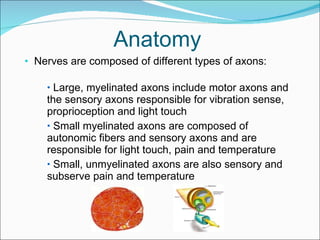
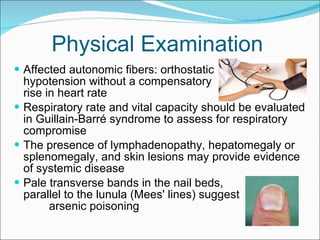
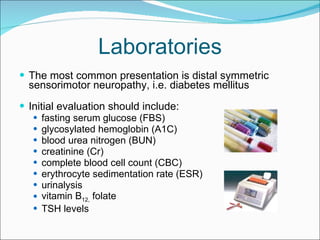
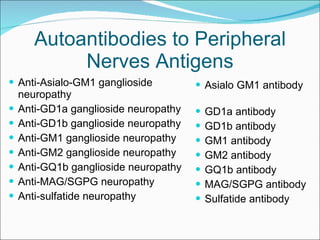
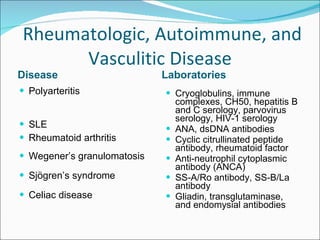
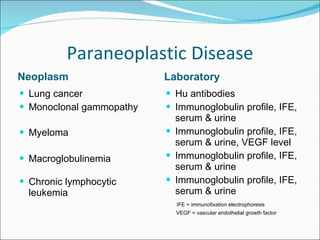
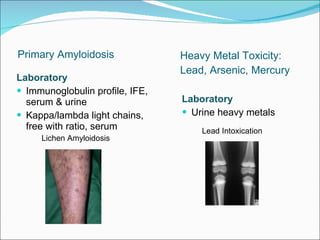
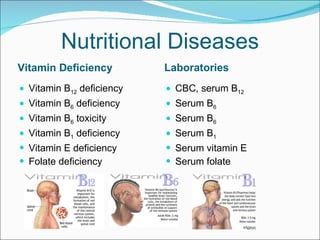
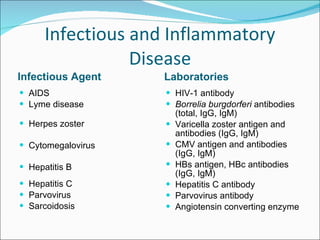
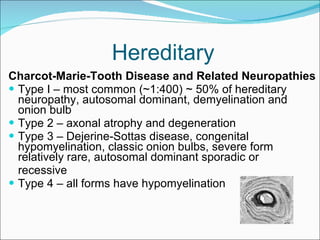
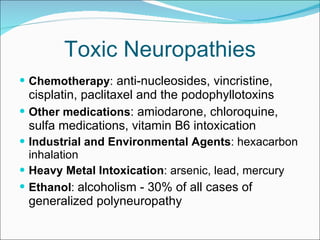
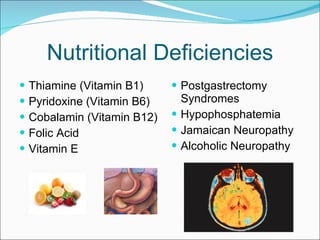
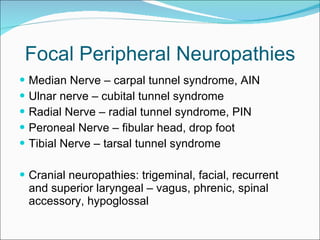
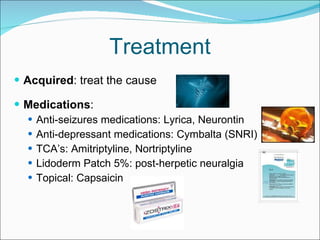
This document provides a comprehensive overview of peripheral nerve anatomy, pathologies, clinical examinations, and diagnostic evaluations associated with neuropathies. It details symptoms, laboratory assessments, and common causes including metabolic, infectious, autoimmune, and hereditary conditions. Treatment options and the role of rehabilitation strategies are also discussed, highlighting the complex interplay of factors affecting peripheral nerve health.