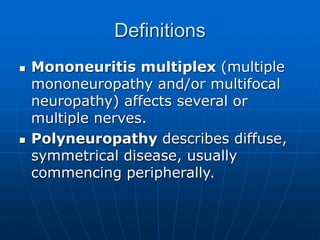
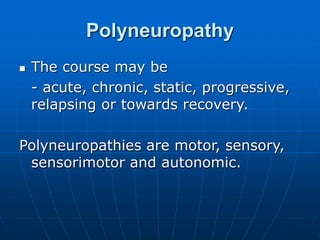
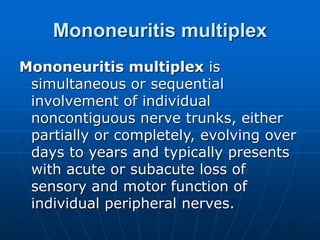
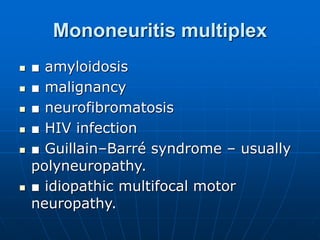
Peripheral neuropathy is damage to the peripheral nervous system, affecting nerves outside of the brain and spinal cord. It can be caused by diseases of the nerves themselves or systemic illness. There are several types including mononeuropathy (affecting a single nerve), mononeuritis multiplex (affecting multiple individual nerves), and polyneuropathy (affecting many nerves symmetrically). Common causes include diabetes, alcohol use, toxins, genetics, and metabolic conditions. Symptoms vary depending on the type and nerves involved but may include pain, numbness, tingling, muscle weakness and loss of sensation. Diagnosis involves clinical exams, nerve conduction tests, and identifying underlying causes. Treatment focuses on managing the cause, treating pain symptoms