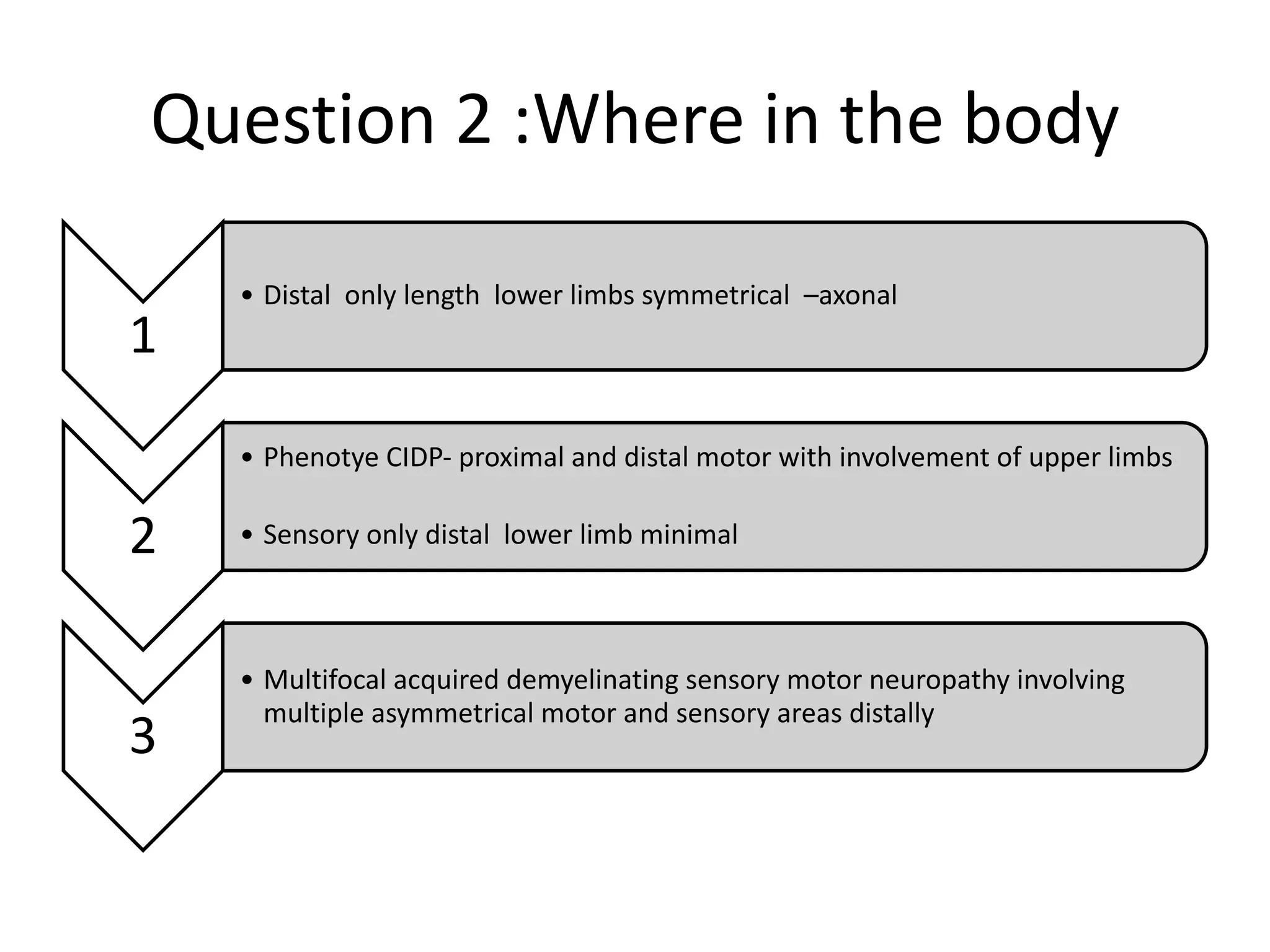
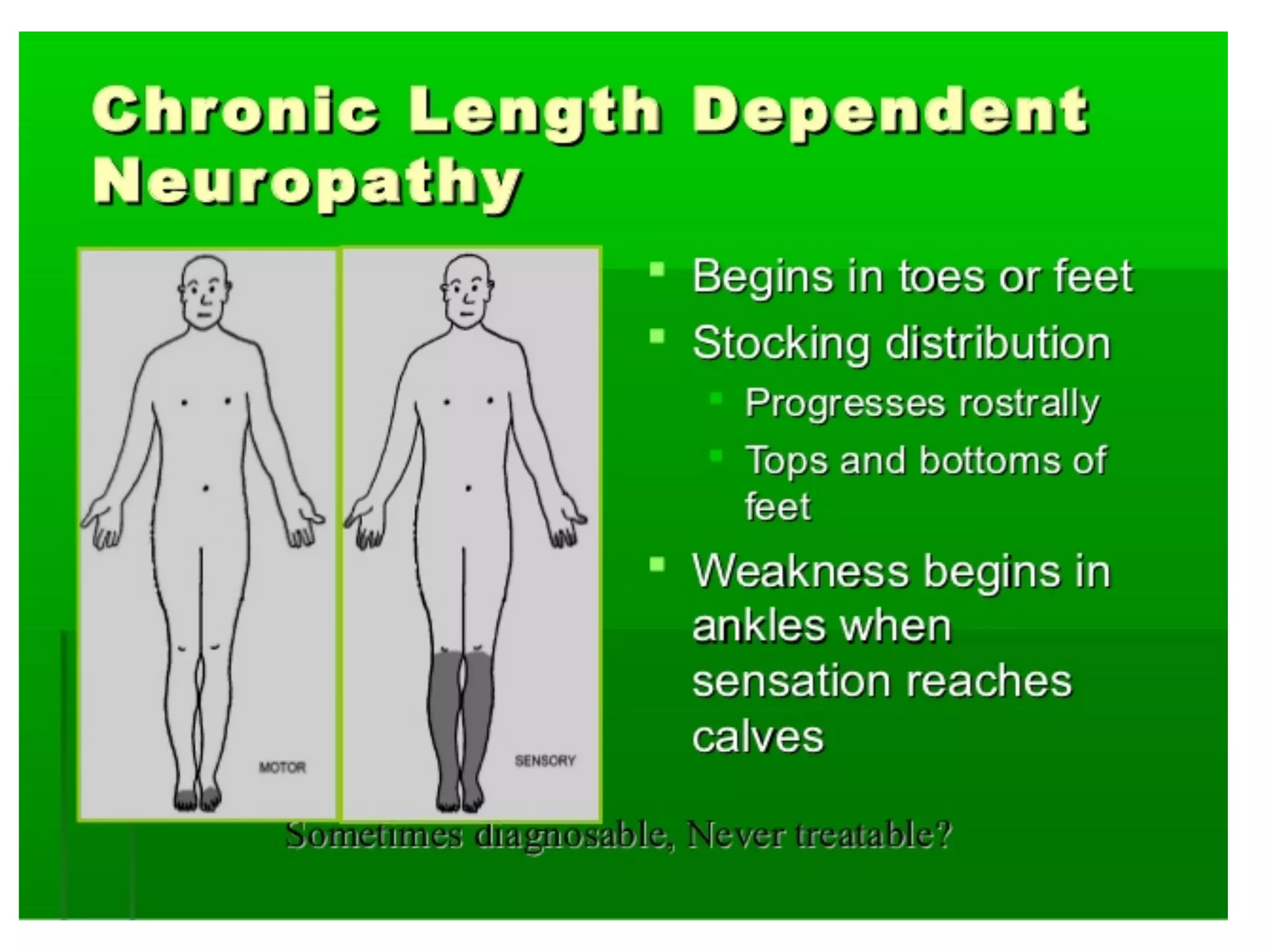
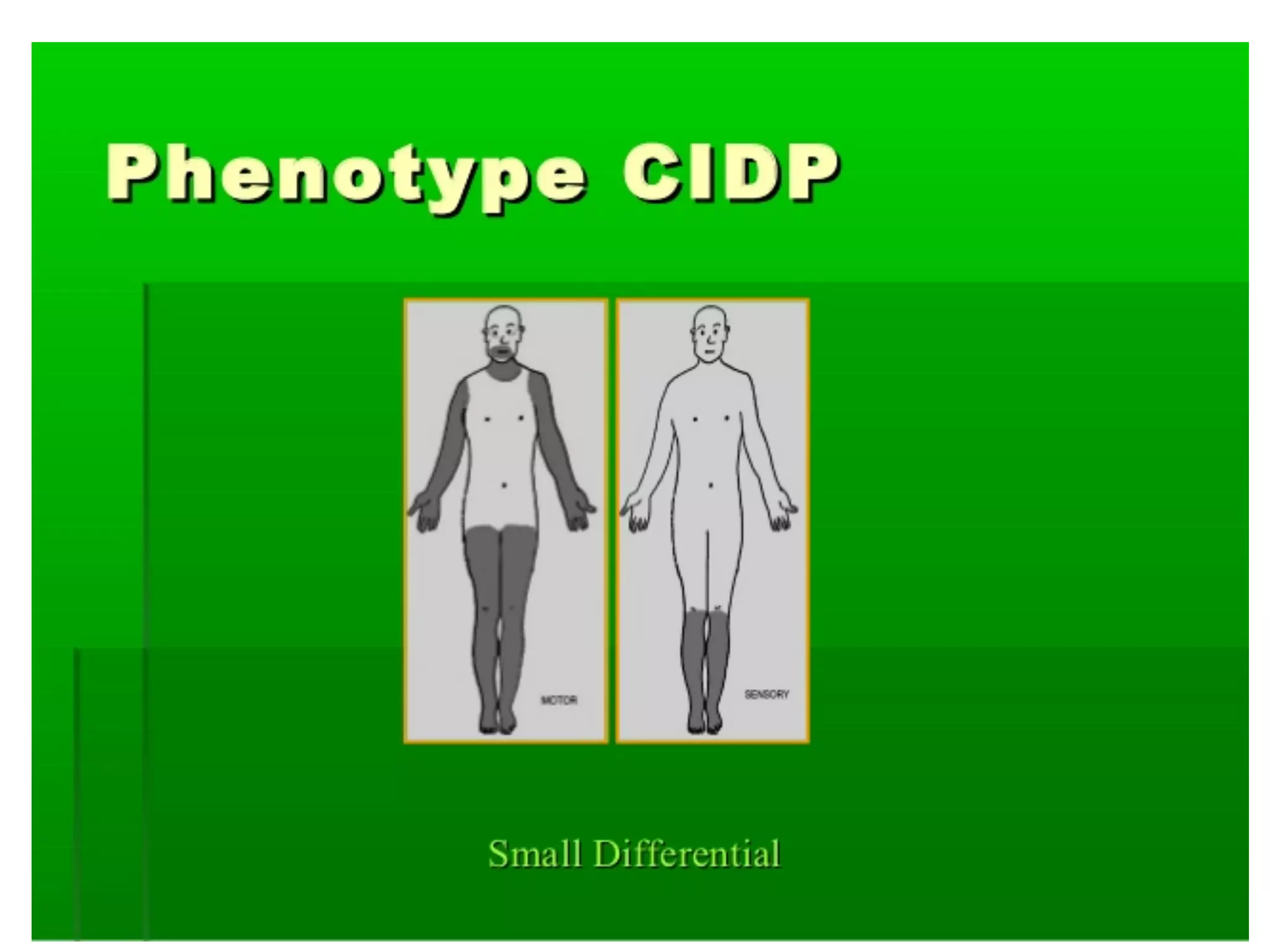
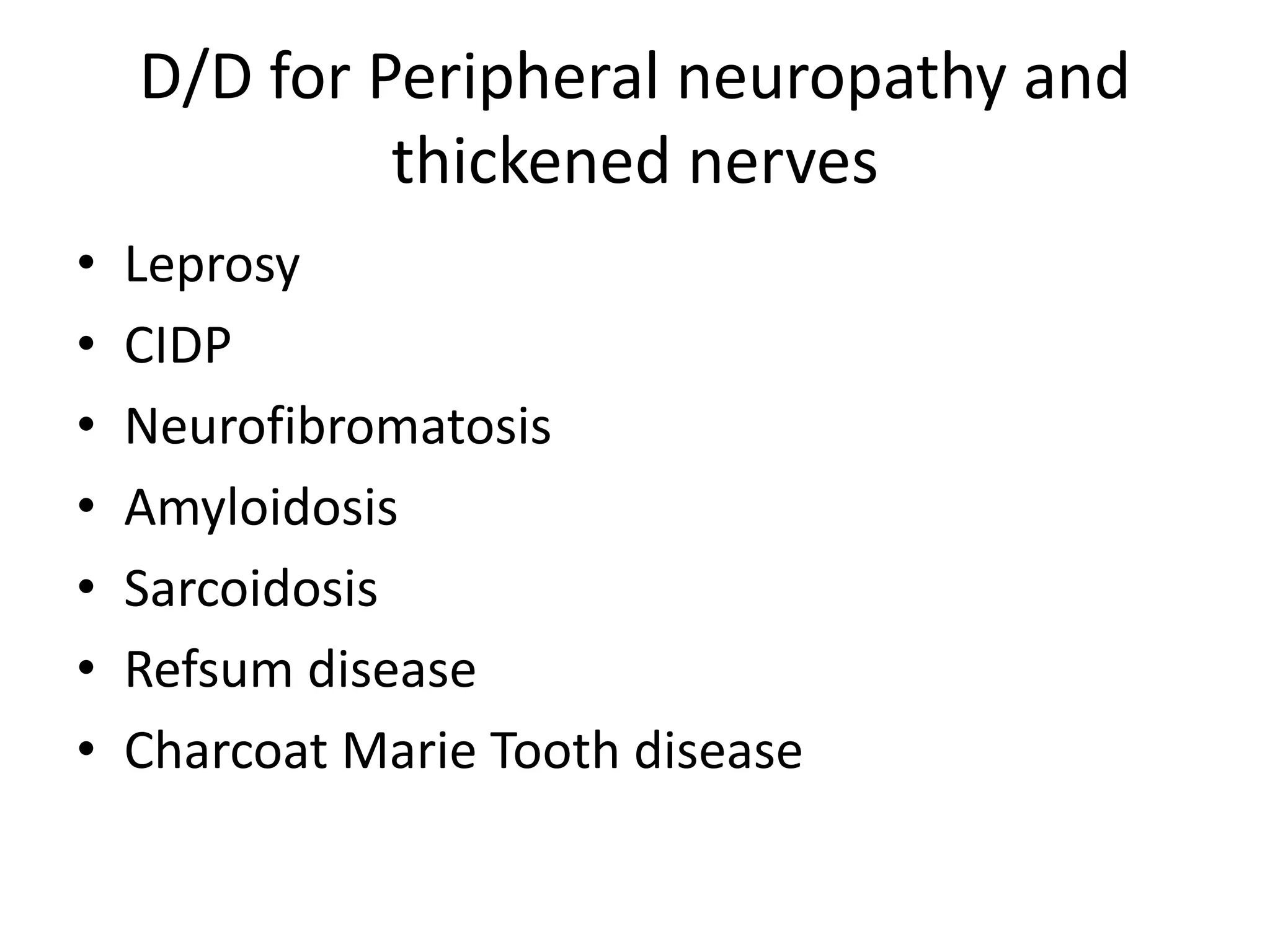
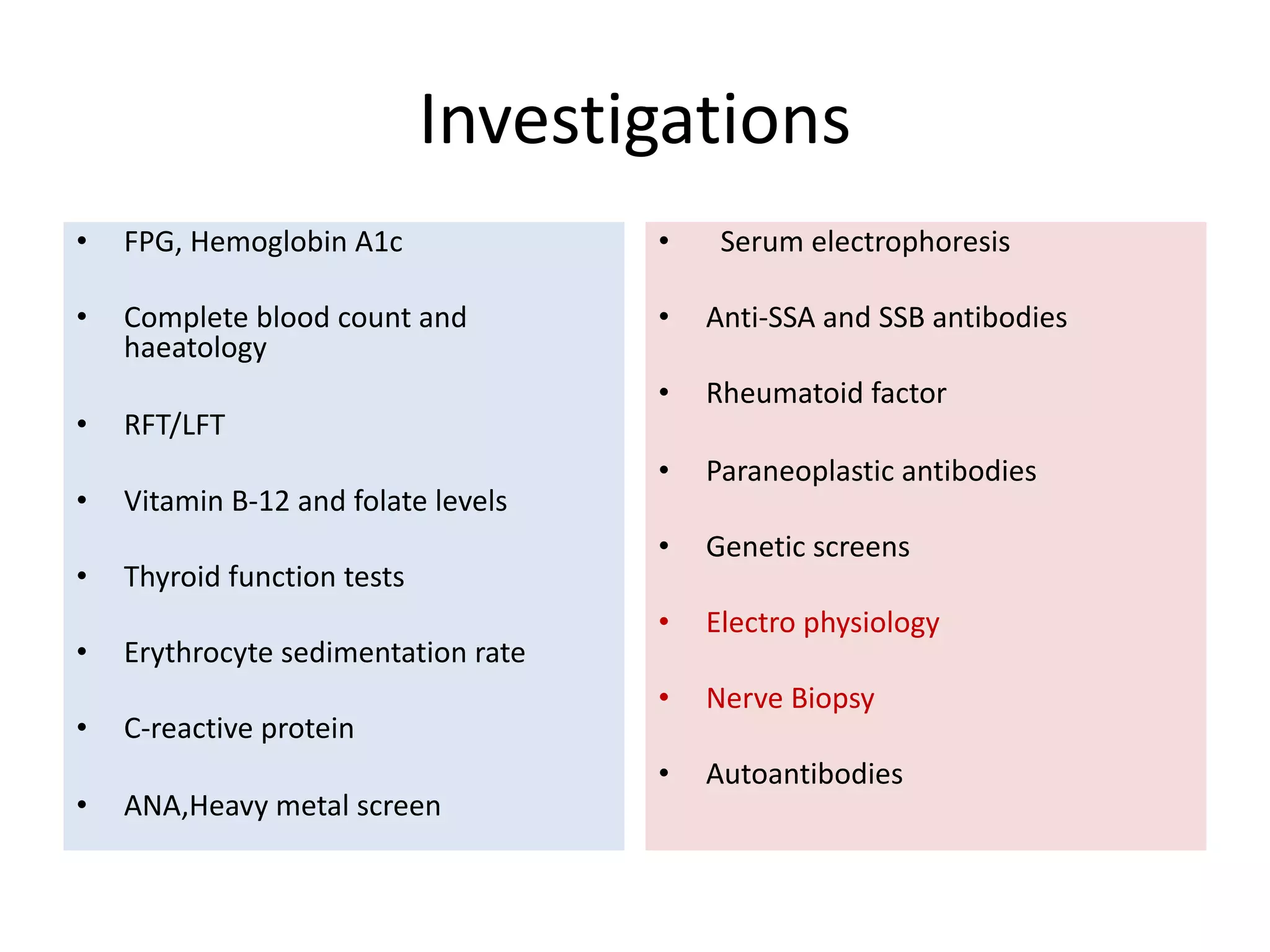
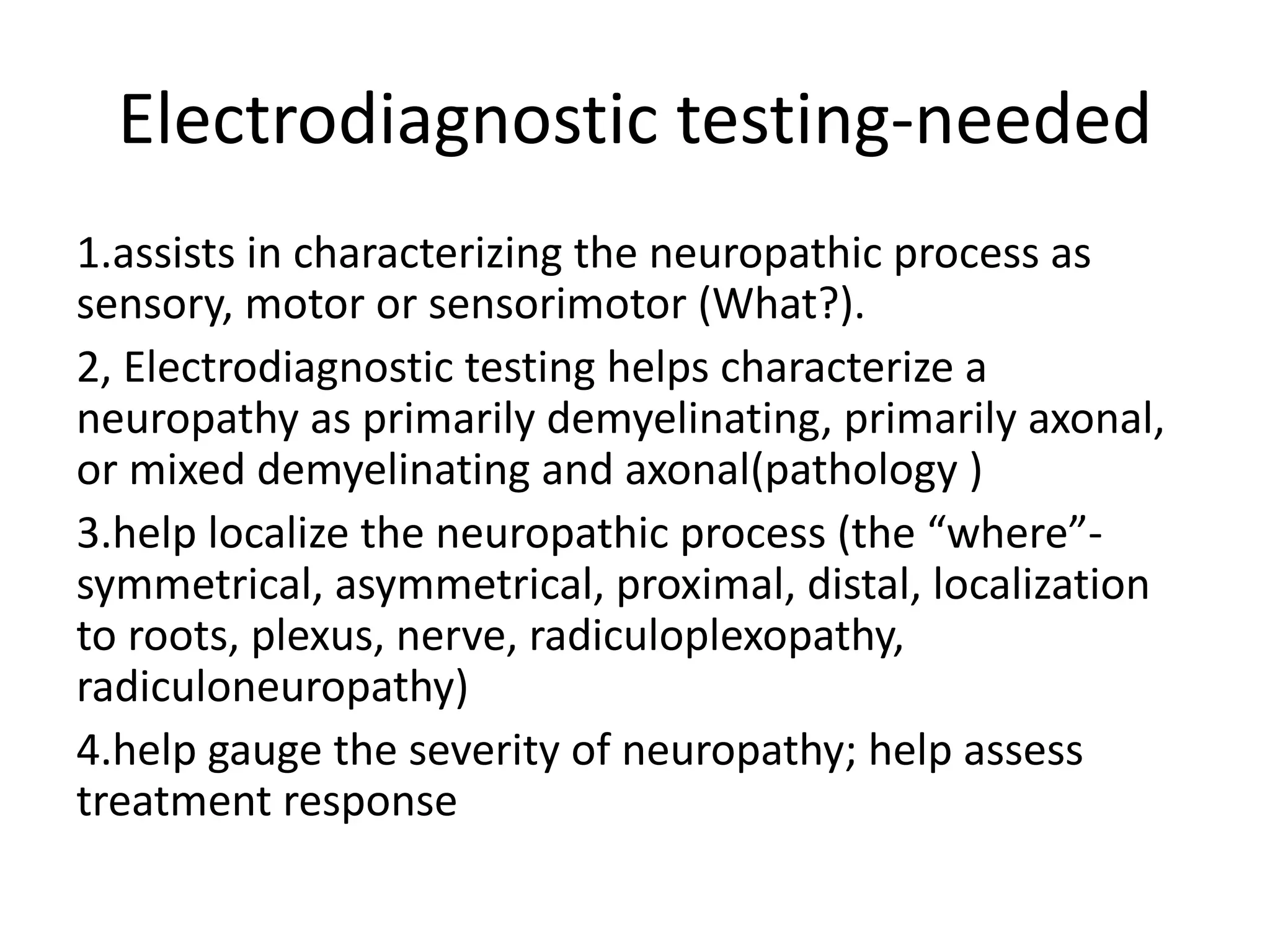
2. It asks questions to help classify the neuropathy including type of nerve fibers involved and diagnostic approach.
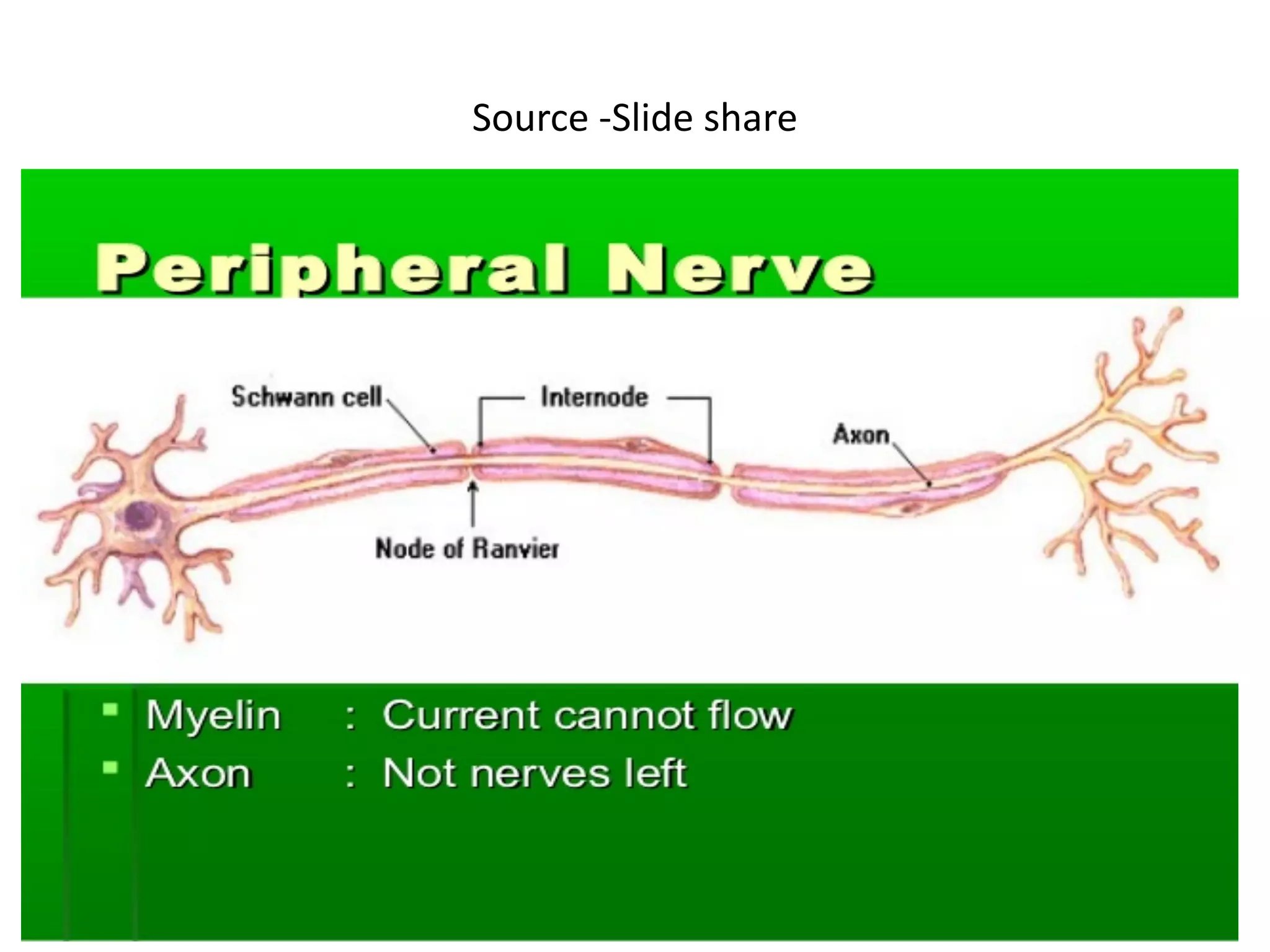
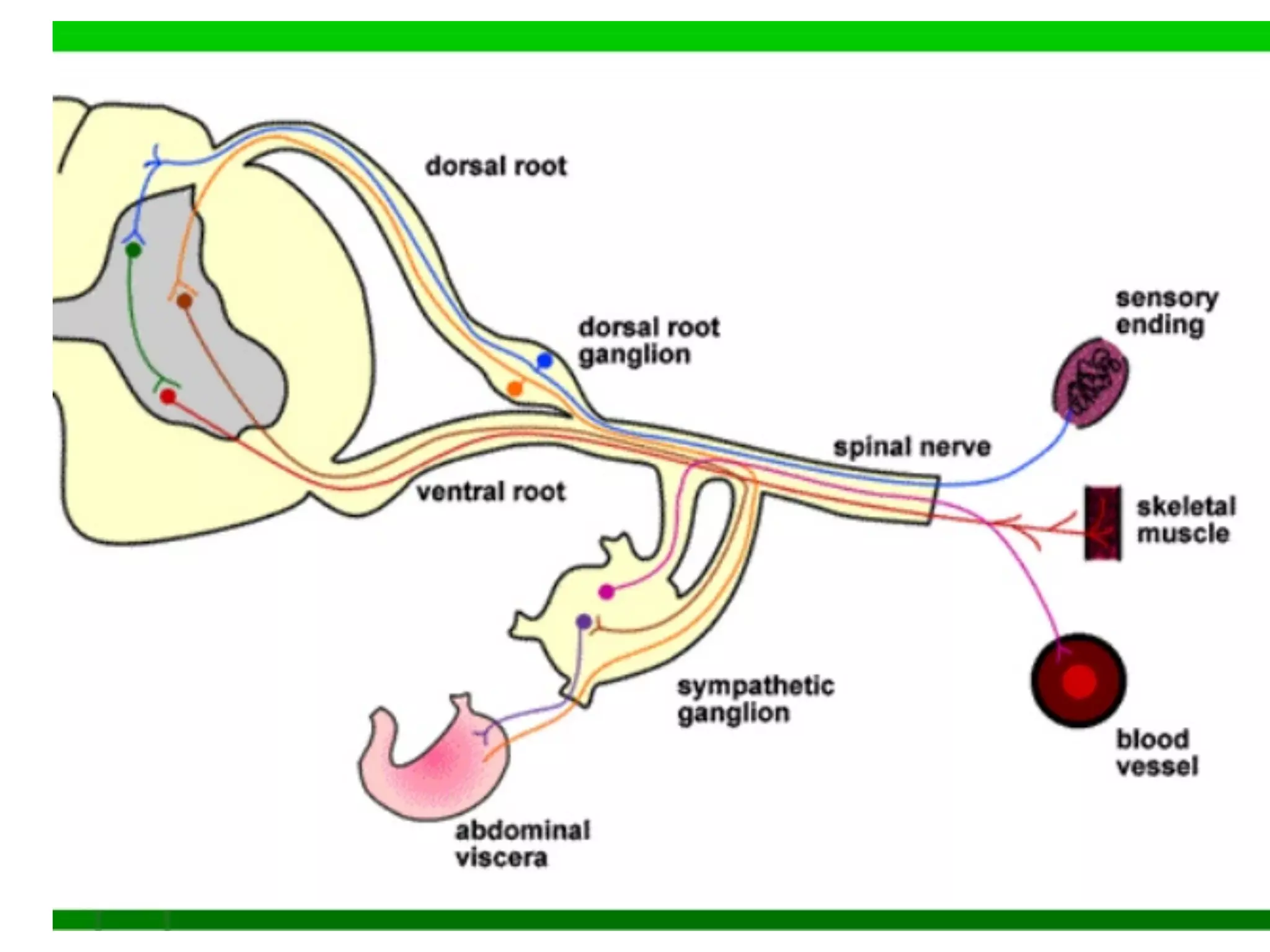
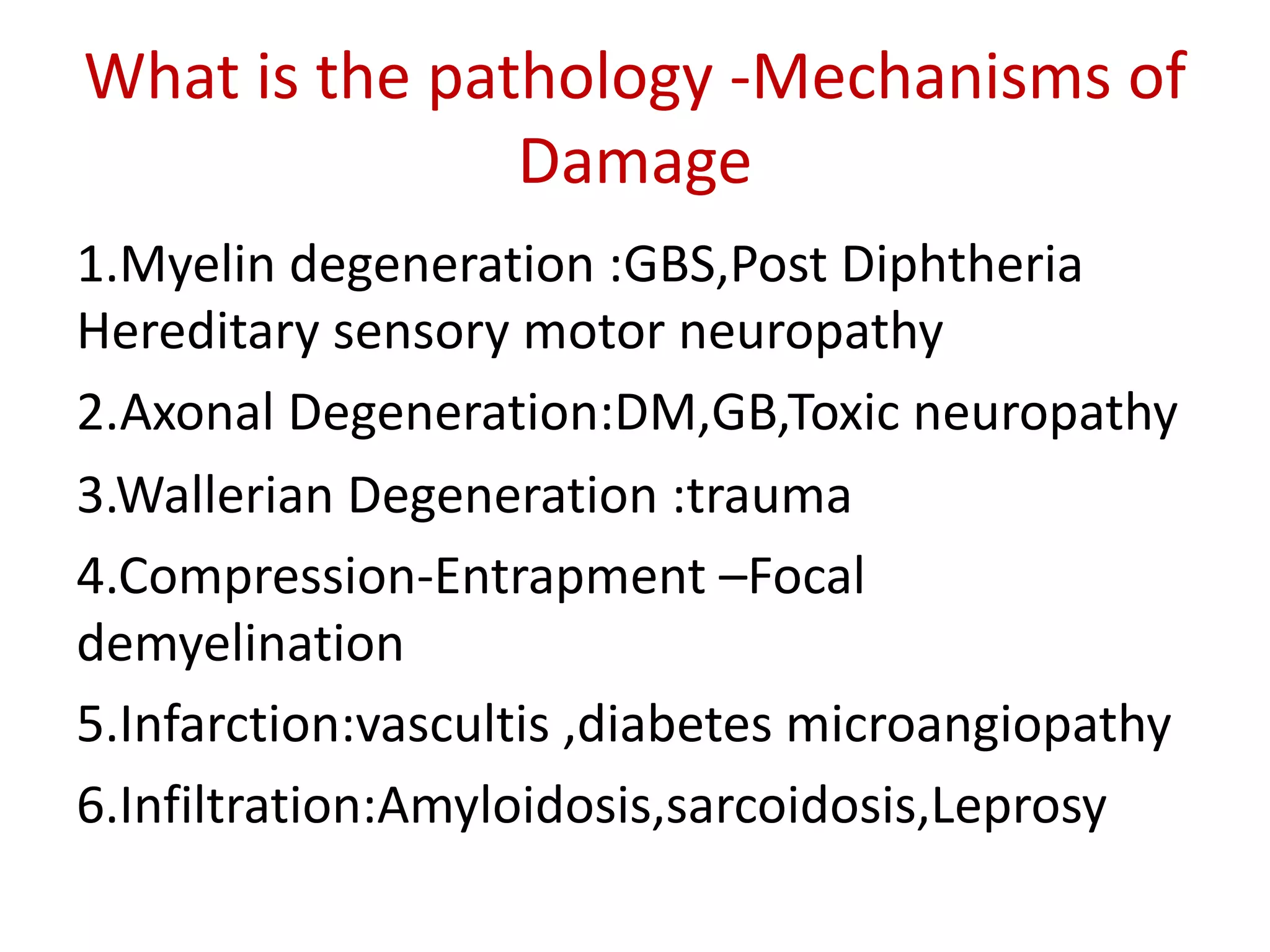
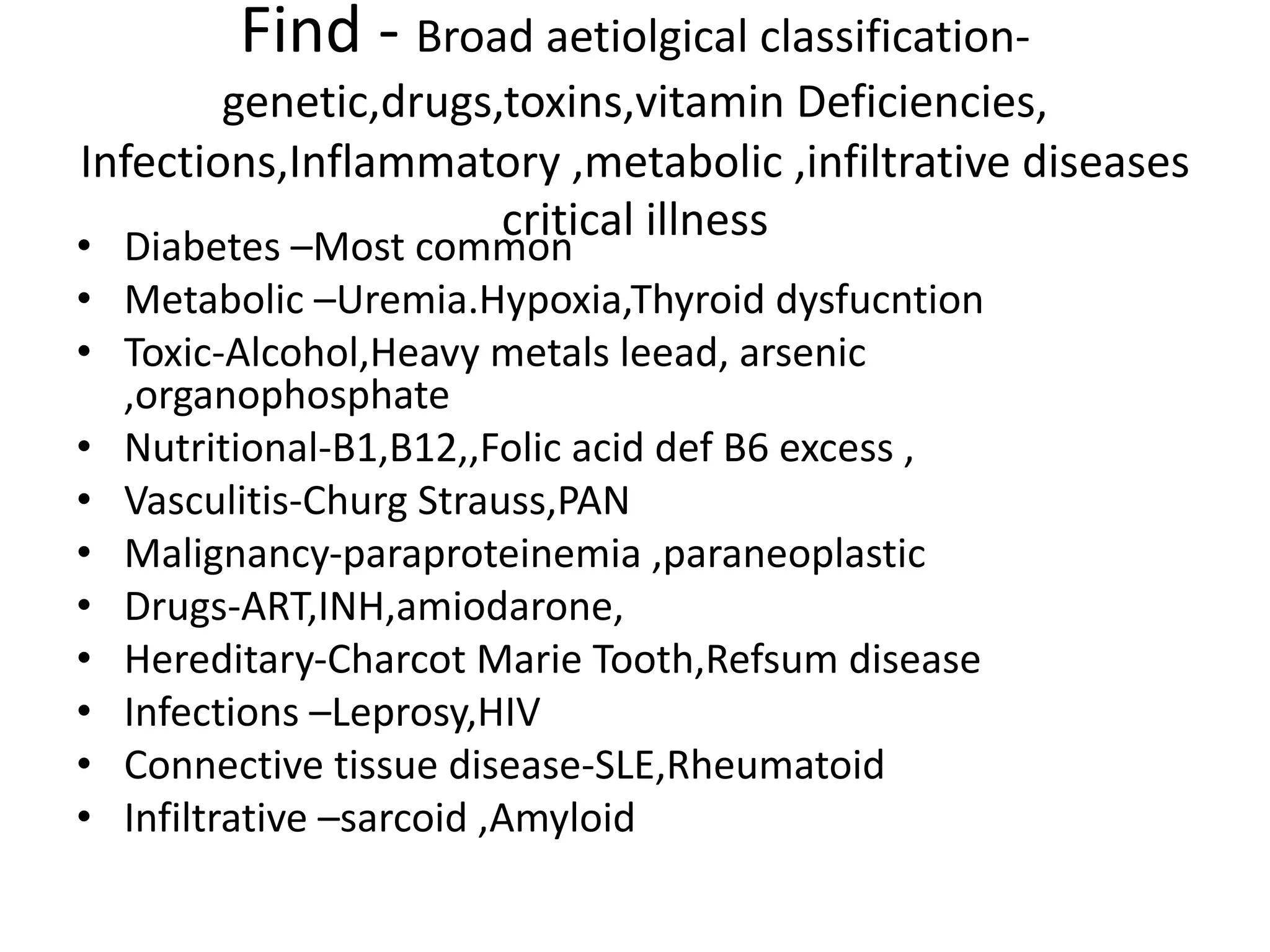
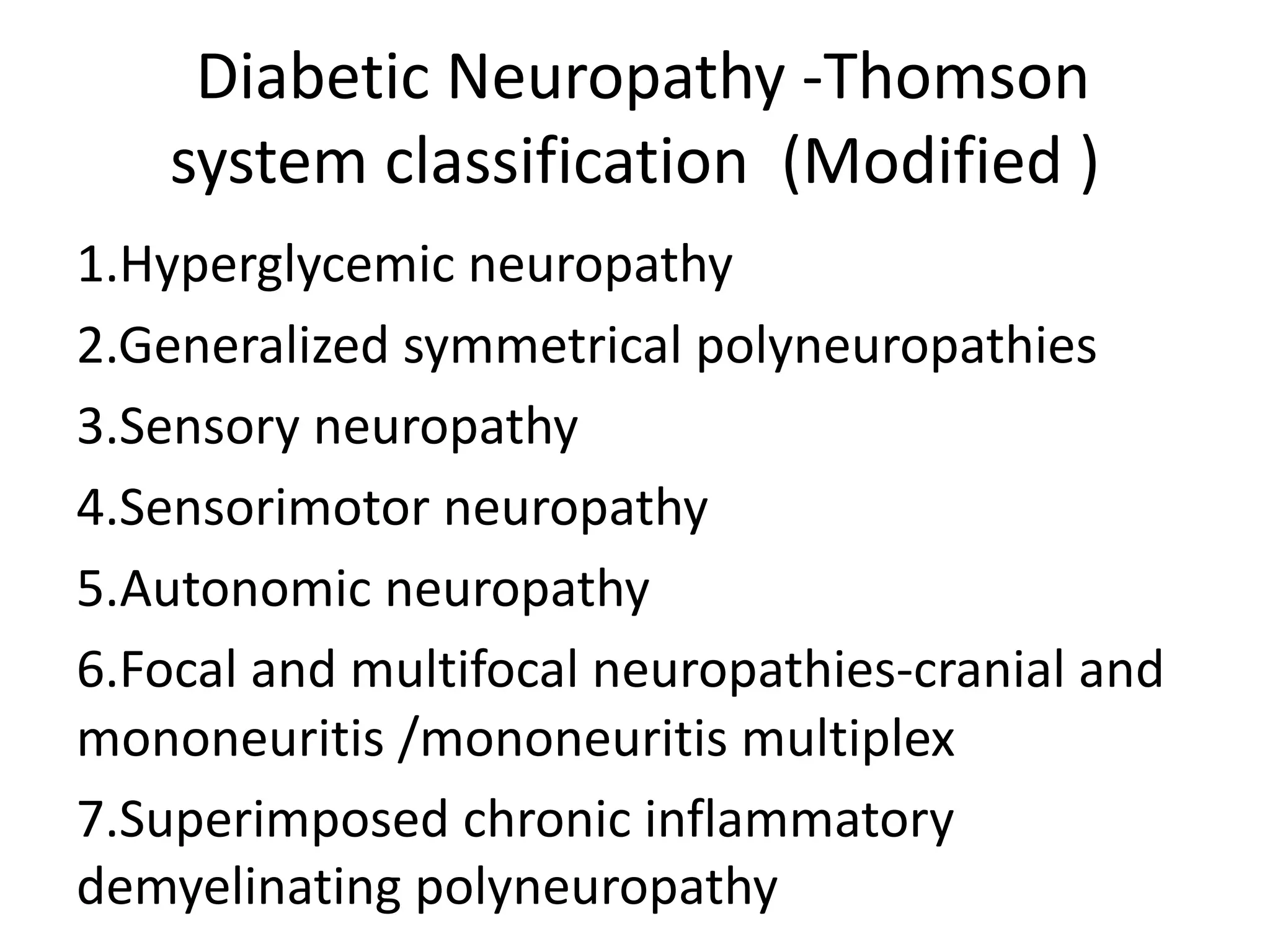
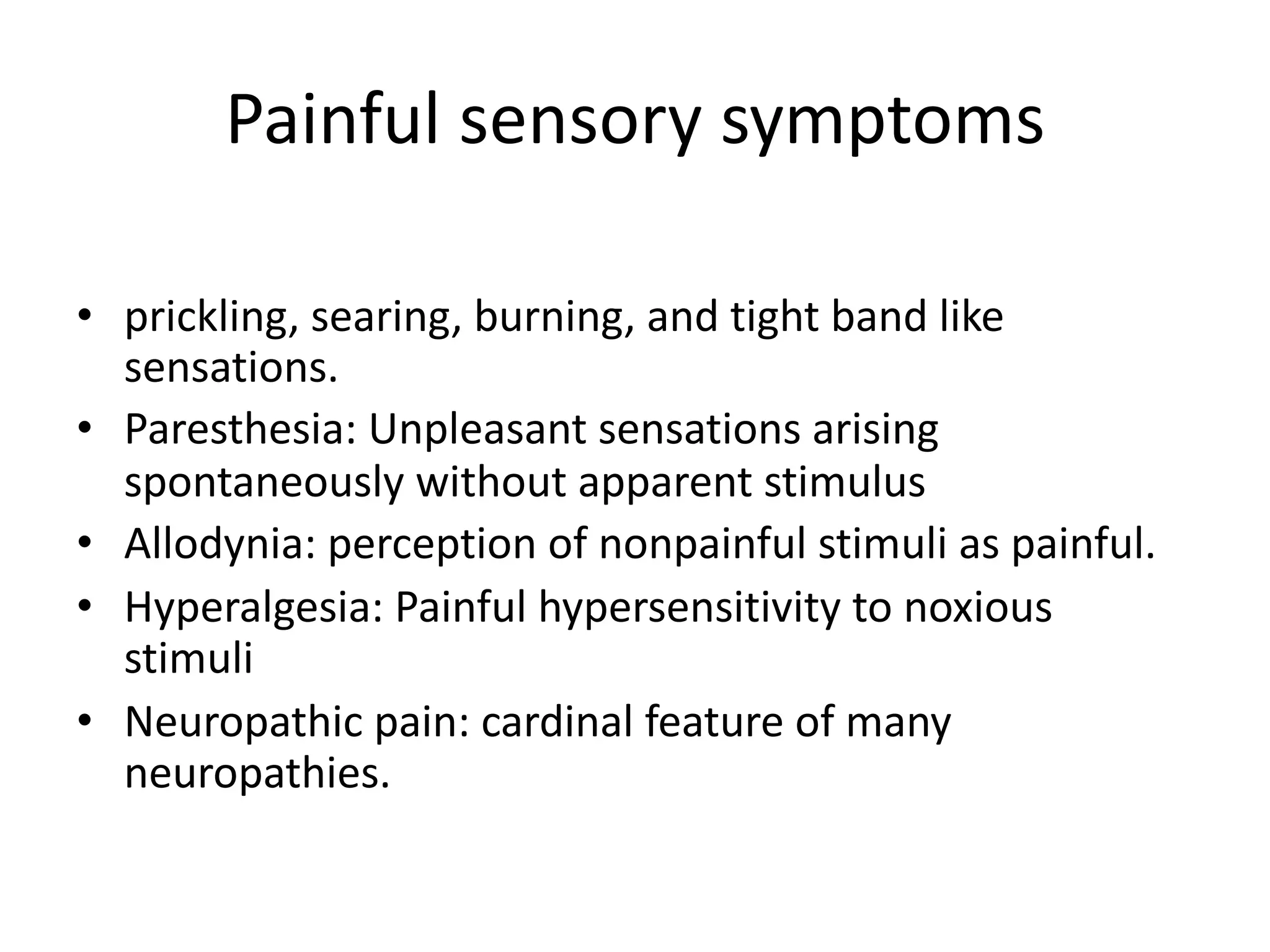
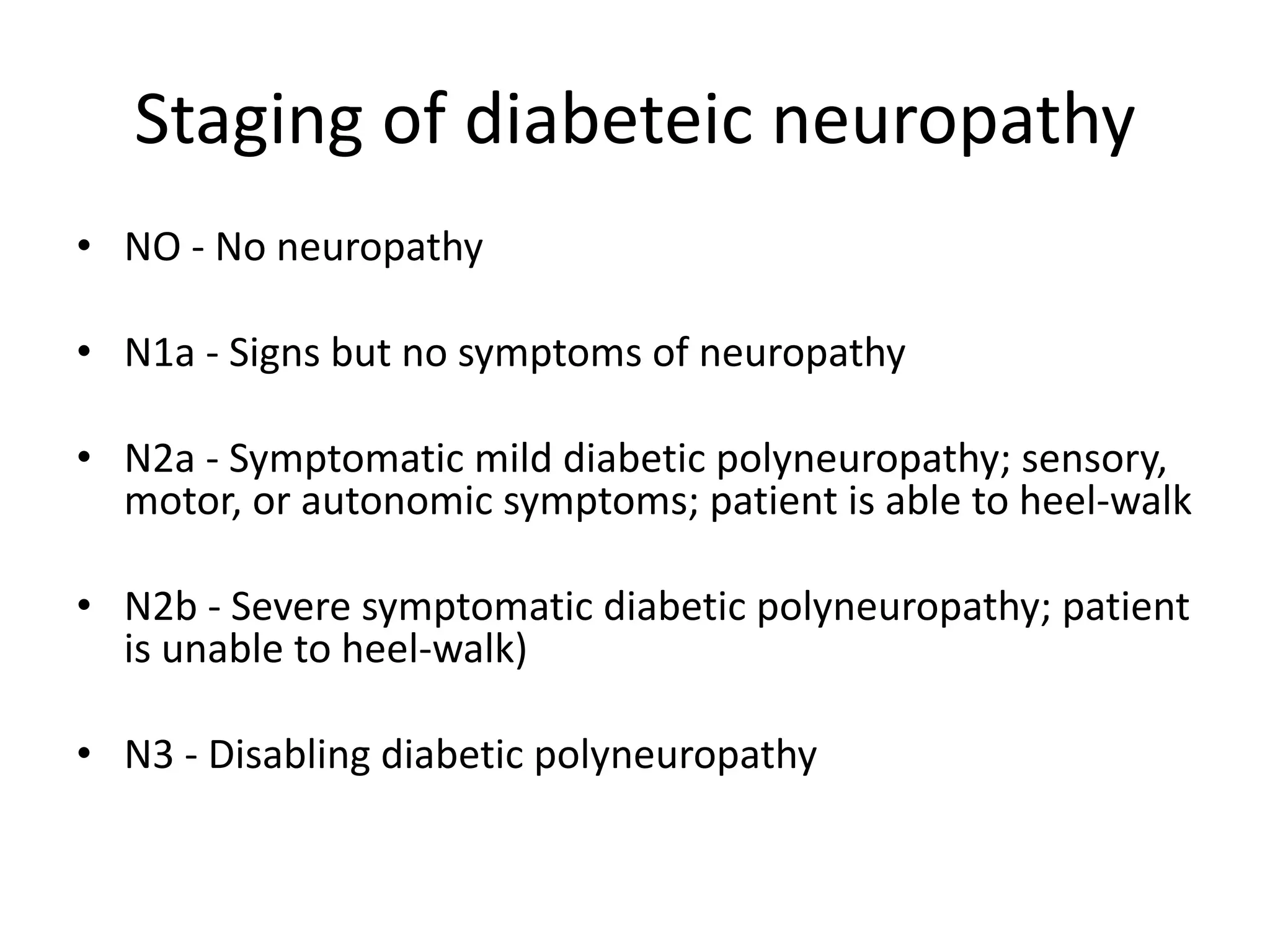
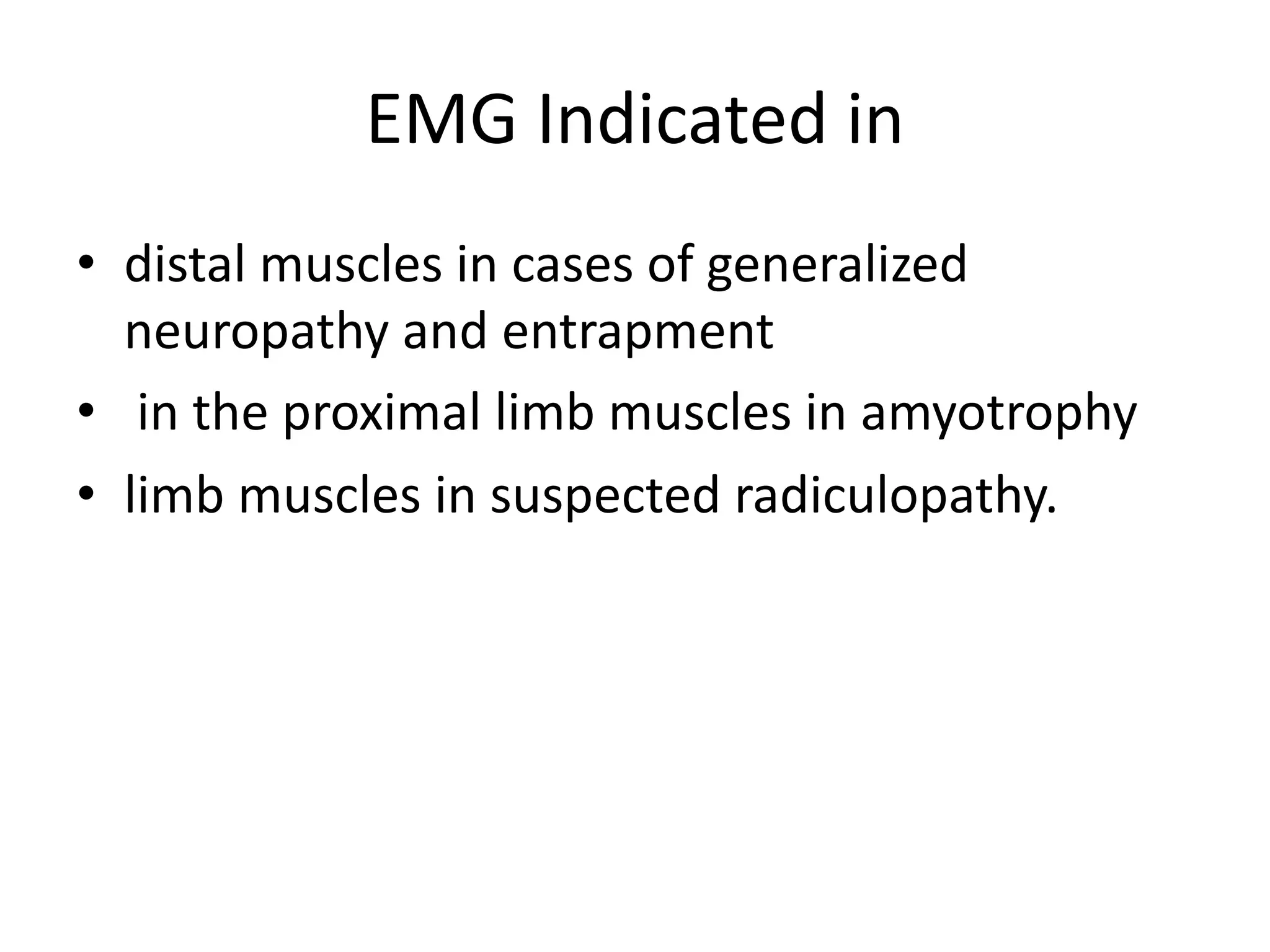
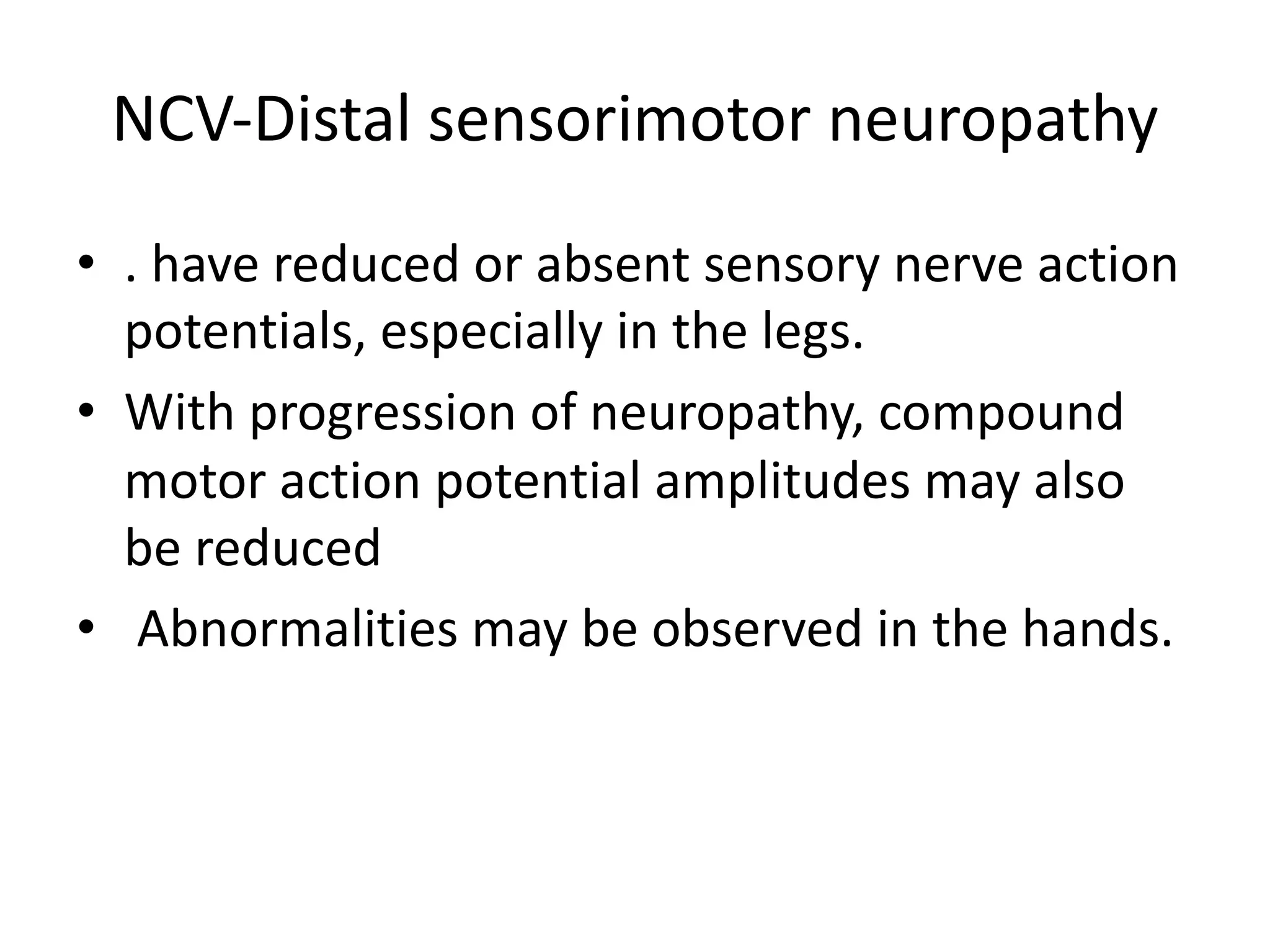
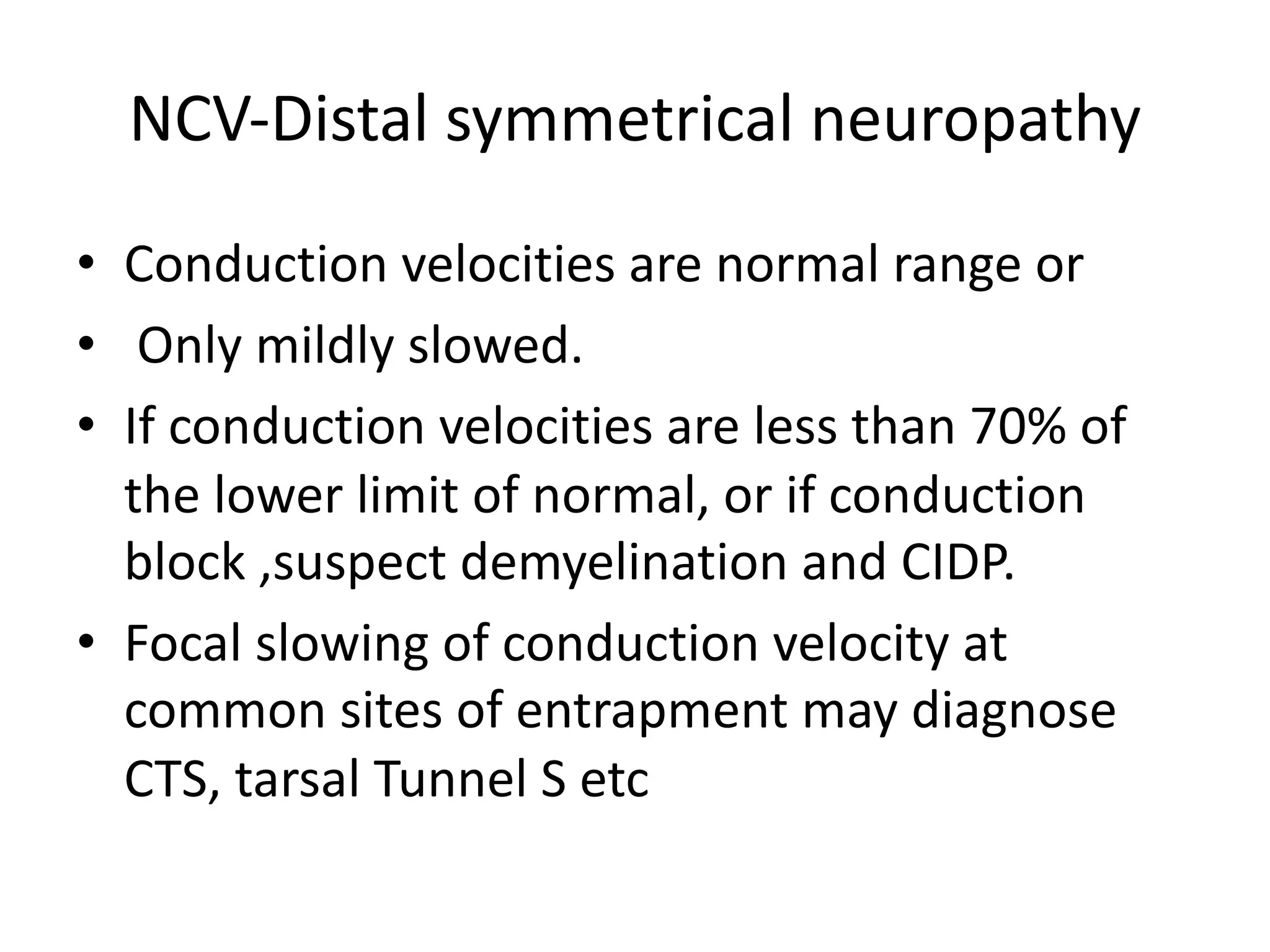
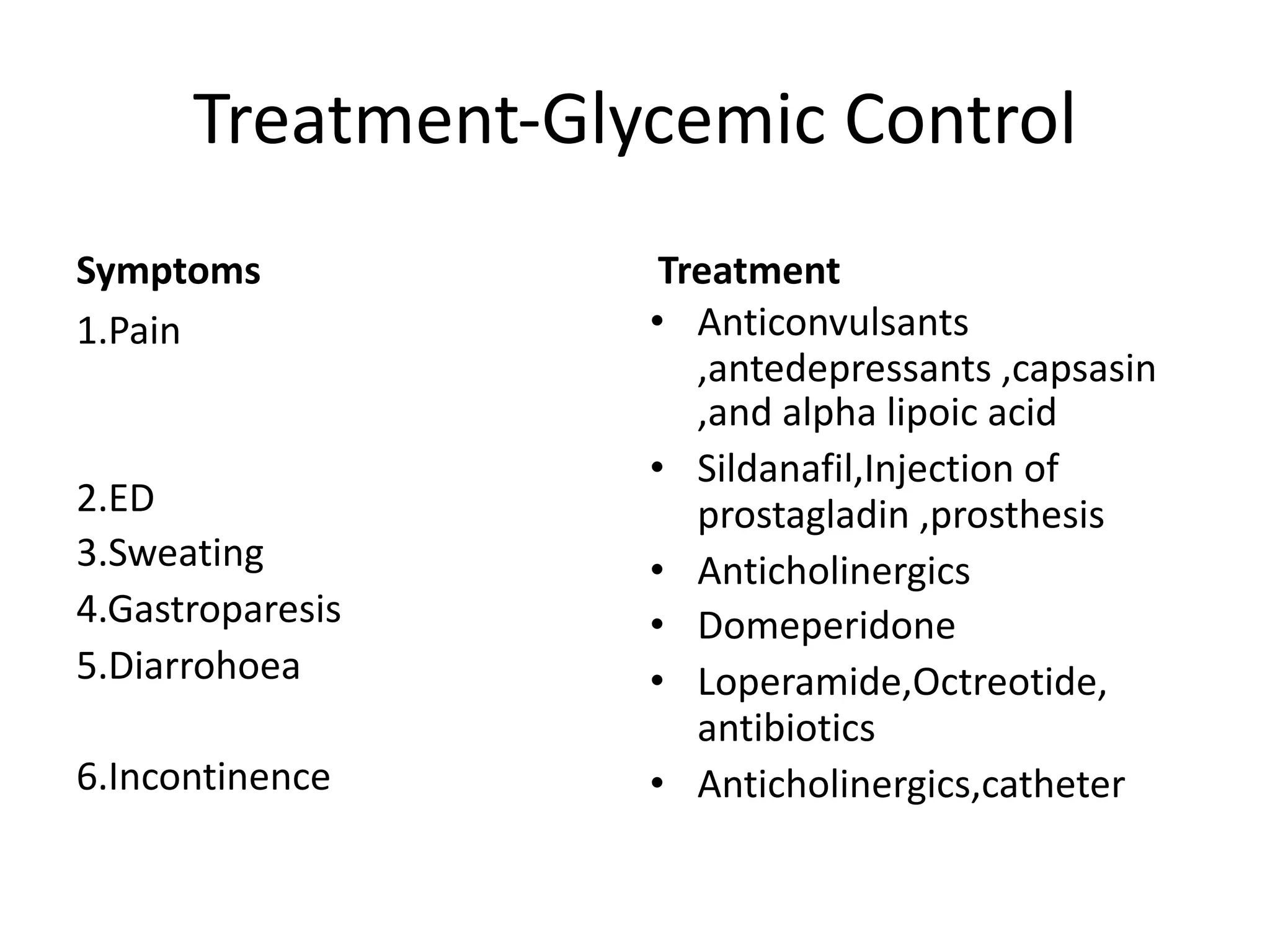
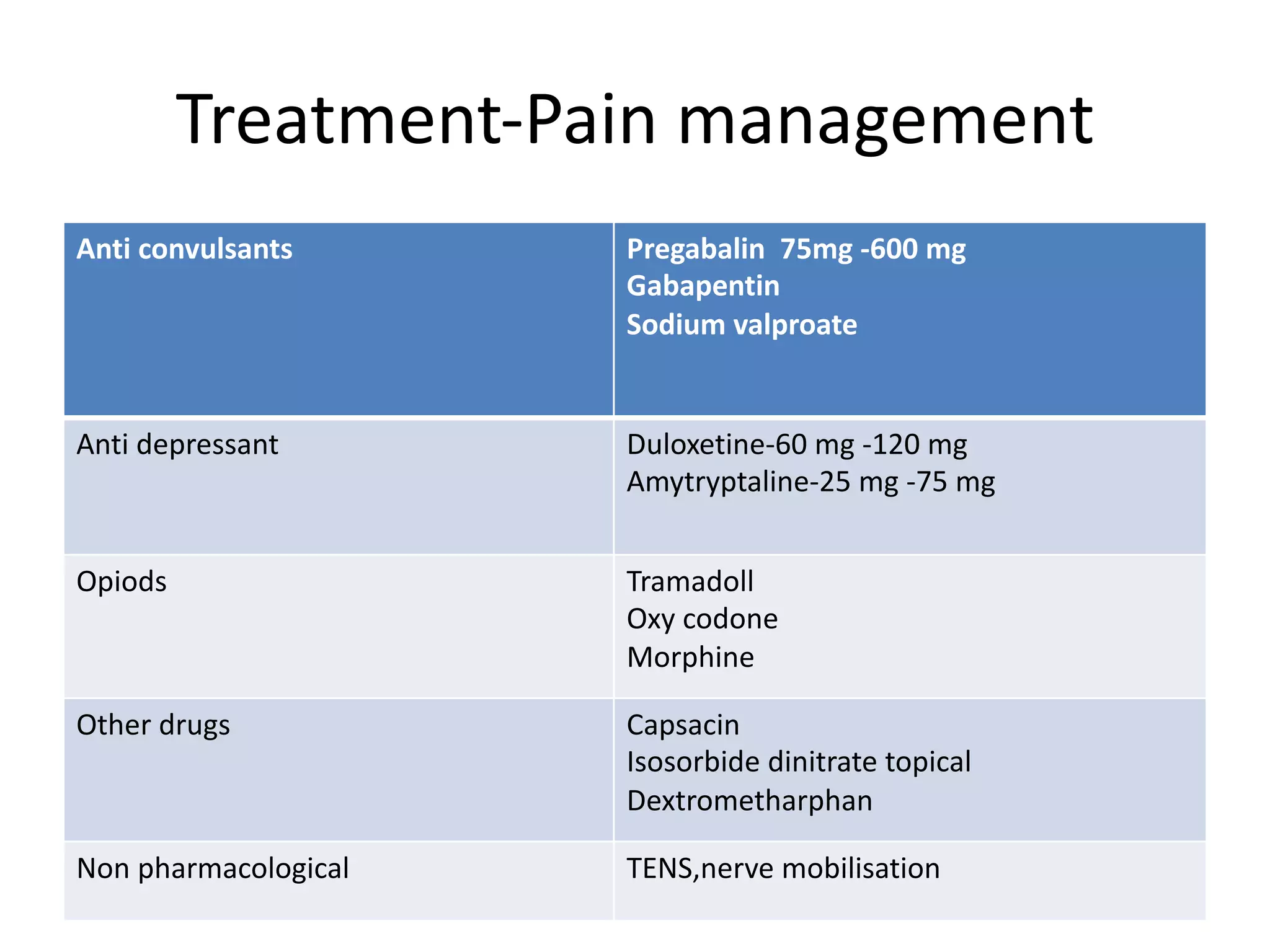
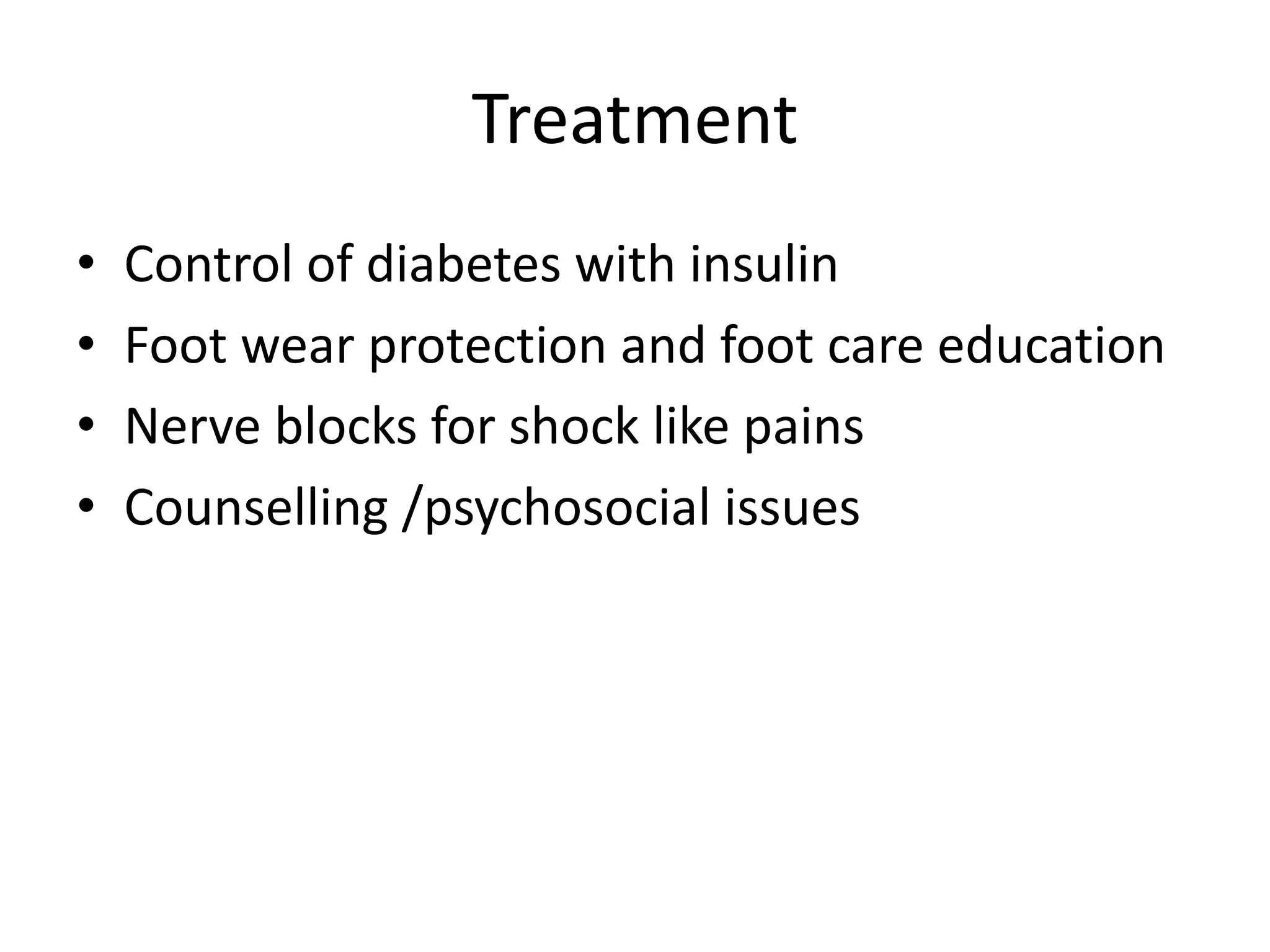
3. It outlines the lesson which will define neuropathy, discuss anatomy/physiology, classification, clinical features, investigations and management.